Medical expert of the article
New publications
How to recognize streptoderma in adults and children: symptoms and stages of the disease
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Skin diseases are one of the most numerous groups of health disorders known to mankind. A wide variety of manifestations and causes, which are difficult for an uninformed person to understand, causes some confusion when we find strange spots, rashes, redness on our body, which may be accompanied by pain, burning, itching or not remind of themselves at all. After all, the skin is an external organ, and all symptoms of health disorders immediately become visible to the naked eye. For example, the external symptoms of streptoderma are not much different from most skin pathologies and are visible a week after infection. And this is actually in the absence of internal discomfort. So maybe you shouldn't worry about such a disease?
Skin diseases are evidence of an unhealthy body
The skin is considered the largest and most important organ of the human body, because it is the only protective shell of our body that protects internal organs and systems from the destructive effects of the environment. It is the skin that is primarily affected by the negative effects of thermal, chemical, mechanical and biological factors, so when making a diagnosis, doctors have to consider many skin pathologies in order to establish the truth by the method of exclusion.
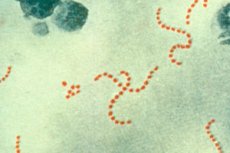
For example, many infectious skin diseases caused by biological factors have similar manifestations: rashes in the form of pustules or vesicles, more or less pronounced discomfort in the area of their localization. But a person who has taken the Hippocratic oath is not limited to just contemplating external symptoms, but will "dig" deeper, looking for moments that are characteristic of a certain disease.
It would seem, why go into detail if the main symptoms of streptoderma are right there, visible on the surface of the skin? In fact, this needs to be done to identify the pathogen (in this case, it is the streptococcus that has multiplied and become dangerous) and prevent it from penetrating deep into the body, causing the development of serious internal complications (rheumatism, myocarditis, glomerulonephritis, etc.) with seemingly safe first external signs of the disease. [ 1 ], [ 2 ]
In fact, diagnosing a disease based on external symptoms is not as simple as it may seem at first glance. Isn't that why most of the diagnoses we make for ourselves turn out to be incorrect? The fact is that the same streptoderma can manifest itself differently in different people. And here we must take into account the patient's age, the specifics of his work or other activities, concomitant diseases, the state of the immune system, etc.
Let's try to figure out what manifestations of streptoderma are typical for children and adults, in what places you can expect the appearance of a rash with this disease, transmitted by contact and contact-household means, what internal changes can indicate this disease.
Streptoderma in children
How does a child differ physiologically from us, adults? First of all, in their vulnerability to many infectious pathogens. A child's immunity is formed and strengthened for several years after birth, so small children suffer from infectious diseases much more often than adults, and the list of such diseases is replenished with purely childhood diseases. [ 3 ]
Streptoderma cannot be classified as a childhood disease, although the incidence among children is much higher than among young people and adults. This is also facilitated by the spread of the pathogen in large children's groups (nurseries, kindergartens, school groups, extracurricular groups, sports sections, art groups, etc.), where children and adolescents are in close contact with each other.
It is especially difficult to protect children under 3 years of age from troubles, for whom tactile sensations (to touch, to feel the properties of an object with their fingers) are especially attractive, allowing them to study the world in all its manifestations. And touching itself is very important at such a tender age. However, a young child does not yet have stable hygiene skills. In addition, the disease manifests itself outwardly much later than the ability to infect others arises, so when the first signs of streptoderma appear in one child, there is a high probability that by that time most of the group has already been infected.
Manifestations of the disease in children may differ depending on the degree of development of the immune system and the strength of immunity, the number of pathogenic microorganisms that have entered the skin, the presence of large and small skin lesions, the site of the disease, and the presence of concomitant pathologies.
In large children's groups, the disease develops according to the epidemic principle, i.e. a sick child quickly spreads infections throughout the entire children's group, and sometimes beyond. However, streptoderma will manifest itself differently in different children. If the child's immunity can withstand the onslaught of bacteria, the clinical picture will be limited to external signs: local rashes on the skin, i.e. damage to individual areas of the body. In this case, local immunity still plays a decisive role.
