Medical expert of the article
New publications
Intrauterine septum
Last reviewed: 29.06.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
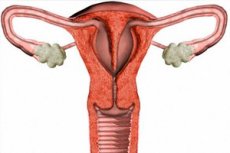
The intrauterine septum (or interuterine septum) is a structure inside the uterus that divides it into two cavities or parts. This septum may be present at birth (congenital abnormality) or formed during a woman's life (acquired).
An intrauterine septum can come in different sizes and shapes. In some cases it may be small and cause no symptoms or complications, while in other cases it may be larger and cause various problems such as:
- Infertility: An intrauterine septum can make it difficult for eggs and sperm to travel to the site of fertilization.
- Uterine bleeding: It can cause menstrual bleeding and menstrual pain.
- Pregnancy anomalies: Septum may increase the risk of miscarriages or complicated pregnancies.
- Other complications: In some cases, the septum may cause lower abdominal pain or lead to an increased risk of infections.
To diagnose and treat an intrauterine septum, women may see a gynecologist. An ultrasound and possibly a hysteroscopy (inserting an optical system through the cervix to view the internal structure) are usually performed to clarify the diagnosis. Treatment may include surgical removal of the septum if it is causing serious problems.
Causes of the intrauterine septum
Intrauterine septum can have different causes and its origin can be congenital or acquired. Here are some of the major causes of intrauterine septum:
- Congenitalanomaly: The most common cause of intrauterine septum is congenital anomaly of uterine development. It can result from abnormalities in the formation of the uterus during early embryonic development.
- Genetic factors: Somegenetic mutations or hereditary factors may increase the risk of developing an intrauterine septum.
- Trauma or surgery: Surg ical procedures such as abortions, cesarean sections, or other interventions in the uterus can sometimes result in a septum.
- Infections: Rarely, but infections that involve the uterus can cause the formation of an intrauterine septum.
- Hormonal factors: Certain hormonal disorders or imbalances of hormones in a woman's body can affect the development of the uterus and contribute to the formation of a septum.
- Intrauterine placentation: Certain conditions of intrauterine placentation, such as abnormal attachment of the placenta to the uterine wall, can affect septal formation.
- Medications and toxins: In rare cases, exposure of the fetus to certain medications or toxins may contribute to septal formation.
Symptoms of the intrauterine septum
This anomaly can be asymptomatic and undetected, but sometimes it can cause various symptoms and problems. Among the symptoms and complications of intrauterine septum may include:
- Abnormal menstruation: Patients with an intrauterine septum may experience irregular and painful menstruation. This is due to changes in the anatomy of the uterus, which can make it difficult for menses to drain.
- Pain and discomfort: Some women may experience lower abdominal pain or uterine cramps, especially during menstruation.
- Confirming pregnancy: An intrauterine septum can make it difficult to confirm a pregnancy because it can affect pregnancy test results.
- Uterinepregnancy complications: If an intrauterine septum is present, pregnancy complications such as neurodevelopmental fetal anomalies or fetal malposition may occur.
- Infertility: In some cases, an intrauterine septum may be associated with infertility.
- Increased risk of miscarriage: An intrauterine septum may increase the risk of preterm labor and miscarriage.
- Urethral problems: Sometimes the intrauterine septum can put pressure on the bladder or urethra, which can lead to urethral problems.
Forms
An intrauterine septum can be incomplete or complete depending on how it divides the uterus:
- Incomplete intrauterine septum: In this case, the septum does not reach the top of the uterus and does not separate it completely. This means that there is one common uterine cavity, but there is a partial separation within it. An incomplete septum can have different sizes and shapes.
- Complete intrauterine septum: In this case, the septum completely divides the uterus into two separate cavities. This creates two separate uteruses, each of which may have its own cervix. A complete septum is usually a more serious condition than an incomplete septum.
Both types of septum can be congenital or acquired. An incomplete septum is usually less problematic and may not cause symptoms. A complete septum can lead to serious problems such as infertility, miscarriage, complicated pregnancies, or other uterine conditions.
Complications and consequences
An intrauterine septum, especially a complete one, can cause a number of complications and consequences that can affect a woman's health. Here are some of the possible complications and consequences of an intrauterine septum:
- Infertility: A complete intrauterine septum can make conception difficult because it can interfere with the normal passage of the egg and sperm to the site of fertilization.
- Multiple pregnancies: A septum may increase the risk of multiple pregnancies, such as twins or twins, if one egg is fertilized in one uterine cavity and the other egg is fertilized in a second uterine cavity.
