Medical expert of the article
New publications
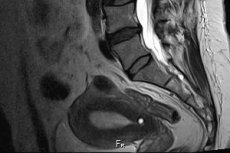
MRI of the sacrum and coccyx: how is the procedure performed?
Last reviewed: 06.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Physical examination and laboratory diagnostics cannot always provide the doctor with enough information about the patient's health, especially when it comes to pathological processes occurring inside the body. Externally, such diseases may not manifest themselves in any way. Tests only allow us to lift the curtain on what is happening in the body, but they are unlikely to provide complete information about spinal abnormalities, degenerative processes in it and adjacent tissues. Fluorography, which is usually aimed at identifying possible pulmonary tuberculosis and neoplasms in this area, despite the reduced image size, allows us to assess the condition of the thoracic spine. But for diagnosing pathologies of the lower spine, it is more appropriate to use X-ray diagnostics or relatively new and at the same time more informative methods. MRI of the sacral spine can confidently be called just such an innovative method.
Benefits of Magnetic Resonance Imaging
Since the end of the 19th century, humanity has been able to see the processes occurring inside a person on X-ray film. This was a breakthrough in medicine at that time, but later it turned out that such examination of a person is unsafe, so it cannot be carried out repeatedly. In addition, X-ray diagnostics. Easily detecting pathological processes in bones, did not always make it possible to accurately assess changes in soft tissues adjacent to bones (muscles, cartilage, ligaments).
This prompted scientists to further search for more informative and safe methods of diagnosing human health, and in 1971, finally, a description of an innovative method appeared that made it possible to obtain an image of human internal organs using a magnetic field and reflection processes in it (magnetic resonance). In fact, such a possibility was mentioned back in 1960, when the Soviet inventor V.A. Ivanov proposed his invention, which allows one to look inside material objects, and the phenomenon of nuclear magnetic resonance itself has been known to mankind since 1938.
Many decades passed from the moment of discovery of such a useful phenomenon to the realization of its possibilities and their introduction into the practice of medical research, until at the turn of the 19th and 20th centuries the MRI method entered the complex of diagnostic methods as one of the most informative and at the same time safe methods of examining the human body.
The basis of the innovative method is considered to be the phenomenon of nuclear magnetic resonance itself. In our body, every second atom is a hydrogen atom, which is capable of vibrating (resonating) if it is exposed to a magnetic field of sufficiently large, but safe for humans, force. In this case, energy is released, which is captured by the tomograph and converted into an image on the monitor screen using special programs. Thus, doctors have the opportunity to receive on the screen both a flat and a three-dimensional image of those organs and adjacent tissues in which the alleged failure occurred.
Like the long-used X-ray examination, magnetic resonance imaging is a painless, non-invasive method, i.e. it allows you to look inside the body without incisions and punctures, and the patient does not experience physical discomfort. But at the same time, unlike X-rays, you can undergo MRI several times a year without worrying about the consequences of irradiation of the body. MRI does not use light rays, it is based on the properties of hydrogen atoms to react to a magnetic field, and after the field stops, everything returns to normal.
A very important and useful property of magnetic resonance imaging is the ability to assess the condition of not only bone tissue, but also connective, cartilaginous, muscular tissue, including the spinal cord and blood vessels. Thus, MRI of the sacral spine makes it possible to see not only the violation of the integrity of the bones in this area, but also to assess the degenerative changes occurring in it, the presence of inflammatory processes or tumors, compression of the bone marrow and blood vessels, pinching of nerve fibers, which is often associated with pain syndrome.
Indications for the procedure
In order to understand for what diseases and symptoms a doctor may suggest an MRI of the sacral region, it would be useful to understand the structure of the lower spine. It is not at all necessary to delve into the scientific evidence base, but it is enough to recall the information from the school anatomy course.
The part of the spine below the rib cage includes 3 sections:
- lumbar, consisting of 5 separate vertebrae,
- sacral, which also has 5 vertebrae, the size of which decreases as they approach the coccyx (in adolescence, the sacral vertebrae fuse into one bone),
- coccygeal, which can consist of 4 to 5 small vertebrae (they also fuse together)
Of the 3 sections of the lower spine, only the lumbar section is mobile in adults. In children and adolescents, the sacral section also has some mobility, the vertebrae of which fuse only in adolescence. The coccyx is considered a vestigial organ that we inherited from our tailed ancestors and has lost its relevance over time.