A rash, as a characteristic symptom of streptoderma, usually appears 2-10 days after infection in the form of bright pink papules or blisters with liquid, which after opening can turn into erosions. With appropriate care, such elements dry up quite quickly with the formation of crusts, which subsequently fall off painlessly.
However, in some forms of the disease, blisters do not form at all, limiting themselves to the formation of small pinkish or reddish lesions with peeling particles of the epidermis (dry form of streptoderma).
Itching with streptoderma is usually mild or absent, so it does not bother the child much. Another thing is that children tend to touch unusual elements on their skin with their fingers, scratch them simply out of childish curiosity and thus spread the infection to other parts of the body, complicating the course of the disease. [ 4 ]
But if the child's immunity is unable to cope with pathogens, and also if streptococci get on the delicate mucous membranes, more severe forms of the disease are likely to develop. In addition to external symptoms, the clinical picture of streptoderma in this case also has internal manifestations:
- An increase in body temperature to febrile values (above 38-38.5 degrees). The child may become lethargic, apathetic, his appetite worsens, and incomprehensible whims may appear. Other children, on the contrary, become overly excitable and the temperature is indicated only by the baby's unusually pink cheeks.
- The appearance of symptoms of intoxication of the body (the child may have a headache, hence lethargy and whims, nausea and vomiting may appear, not depending on food intake, appetite decreases, sleep is disturbed). In some cases, pain in the joints and muscles appears, which limits the child's mobility and causes tearfulness in babies and complaints about health in older children.
- Enlargement of the lymph nodes near the lesions along the lymph flow, which can sometimes be detected from the first days of the disease (lumps can be felt under the child’s skin, often painful when palpated).
- Blood tests of the child will show the presence of a pronounced inflammatory process characteristic of a bacterial infection.
Streptoderma in adults
The high incidence of streptoderma among children does not at all exclude the development of this disease in adults, because in infectious diseases, immunity plays a decisive role, not age. And it is worth mentioning that in the conditions of an ecological catastrophe in which most of us live, one cannot really count on strong immunity. According to a study conducted in 2005, at least 18.1 million people suffer from invasive diseases S. pyogenes, with another 1.78 million cases occurring each year. [ 5 ]
In addition, streptococcus penetrates the body through various, even microscopic, damages on the skin, so catching the disease is not as difficult as it seems. Another thing is that in people with more or less normal local and general immunity, it can proceed almost unnoticed, while a person weakened by chronic diseases can experience noticeable discomfort. [ 6 ]
An adult can become infected at work, while traveling on public transport, while visiting public places, including swimming pools and gyms. You can catch the infection even without leaving home if one of your relatives, for example, a child attending kindergarten or school, has become a source of infection. In this case, it is not necessary to have close contact with a sick person or a carrier of bacteria; you can also detect symptoms of streptoderma in yourself some time after skin contact with the patient's bed, clothes, household items, dishes, etc.
You can understand how streptoderma begins in adults, i.e. detect its first signs, by the appearance of the skin, on which, with this pathology, small pink, slightly raised above the body, painless spots are formed. A little later, slight itching and peeling appear on the surface of the pathological elements.
Then the papules, in most cases, begin to protrude more strongly above the skin and turn into small diameter bubbles, inside which a cloudy yellowish liquid can be seen. In the absence of treatment, individual closely located elements can merge into groups, covering large areas of the skin.
After some time, the blisters burst, forming cracks and ulcers, on the surface of which dry crusts or scales appear, reminiscent of lichen.
In the dry form of streptoderma, the rash has a slightly different character, blisters do not form in this case, and the foci of the disease have a whitish rather than pink tint due to the peeling that occurs. They are round in shape and up to five centimeters in size. Flaky scales of the epidermis form on them almost immediately, after which a weakly pigmented area of skin remains for a long time. Pathological foci are less likely to increase in size and spread to visible and hairy areas of the body than in other forms of the disease.
Complaints about itchy skin are not common when affected by streptococcal infection. Itching, if present, is insignificant and does not cause much discomfort, as is the case, for example, with chemical burns from alkali solutions, allergies or herpes, which have similar external manifestations to weeping forms of streptoderma.