- Risk miscarriage: A septum may increase the risk of miscarriage or premature delivery in pregnancy, especially if it affects the area where the fetal egg is supposed to attach.
- Pain and menstrual irregularities: Women with an intrauterine septum may experience lower abdominal pain and unusual menstrual irregularities such as heavy bleeding and pain.
- Inability to perform an endometrial biopsy: A septum may make it difficult or impossible to perform an endometrial biopsy, which may be necessary to diagnose certain uterine diseases.
- Symptoms of pain and discomfort: An intrauterine septum can cause lower abdominal pain, especially during menstruation, and general discomfort.
Diagnostics of the intrauterine septum
Diagnosing an intrauterine septum (or septum) of the uterus may involve several methods and procedures to determine the presence and characteristics of this abnormality. Here are some of them:
- Gynecologic exam: Your doctor may examine you in a gynecologic chair and assess the condition of your uterus. They may notice an intrauterine septum on visual inspection.
- Ultrasound (USG): Ultrasound can be a useful method to determine the presence of an intrauterine septum and its characteristics. Ultrasound can be used to assess the size, thickness and shape of the septum.
- Hysterosalpingography (HSG): This is a radiologic study in which x-ray contrast is injected into the uterus and tubes. HSG can help visualize the septum and its shape.
- Magnetic resonance imaging (MRI): MRI can be used to visualize the uterus in more detail and to characterize the intrauterine septum.
- Laparoscopy: A laparoscopic surgical procedure can be performed for a more accurate diagnosis and at the same time to correct the intrauterine septum if necessary.
- Examination using contrast agents: Sometimes contrast agents may be injected into the uterus to better visualize the intrauterine septum by ultrasound or other methods.
Differential diagnosis
The differential diagnosis of intrauterine septum is to identify and distinguish this condition from other uterine abnormalities and diseases. Here are some conditions that may resemble an intrauterine septum and require differential diagnosis:
- The uterine cavity is separated by myoma (fibroids): Myomas are benign uterine tumors that can create intrauterine septa or change the shape of the uterus. Differentiating between intrauterine septum and myomas may require intrauterine ultrasound or hysteroscopy.
- Uterine polyps: Polyps are small growths inside the uterus. They can cause similar symptoms such as menstrual irregularities and pain. Hysteroscopy can help in the differential diagnosis between polyps and intrauterine septum.
- Uterine architectural abnormalities: Some women may have congenital uterine shape abnormalities such as a double-laced uterus (two uterine cavities), which may resemble an intrauterine septum. Medical imaging and hysteroscopy may be required for differential diagnosis.
- Endometriosis: Endometriosis is a condition in which tissue similar to the inner layer of the uterus grows outside the uterus. This condition can have symptoms similar to those of an intrauterine septum. Educational methods such as ultrasound and magnetic resonance imaging may be used for differential diagnosis.
Treatment of the intrauterine septum
Excision of the intrauterine septum (septum) in the uterus may be performed when there is a medical indication. This procedure is called a myomectomy or resection of the intrauterine septum. Here are some of the possible indications and basic steps of this procedure:
Indications:
- Infertility: An intrauterine septum can interfere with successful embryo implantation and lead to infertility.
- Abortions or recurrent miscarriages: Having a septum increases the risk of recurrent miscarriages or abortion complications.
- Menstrual disorders: Septum may causemenstrual cycle abnormalities and severe pain.
- Compression of other organs: In case the septum protrudes strongly into the uterine cavity, it can put pressure on neighboring organs, which can cause discomfort or pain.
Procedure Steps:
- Preparation: The patient undergoes a preliminary evaluation and preparation. This includes a physical examination and a number of laboratory tests.
- Anesthesia: The procedure can be performed under general anesthesia, spinal anesthesia or local anesthesia, depending on the complexity of the case and the doctor's decision.
- Septal excision: The doctor makes access to the uterus through the vagina using special instruments. The intrauterine septum is then removed or resected to restore the normal structure of the uterus.
- Recovery and follow-up: After the procedure, the patient may need some time to recover. The physician will monitor the patient and provide recommendations for care and recovery.
After the removal of an intrauterine septum, it is important to follow your doctor's recommendations and monitor your health. This procedure can be effective in treating medical problems related to the presence of a septum in the uterus.
Literature
Savelieva, G. M. Gynecology: national guide / edited by G. M. Savelieva, G. T. Sukhikh, V. N. Serov, V. E. Radzinsky, I. B. Manukhin. - 2nd ed. Moscow: GEOTAR-Media, 2022.

