Medical expert of the article
New publications
Histoplasma is the causative agent of histoplasmosis
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Histoplasmosis is a natural focal deep mycosis characterized by predominant damage to the respiratory tract. A distinction is made between American (H. capsulatum) and African (H. duboisii) histoplasmosis, which is registered only on the African continent. The latter is characterized by lesions of the skin, subcutaneous tissue and bones in rural residents, as well as in people in contact with soil and dust. In addition to humans, baboons suffer from this mycosis in natural conditions.
The causative agents of histoplasmosis are Histoplasma capsulatum and H. duboisii.
Morphology of Histoplasma
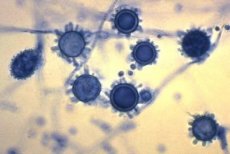
Dimorphic fungi. The mycelial phase is represented by septate mycelium 1-5 μm thick, spherical or pear-shaped microconidia 1-6 μm in diameter, and tuberculate macroconidia 10-25 μm in diameter. At 35-37 °C they grow as yeast cells, the size of which is 1.5-2x3-3.5 μm in H. capsulatum and 15-20 μm in H. duboisii.
Cultural properties of histoplasma
Colonies of yeast-like fungi are shiny, soft in consistency. Optimum growth temperature is 25-30 °C, pH 5.5-6.5, but growth is possible in wide pH ranges - 5.0-10.0. Biochemical activity is low.
Antigenic structure of histoplasma
It has common antigens with Blastomyces dermatitidis. It has an antigen of the yeast and mycelial (histoplasmin) phases. When grown on a liquid medium for 3 days, the mycelial form produces exoantigens h, m, which can be determined using immunodiffusion in a gel. Pathogenicity factors are microconidia, hydrolases, cell wall polysaccharides.
Ecological niche of Histoplasma
The natural habitat is soil. The fungus grows well in soil contaminated with bird and bat droppings, where it grows as a mytelium.
 [ 12 ], [ 13 ], [ 14 ], [ 15 ], [ 16 ], [ 17 ], [ 18 ], [ 19 ]
[ 12 ], [ 13 ], [ 14 ], [ 15 ], [ 16 ], [ 17 ], [ 18 ], [ 19 ]
Ecology
H. duhoisii has not been studied sufficiently; reports of the isolation of this species from soil are isolated.
 [ 20 ], [ 21 ], [ 22 ], [ 23 ]
[ 20 ], [ 21 ], [ 22 ], [ 23 ]
Sustainability in the environment
Microconidia are highly resistant in the external environment, remaining viable in dry soil for about 4 years, and in water at 4 °C for about 600 days.
Antibiotic sensitivity
Sensitive to amphotericin B and ketoconazole. Sensitive to antiseptics and disinfectants, Sensitive to the action of commonly used antiseptics and disinfectants.
Epidemiology of histoplasmosis
Histoplasmosis - sapronosis. The source of the infectious agent for humans and animals is the soil of endemic zones. Endemic zones are located in North, Central, South America, the Caribbean, South Africa, India, Southeast Asia, New Zealand and Australia. Sick people and animals are not infectious to others. The mechanism of transmission is aerogenic, the route of transmission is airborne and dusty. The susceptibility of the population is universal. In epidemic outbreaks, contact of patients with soil is detected. The epidemiology of African histoplasmosis has not been sufficiently studied.
Symptoms of Histoplasmosis
Symptoms of histoplasmosis depend on the immune status of the organism: acute forms are observed in children due to the peculiarities of their immune system, chronic disseminated forms, as a rule, develop against the background of insufficiency of the cellular link of immunity. Manifestations of histoplasmosis can vary from acute pulmonary infection, ending with spontaneous recovery, to chronic cavernous histoplasmosis and generalization of the infection.
Laboratory diagnostics of histoplasmosis
The material examined is pus from ulcerative lesions of the skin and mucous membranes, sputum, blood, urine, cerebrospinal fluid, punctures of bone marrow, spleen, liver, lymph nodes, and subcutaneous tissue.
Microscopic, mycological, biological, serological, allergological and histological methods are used for laboratory diagnostics. Work with the pathogen is carried out in laboratories of especially dangerous infections.
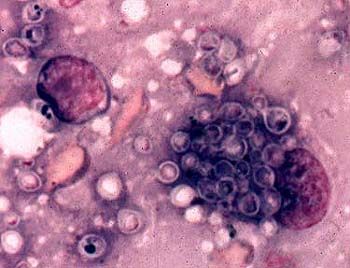
Microscopic examination of pus and exudate reveals histoplasms in hyperplastic cells of the mononuclear phagocyte system in the form of oval yeast-like cells measuring 10-15 μm, located extracellularly or inside monocytes and macrophages. Smears are stained according to Romanovsky-Giemsa.
To isolate a pure culture, the material to be studied is inoculated onto Sabouraud medium, serum or blood agar, and chicken embryos are also infected. Thiamine is added to the media to stimulate growth, and penicillin and streptomycin are added to suppress bacterial growth. Some of the inoculations are cultivated at 22-30 °C, and others at 37 °C for 3 weeks. The isolated culture is identified by morphological features and the results of a bioassay on mice. Detection of a two-phase fungus with a characteristic morphology of the mycelial phase (thin septate mycelium, microconidia and tuberculous macroconidia) and colonies consisting of small cells allows identification of H. capsulation.
Isolation of only the mycelial form of the fungus requires proof of its dimorphism. Transformation is achieved either by growing mycelial elements at 30-35 °C or by intraperitoneal infection of mice, which die in 2-6 weeks, and small yeasts are detected in the internal organs.
A pure culture is isolated by intraperitoneal infection of white mice or golden hamsters. After a month, the animals are killed, the crushed liver and spleen are seeded in Sabouraud's medium with glucose, and the pathogen is grown for 4 weeks at 25, 30, and 37 °C.
Isolation of culture in primary histoplasmosis is difficult due to minimal changes in the lungs, so in such cases one should rely on the results of serological reactions, of which the most effective are RP and RSK with histoplasmin, RP, immunodiffusion and latex agglutination are positive on the 2-5th week after infection. Later, a positive RSK is detected, the titers of which increase with generalization of the infection.
A positive intradermal test with histoplasmin (1:100) appears at an early stage of the disease and persists for many years. Only the transition of a previously negative reaction to a positive one has diagnostic value. The histoplasmin intradermal test can stimulate antibody genesis, so it is performed after serological studies.
For histological examination, the section preparations are stained with the Schiff reagent, but the Gomori-Grocott method gives the clearest results: yeast cells are stained black or brown. The pathogen can be found in the cytoplasm of lymphocytes, histiocytes in the form of small rounded single or budding cells.