The temperature with streptoderma in adults usually does not rise, unless the person is diagnosed with immunodeficiency, severe vitamin deficiency, or his body is greatly weakened by a long illness, excessive physical and mental stress, constant stress, which could not but affect the state of the immune system.
Enlargement of lymph nodes can be observed only when the infection spreads deep into the body. But this symptom usually appears already at the stage of possible complications, and not at the very beginning of the disease, as happens in children, whose skin barrier function is much weaker, which allows the infection to quickly penetrate into the deep layers of soft tissues and lymph.
With a mild course of the disease and appropriate treatment, the symptoms that appear disappear within 3-10 days without causing a deterioration in a person's health. But even with a severe form of streptoderma in adults, it is possible to cope quite quickly - within 3-7 days, if adequate treatment is prescribed and all its requirements are met. Only with a greatly weakened immune system or unsystematic implementation of therapeutic measures can the treatment be delayed up to 10-14 days with a certain probability of the transition of the acute form of the disease to a chronic one.
An important feature of streptoderma is the fact that even the usual daily hygiene of the body during the disease can do a disservice, because it is strictly not recommended to wet the affected areas with water, because this only delays the healing process.
Streptoderma in women and men
It is believed that women's skin is thinner and more delicate than men's, and it is logical that various wounds and scratches appear on it faster and more often, even with minor exposure to a damaging factor. Considering that streptococcus is considered a permanent resident of our skin, it can be assumed that women are more likely to get streptoderma than men.
In fact, the statistics of disease incidence in men and women do not differ much, because most representatives of the stronger sex work in conditions of increased risk of injury, and the hygienic conditions in many factories, plants, and public transport (and many work as drivers) are not up to par. In such conditions, the only protection against bacteria can be a strong immune system, which not everyone has.
In addition, both men and women have other specific factors that predispose to the development of streptococcal disease. These factors include diabetes mellitus, which comes in 2 types. Type 2 diabetes (insulin-independent) is more common in women, while insulin-dependent diabetes is more likely to affect men. And since this disease has a higher risk of developing long-healing wounds on the body, both sexes are equally likely to notice symptoms of streptoderma at some point. In addition, the disease is chronic in the vast majority of cases, just like diabetes itself.
In men, the likelihood of developing streptoderma increases during military service or imprisonment. This is facilitated by a large group, where the infection spreads in a short time, active physical activity that provokes increased sweating and the occurrence of prickly heat - foci where bacteria most easily penetrate the skin, insufficient hygiene, etc. Streptoderma in the army and prisons often has an acute epidemic nature.
It is believed that men are more likely to have symptoms of the dry form of streptoderma, i.e. small, oval-shaped, non-weeping, flaky lesions on the body, which, if left untreated, can spread to larger areas.
Women have an increased risk of developing streptoderma during pregnancy. This is not surprising, because hormonal changes in the body of the expectant mother are a blow to her immunity, which is exactly what bacteria need. Feeling a weakness, they immediately begin to actively multiply.
It is clear that streptoderma during pregnancy does not develop in all women, but only in those whose bodies experience an acute deficiency of vitamins and minerals necessary for the proper functioning of the immune system, or are exhausted by chronic diseases or stress.
Streptoderma does not develop very often during pregnancy, and it does not pose much of a danger to the expectant mother, as long as it only concerns external symptoms (slight itching and local rashes on the body), for which external use of antibiotics is quite acceptable.
True, many mothers, fearing to harm the baby in the womb, are in no hurry to resort to the help of potent drugs. And it is very in vain, because local application of antimicrobial drugs, in which their absorption into the blood is small, is almost impossible to harm the child. But in the absence of treatment, there is a risk that the fetus will also suffer. If microbes penetrate the placenta through the mother's blood to the baby, they will negatively affect the development of various organs and systems of the baby, especially if the mother falls ill in the 1st trimester of pregnancy, which most often happens. But it is in the first 3 months of fetal development that almost all the main vital systems of the future person are laid and formed.
As we can see, the chances of getting infected exist for representatives of different sexes and at certain moments of an individual's existence they can increase. At the same time, we do not always correctly interpret the symptoms that appear, so statistics cannot even approximately calculate how widespread this disease actually is, especially since the variety of forms of streptoderma and the peculiarities of its course predispose to a certain share of erroneous diagnoses.