The lumbar spine is the neighbor of the sacral spine from above, and the coccygeal spine is the neighbor of the coccygeal spine from below. Therefore, when pain or limited mobility of the spine appears in its lower part, it is often very difficult to say in which of the sections the cause of the pathological symptoms lies. The difficulties of visual diagnostics are resolved by prescribing a comprehensive examination of 2 sections at the same time: MRI of the lumbosacral or sacrococcygeal spine.
Doctors give a referral for MRI diagnostics of the lumbosacral region if they have:
- Suspected intervertebral herniation or protrusion of the vertebrae in the lumbosacral region as a result of damage to the fibrous ring.
- Suspected osteochondrosis of the lumbosacral spine is a degenerative disease characterized by the destruction of the intervertebral discs.
- The assumption that the cause of the malaise is stenosis of the spinal canal, or rather its lower segments, resulting in compression of the spinal cord and spinal nerve roots. With such a diagnosis, patients usually complain of pain in the back and legs, weakness in the lower limbs, impaired sensitivity in the lower limbs and pelvic area, cramps in the calf muscles, etc.
- There is reason to suspect tumor processes of the vertebrae and spinal cord in the lumbar and sacral region. Such diagnostics can also be performed with an established diagnosis to detect metastases in the vertebrae, spinal cord and pelvic organs.
- Suspected multiple sclerosis is an autoimmune disease with damage to the myelin sheaths of the nerve tissues of the brain and spinal cord, in which, along with memory loss, a complex of neurological symptoms is observed (increased tendon reflexes, weakness and muscle pain, dysfunction of the pelvic organs, up to urinary incontinence, etc.).
- Suspected development of syringomyelia - a chronic, progressive disease of the spine with the formation of cavities inside the spinal cord, resulting in a decrease or loss of pain and temperature sensitivity, weakness and a decrease in muscle volume, decreased sweating, and increased muscle fragility.
- Suspected inflammation of the spinal cord (myelitis) resulting from trauma, intoxication or infection. Characterized by decreased sensitivity of soft tissues and increased muscle tone, increased sweating, impaired urination and defecation, severe weakness in the limbs.
Instrumental diagnostics MRI may also be needed when symptoms of circulatory disorders in the lower extremities appear. They can be caused by vascular pathologies (phlebitis, varicose veins), as well as deforming changes in the spinal column, resulting in compression of the vessels, tumor processes.
In general, it can be said that MRI of the lumbosacral spine can be prescribed for any pain syndrome in the lumbar region, sacrum, sacroiliac joints, and stiffness of movement in this region. The same examination can be prescribed for impaired sensitivity in the pelvic and leg region associated with impaired blood flow and tissue innervation due to compression of nerve fibers and vessels by modified or displaced bones, cartilage, ligaments, and muscles.
MRI of the sacral or sacrococcygeal spine involves identifying pathological changes in the coccyx area, and in the area of the sacrum and sacroiliac joints, where multiple blood vessels and nerve roots pass, providing innervation of the pelvic area and lower limbs. Doctors prescribe such an examination for symptoms such as:
- pain syndrome in the gluteal muscles,
- forced posture due to pain in the coccyx or sacrum and limitation of the intervertebral joints,
- the appearance or increase of pain when pressing on the sacral area,
- pain in the coccyx area that intensifies during movement or sitting
- changes in sensitivity in the lower limbs.
The sacrum and coccyx in adults are immobile organs with fused vertebrae, so here we are talking about vertebral deformation rather than their displacement. In addition, the spinal cord in this part of the spine is presented in the form of a thin thread with a lower probability of damage than in other sections. Most pathologies of the sacrococcygeal region are traumatic in nature, less often we are talking about inflammatory-degenerative processes or oncological diseases. Nevertheless, it is sometimes quite difficult for doctors to make a diagnosis without relying on visual information about the internal structures of the body.
Thus, coccyx injuries, which usually occur when women fall with their buttocks on a hard surface or during childbirth, are very often immediately ignored by patients. But pain that intensifies during walking or pressure on the organ forces patients to seek help. At the same time, patients do not always even remember the old injury, but MRI images of the coccyx clearly indicate a fracture, dislocation or displacement of the vertebrae that occurred during a blow or strong pressure, with the formation of cicatricial-fibrous changes, which is the cause of prolonged pain.