Lesions: where to look for them?
Knowing that streptococcal infection is transmitted by contact and contact-household means, it can be assumed that the first symptoms of streptoderma appear mainly on the hands. In reality, specific rashes can be found on different parts of the body, namely, where there are micro- or macrodamages to the skin. In addition, after contact with the source of infection, a person can contribute to the spread of infection to other parts of the body.
The localization of lesions in streptoderma may vary, which to some extent affects the final diagnosis of the doctor. For example, streptoderma in the corners of the lips (angular cheilitis) may be diagnosed as "impetigo caused by streptococcal infection" or "streptococcal impetigo".
In most cases, streptoderma occurs on the arms and legs - the parts of the body that are more often than others open, not protected by clothing, less often on the feet, mainly in people with increased sweating of the feet, because this creates especially favorable conditions for the reproduction of pathogens (both bacteria and fungi). It is important to understand that various skin lesions are more likely on the extremities than, for example, on the back or buttocks. And if the skin also sweats (for example, on the feet), this makes it more vulnerable.
Oddly enough, but steptoderma on the face, as well as on the head, for example, behind the ears or on the lower part of the chin is not inferior in its prevalence. Not only children, but also adults tend to often touch their faces with their hands, not caring about their cleanliness. But the skin of the face is very delicate, so any friction or scratching can cause microdamage, and if a secret pest was hiding on the fingers or under the nails, then it is quite likely that it will settle in a new place, penetrating the skin in a suitable area.
There is a high risk of facial wounds and infection in those who shave (the vast majority of men and a small proportion of women), especially without using hygiene products, i.e. dry. And we remember that any wound on the body is attractive to infection because the body's protective barrier is broken in this place.
If the first signs of streptococcal infection appear on the skin near the hairline, there is a high risk that with improper treatment or its absence, the disease will develop into streptoderma of the scalp, spreading to the hair growth zone. In this case, a person's hair will have an accumulation of peeling skin particles (similar to dandruff), and the crusts after the ulcers dry up can fall off along with the hair follicles, causing local thinning.
The skin around the eyes is considered to be especially delicate and vulnerable, so foci of the disease are often found in this area, just rub the eyelid with a hand that comes into contact with the infection. Streptoderma of the eyelid is characterized by the appearance of pimples and blisters on the mucous membrane of the organ of vision or in the lateral folds around the eyes. At the same time, streptoderma on the eyelid is sometimes confused with a cold, herpes or barley, which in 90-95% of cases is caused by staphylococcus.
Streptoderma in the nose or ear is very similar to a herpes infection, but the itching occurs much later (with herpes, even before the rash appears), and it is much weaker in intensity. In addition, after the herpes elements open, there is practically no trace left on the soft tissues, while with streptoderma, cracks and ulcers remain in place of the blisters.
Streptoderma in the mouth, on the tongue, as well as situations when the rash reaches the throat, is a variant of bacterial stomatitis caused by streptococcal microflora. Our skin is a stronger barrier than mucous membranes, so it is not surprising that bacteria can more easily penetrate soft tissues through them. In addition, during eating and brushing teeth, the mucous membrane is often injured, and wounds on it, due to the increased humidity of the mouth, heal much longer than on the surface of the skin.
Streptoderma in the corners of the mouth, where microcracks often occur during wide opening of the mouth or active chewing, usually develops in children. This can be facilitated by eating with someone else's or an unwashed spoon with "living things" on it. Although in adults and adolescents (especially during hormonal changes) such situations also cannot be ruled out, although they occur with much less frequency.
Streptoderma on the lips (again, delicate skin that can be damaged even by the wind) can easily be confused with herpes, because the external symptoms of a viral infection and a bacterial disease are very similar. But again, it is worth paying attention to the itching, which is much stronger with herpes.
Any area with delicate skin and mucous membranes is more susceptible to various injuries, which means the probability of infection in these areas is higher. For example, do not be surprised if streptoderma is found in the groin. This is an area of skin with increased humidity, and therefore sensitivity to various negative effects. It is in such hidden areas, where it is warm and humid, that bacteria and fungi multiply with particular zeal, and the lesions increase at a faster rate, spreading to the perineum and anus.