But the reason may be different. Pain in the coccyx, for example, may be associated with pathologies of internal organs: proctitis, hemorrhoids, anal fissures, prostate pathologies in men, inflammatory diseases of the female reproductive system. And given that magnetic resonance imaging allows us to assess the condition of both bone (hard) and soft tissue structures, its value as a method of instrumental diagnostics that helps in differentiating diseases and diagnoses remains beyond doubt.
MRI diagnostics is used not only to detect pathological changes in organs, but also to detect congenital developmental anomalies that negatively affect the well-being of patients. True, in some cases they are detected by chance, which is also good for the prevention of possible health problems.
Some diseases and developmental anomalies can be treated or corrected surgically. In this case, MRI can be useful not only at the stage of preparation for surgery (its results give the doctor a clear understanding of the location of organs and deformed structures, help determine the localization and depth of incisions, the size of neoplasms and the spread of metastases), but also in the postoperative period. With the help of a simple and safe procedure, you can evaluate the quality of the operation performed and track the recovery process, during which corrective procedures may also be needed.
Preparation
MRI of the sacral spine is a fairly simple procedure. The results of the study are not affected by the food or medications consumed the day before, nor by physical or mental stress, nor by the physiological needs of the human body. In such conditions, doctors do not see any point in limiting patients in any way, i.e. special preparation for the procedure, as such, is not required.
It is clear that a person does not come to an MRI of the sacral, lumbosacral or coccygeal spine empty-handed and complaining about his health. First, he will have to contact a therapist, pediatrician or family doctor, who will either give a referral for examination after listening to the patient's complaints, studying the anamnesis and the results of a preliminary examination (for example, laboratory diagnostics), if such was prescribed, or refer the person for a consultation with a narrow specialist (traumatologist, neurologist, rheumatologist, orthopedist). But neither generalists nor highly specialized doctors will make a final diagnosis without an instrumental examination of the corresponding section (or sections) of the spine.
The referral issued by the doctors will be tenderly presented to the technician who conducts the magnetic resonance examination in a specialized room of the hospital or in the reception of a clinic specializing in such studies.
Certain requirements are imposed on the clothes and jewelry on the body of the person being examined. Immediately before the examination procedure, the patient is invited to a separate booth, where he will need to take off his outerwear, all items of clothing and jewelry containing metal components, leave behind regular and electronic keys, bank cards, small change, watches, etc. This applies to any items that can interact with the magnetic field, distorting information or causing harm to the patient's body.
In many clinics, patients are given special clothing, a gown for examination, or a sheet.
It is advisable for women to undergo the procedure without cosmetics and certain body care products (creams, antiperspirants, etc.), since some types of them may contain metal particles that interact with the magnetic field.
MRI of various parts of the spine can be performed both without and with contrast (most often, gadolinium salts, which are safe for humans, act as a contrast agent). In this case, the contrast is usually administered intravenously or intra-articularly. Contrast agents can rarely cause unpleasant symptoms in a mild form. They do not interact with various substances in the blood or intra-articular fluid, so preparation for MRI with contrast is no different from that for an examination without the use of a contrast agent, which improves the visibility of the structures being examined, which is especially valuable in diagnosing tumor processes and tumor metastases.
Regardless of whether the patient has had an MRI before or is coming for the first time, the technician performing the procedure explains how it will be performed, what requirements are imposed on the patient's behavior, and what options there are for communicating with the medical staff (the procedure is performed in a separate room, and the technician is in another room).
Technique MRI of the sacral spine
If a person has never had to undergo magnetic resonance imaging, naturally, he immediately has a question about how MRI of the lumbar, sacral and coccygeal spine is done. Even without special training, the procedure may seem frightening due to the large size of the MRI diagnostics unit itself.
Despite its large size, the MRI machine itself is generally harmless. To perform the procedure, the patient lies down on a special sliding table, which is then moved into the tomograph chamber, which resembles a large tube.
When lying down on the table, you need to take a comfortable position, while the patient's arms and legs can be additionally fixed with belts. This is necessary to maintain a motionless position during the examination, because any movement will affect the clarity of the resulting image, as a result of which it will be unsuitable for diagnosis.
During the operation of the tomograph, a specific sound (noisy tapping) is noted inside it, emanating from the operating magnetic field generator, which can irritate the examined. To make the person comfortable, they are given earplugs or special headphones for listening to music before the procedure.
Many people are frightened by the need for isolation during the examination, and those who suffer from claustrophobia (fear of enclosed spaces) may even experience panic. In case of phobia, the use of high doses of sedatives is indicated, other patients in case of unpleasant sensations or severe discomfort can always seek help from medical staff. The tomograph device provides for two-way communication with the doctor conducting the examination and located in the next room during the procedure. If necessary, the patient's relatives can also be there, especially if a child is being examined.
It should be said that unlike X-ray, which takes only a couple of minutes to perform, magnetic resonance imaging is a technique that takes much longer to perform. The patient must lie still while in the chamber of the device. The procedure without contrast takes about 20-30 minutes, and with the introduction of a contrast agent, 10 minutes longer, which is necessary for the contrast to penetrate the organ being examined.
To reduce anxiety and ensure the preservation of a static posture during the entire procedure, overly excitable patients and those who are afraid of the device are given sedatives. In the case of severe back pain that does not allow them to lie still for a long time, patients are offered painkillers before the procedure. If the procedure is prescribed to a child with back pain, the best option would be to administer light anesthesia or local anesthesia.
As we can see, the device for conducting MRI of the sacral spine and other human organs, as well as the examination methodology, are designed in such a way as to maximally protect patients, eliminate panic among them and, if possible, ensure their comfort.
 [ 4 ]
[ 4 ]
Contraindications to the procedure
Despite the fact that MRI of the sacral spine is considered an absolutely safe procedure, it has its contraindications. It should be noted that there are not so many absolute contraindications to the procedure. These include:
- Connection to portable devices that affect the heart rhythm (pacemakers), without which a person cannot be during the procedure. The magnetic field can affect the operation of the device and provoke an exacerbation of heart disease.
- The presence of ferromagnetic implants, various electronic devices introduced into the patient's body (again, due to the danger of interaction with the magnetic field)
- Elizarov devices used for severe bone integrity disorders.
- Ferromagnetic fragments in the body that can change their position under the influence of a magnetic field.
Metal hemostatic clips previously placed on the vessels will also be a reason for refusing to perform an MRI for the safety of the patient's health.
Relative contraindications include:
- The presence in the body or on its surface of metal fragments, metal-ceramic dental prostheses and crowns, tattoos, implants made of materials unknown to the patient, insulin pumps, nerve stimulators, prostheses that imitate heart valves.
- Claustrophobia, in which case the examination is recommended in open-circuit devices, in the presence of the patient's relatives and, if necessary, with the use of drugs that provide sedation or drug-induced sleep.
- Conditions in which a person cannot remain in a static position for a long time.
- Mental illnesses, especially in the acute stage, convulsive syndrome, inadequate patient condition (for example, alcohol intoxication, fever, etc.).
- Severe heart failure.
- Severe patient condition and conditions requiring constant monitoring of physiological systems.
- Severe renal and hepatic failure, hemolytic anemia, pregnancy (in case of contrast administration). Contrast agent is also not administered in case of hypersensitivity of the patient's body to it.
Pregnancy is not a direct contraindication to MRI of the sacral spine. However, many doctors do not recommend undergoing the procedure in the first trimester of pregnancy unless absolutely necessary. This is due to insufficient information about the effect of the magnetic field on the developing fetus.
Childhood is also not an obstacle to examination. MRI is prescribed even to infants. If necessary, even MRI with contrast is prescribed, accurately calculating safe doses of contrast agents depending on the age and weight of the child.
Normal performance
A useful and important feature of magnetic resonance imaging is the rapid receipt of examination results, which are either sent to the attending physician or given to the patient. The latter requires a subsequent visit to a specialist who will help correctly interpret the results of the study.
In the absence of spinal pathologies, MRI images show smooth vertebrae of the correct shape and size, intervertebral discs located in their place and having a standard height, joints without roughness and growths. The spinal cord is characterized by a clear structure, has no pathological distortions and neoplasms that are clearly visible when contrast is administered.