The appearance of streptoderma symptoms on the mucous membranes is accompanied by noticeable pain, which intensifies when touching the inflamed elements. If the rash appears on the skin, it does not cause noticeable pain.
Thus, streptoderma on the genitals is not just an inconvenience, but a certain discomfort that affects the patient's quality of life. In addition, there is a high risk of infection spreading inside the body during sexual intercourse and during hygiene procedures.
Streptococcus constantly lives on the genitals, but when the immune defense is weakened, it can actively multiply, causing damage to the epidermal cells and tissue inflammation. But even with a fairly strong immune system, such a "gift" can be received from a sexual partner during sexual contact or intimate caresses, as well as streptoderma on the face when kissing.
Streptoderma under the arms develops for the same reason as in the groin, i.e. due to increased humidity and vulnerability of the skin in this area. In addition, many adults (mainly women) consider it indecent to have "vegetation" in this place, so they regularly shave their armpits. And shaving is a trauma to the skin, especially for its delicate areas. As a result, both small, invisible to the eye, and larger damages almost always remain on the skin, through which the infection subsequently penetrates.
But streptoderma on the back, stomach, chest or buttocks has other causes. It usually occurs after contact with contaminated bedding or clothing, less often after contact with the skin of a sick person (which is quite possible during the incubation period, when even the patient himself does not suspect his disease). It usually manifests itself in the form of a large number of separate red or pink small elements, initially reminiscent of a common acne rash, which subsequently turns into bubbles with cloudy contents and has a tendency to merge individual formations into larger foci.
The absence of pronounced itching and discomfort is the reason why patients are in no hurry to seek help until the infection has spread alarmingly or symptoms of a different nature appear.
Stages of streptoderma
Streptoderma is an infectious disease that can have different manifestations at different stages of its development. Thus, each stage of streptoderma development is characterized by its own specific symptoms.
At the first stage of its development, the disease has no external symptoms. This period is called the incubation period. It begins when the infection penetrates through damaged skin. Within 2-10 days, the bacteria become active and begin to multiply intensively. It is possible that the wound through which the infection penetrated may finally heal by the end of the incubation period and no manifestations of the disease will be visible on the skin.
At the second stage, small foci of hyperemia appear at the site of infection penetration, with subsequent formation of reddish seals (pustules). This indicates the development of an inflammatory process provoked by streptococcus bacteria. Already at this stage, some children begin to feel unwell, become lethargic, and get tired quickly. Adults, as a rule, do not feel unwell.
The third stage of the disease can be considered the transformation of the pustule into a blister with cloudy contents, which soon opens with the formation of ulcers and a yellowish-brown crust forms in its place. In some weeping forms of the disease, vesicles form almost immediately, and only then a red inflamed halo appears around them. All these are characteristic manifestations of the vital activity of beta-hemolytic streptococcus: the release of toxins and specific poisons.
With the dry form of streptoderma, blisters usually do not form at all. At the same time, the foci of infection are initially larger and very quickly become covered with whitish peeling crusts (the epidermis peels). This is a superficial form of the disease, which is quite easy to treat, and recovery usually occurs within 3-5 days.
At the last stage of the disease, the crusts dry up and fall off, leaving behind spots with a pink or bluish tint, which subsequently disappears. After dry streptoderma, as a rule, areas with weak pigmentation remain for a long time.
On average, 5-7 days pass from the appearance of a pathological element on the skin to the separation of the crusts. But it should be taken into account that not all elements appear at the same time, so the duration of treatment may be longer. In addition, careless scratching of pimples, bathing, palpation can cause the infection to spread to other parts of the body, and again it will take time for it to activate. Thus, new foci may appear when the first ones have barely a trace left.
If the process is not stopped, new elements of streptoderma will consistently appear in different places on the body, weakening the body's protective functions, and the disease threatens to become chronic. In this case, any decrease in immunity will be accompanied by the appearance of rashes on the body, and the person will become a virtually constant source of infection.
The symptoms of streptoderma are direct evidence that something is wrong with the body and that it is reducing its defenses. The disease itself is not life-threatening, but it is an alarming signal to take a closer look at your health and, first of all, strengthen your immune system.