In some pathologies, you don’t even need to be a specialist to understand what an MRI scan of the sacral spine shows. Here are a few examples:
- in case of fractures, the fracture line will be clearly visible on the RT image, and the deformation of the bones or the displacement of their parts relative to each other can also be noted,
- if we are talking about a compression fracture, there will be no displacement, which means we are talking about the destruction of bones (a decrease in their strength, observed in osteoporosis) or the spread of tumor processes into bone structures (for example, metastases from a tumor diagnosed nearby),
- the tumors themselves are defined as separate light-colored spots (with contrast examination they acquire the color of the contrast) in the area of soft tissue or spinal cord,
- You can diagnose a spinal hernia if the image shows visible changes in the intervertebral discs: their displacement and protrusion, uneven height over the entire area of the disc or a decrease in the height of one of the intervertebral discs, rupture of the disc membrane (fibrous ring), narrowing of the spinal canal at the site of disc displacement.
- With osteochondrosis or weakness of the spinal muscles, a displacement of the vertebrae themselves is observed; in the first case, their deformation (flattening) may also be visible.
- On MRI images of the sacral spine, a cyst appears as a gray spot with clear edges and is often localized on the marginal segments of the coccyx.
- Stenosis of the spinal canal can be judged by the condition of the spinal cord, which is shown in the images as a light strip running inside the spine. Compressions and curvatures of the spinal cord are clearly visible against the background of surrounding darker areas. But protruding light areas may indicate the development of tumor processes.
Despite the amount of information that can be obtained by simply carefully examining the MRI images of the sacral spine, a specialist should decipher the results of the examination. This will help to avoid not only groundless panic due to incorrect interpretation of the MRI results, but also a dangerous delay in treatment if the patient ignores alarming symptoms and does not consult a doctor. The human brain has such a feature that allows us not to notice what we do not want to see and admit. So often we ignore serious diseases only because we do not want to admit that we have them and get treatment. But some diseases of the spine, if left untreated, are a direct path to disability.
Complications after the procedure
Doctors claim that the MRI procedure is absolutely safe if you take into account the above contraindications, do not hide the presence of electronic devices and ferromagnetic implants in the body, and most importantly, listen to the requirements and advice of doctors. Doctors create all the conditions so that the patient is as comfortable as possible during the procedure, starting from headphones with pleasant, relaxing music and ending with sedatives and painkillers.
In case of epilepsy and claustrophobia, the patient can undergo examination in an open-loop device, which helps to avoid complications of the existing nervous system disorder. The same examination can be offered to children. Relatives are allowed to be present at the procedure as support.
The most unpleasant consequence of an MRI procedure without contrast is blurry images if the person moved while in the magnetic field. This happens when the patient refuses the medications offered to help calm down or relieve pain, and also in cases where the patient did not bother to go to the toilet in advance or drank a lot of water the day before.
Side effects of MRI of the sacral spine are usually discussed in connection with the introduction of contrast. These substances, although considered safe, can cause allergic symptoms in some people (skin rash, tissue swelling, itching, hyperemia, etc.). Sometimes patients may complain of dizziness and headaches, but this usually happens during brain examination or if not all metal objects were left outside the room (for example, these could be ordinary metal buttons).
The occurrence of side effects may be caused by concealment of renal failure during examination with contrast. In this case, the contrast remains in the body longer and may cause deterioration of the patient's well-being.
The most dangerous complication usually occurs not after the procedure, but in cases where the patient ignores pathological symptoms, refuses to undergo examination, or delays going to the doctor for a long time, turning to him only when the treatment no longer gives positive results. This can become not only the cause of disability, but also the death of the patient (this is usually the case with oncology, if it is not treated at an early stage).
The disadvantage of magnetic resonance imaging is its high cost compared to radiography. But the harm from it is much less, given that the study itself is more informative and allows you to get a three-dimensional image of the organs.
Another positive aspect of MRI of the sacral spine or other sections or organs is the lack of need for special care after the examination. However, this is not a reason to give up on the results and not go to the doctor anymore if it suddenly seemed that everything was normal in the image, or to self-medicate, having independently diagnosed yourself based on the image. Only a specialist can correctly interpret the results of the examination and, if necessary, prescribe effective treatment. Care after the MRI procedure consists of further professional care for your health.

