Medical expert of the article
New publications
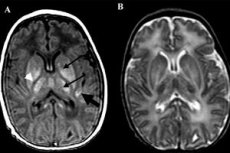
Cerebral hemodynamics and perinatal brain lesions
Last reviewed: 06.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Intracranial blood flow in the acute period of perinatal encephalopathy
Newborns with hypoxic-ischemic brain damage (cerebral ischemia) of I-II severity are generally characterized by the same patterns in changes in cerebral hemodynamics as healthy newborns, but with lower linear blood flow velocities (mostly diastolic). From the 3rd day of life, no reliable differences in linear velocities of cerebral blood flow were noted in healthy newborns and children with ischemia of II severity, which reflected the reversibility of the detected disorders, their "functional" nature. Normal echographic characteristics of the brain in neurosonography, as well as the absence of reliable differences in IR in healthy children and newborns with ischemia indicate the preservation of autoregulation of cerebral hemodynamics.
Analysis of cerebral hemodynamic parameters in grade III cerebral ischemia, accompanied by the formation of intracranial hemorrhages, demonstrates a significant decrease in all parameters characterizing blood flow in newborns.
The degree and rate of change in cerebral hemodynamics in various forms of hemorrhage are different. In newborns with grade I-II PVS, low velocities of both systolic and diastolic blood flow were noted, which was determined by high vascular resistance. This trend persists throughout the early neonatal period and is more typical for patients with grade II PVS. Blood pressure remains low during the first 2 days of life and fluctuates mainly within the range from 37.9 ± 1.91 to 44.2 ± 1.90 mm Hg. On the 3rd day of life, blood pressure rises to 56.0 ± 1.80 mm Hg, which is more often observed among patients with grade II PVS, accompanied by rapid progression of hemorrhage to grade III-IV PVS. In this case, the Dopplerogram often has a fluctuating character.
Thus, grades III-IV PVK most often develop against the background of severe arterial hypotension, which persists for the first 4-6 days of life. In cases with a fatal outcome, diastolic blood flow (after exclusion of the functioning arterial duct) is not determined in the first 6-8 hours of life. The fact of a decrease in blood flow rates in massive grade III PVK, especially diastolic, high IR of the cerebral arteries, and the fluctuating nature of blood flow are unfavorable prognostic signs - most of these children die. Stabilization of Dopplerogram indicators serves as a criterion for the effectiveness of the therapy.
Perinatal brain lesions mainly with ischemic focal lesions: periventricular and subcortical leukomalacia are characterized by a consistently high resistance of cerebral vessels throughout the early neonatal period. The maximum increase in IR occurs among patients with PVL. A drop in diastolic blood flow velocity indicates a decrease in intracranial blood flow and an increase in cerebral ischemia. Subsequently, IR decreases slightly. In children aged 3-4 weeks with increased periventricular echogenicity and small pseudocysts (cystic PVL stage), a high IR (0.8-0.9) is observed, which persists for a long time regardless of the treatment. Severe intracranial hypertension and high IR in these cases are extremely unfavorable prognostic signs reflecting the severity and irreversibility of brain damage.
In children with the phenomenon of "physiological" increased periventricular echogenicity (periventricular halo), mild hypoperfusion of the brain parenchyma and arterial hypotension are observed on days 1-4 of life. Starting from days 4-7, the arterial pressure in these newborns corresponds to similar indicators in healthy children and even, in some cases, exceeds their values, which does not change the level of cerebral blood flow. This is a convincing argument in favor of the preservation of the mechanisms of autoregulation of cerebral blood flow in the phenomenon of increased periventricular echogenicity and indicates the peculiarities of the blood supply to the periventricular region in children of this gestational age.
Based on the diagnostic and prognostic values of IR in the first day of life of a newborn, algorithms for the diagnosis and prognosis of hypoxic-ischemic brain damage are proposed. The most unfavorable prognostic sign is the absence of diastolic blood flow (IR = 1.0) in the first 6-8 hours of life (provided that a hemodynamically significant functioning arterial duct is excluded), which is accompanied by the development of an infarction or cerebral edema (less common) and is fatal in 80% of cases. IR values of 0.9 and higher in the first three days of life lead to the development of severe organic pathology of the brain in a child aged 1 year. The data obtained convincingly indicate that hypoperfusion of the brain parenchyma in the first day of a child's life, characterized by high IR values, is a prognostically more unfavorable sign of the outcome of perinatal encephalopathy at 1 year than hyperperfusion.
Intracranial blood flow in the recovery period of perinatal encephalopathy
In a comparative analysis of intracranial hemodynamics in children over 1 month of age and children who suffered chronic intrauterine or acute hypoxia during childbirth, with clinical manifestations of perinatal encephalopathy (PEP) in the recovery period (children over 1 month of age), it was noted that during the year in healthy children, IR in the PMA basin is stable and equals 0.66-0.7 in the first half of the year and 0.65-0.69 in the second half of the year.
In children with clinical syndromes of PEP, a phased change in IR indices in the anterior cerebral artery is observed during the first year of life:
- Phase 1 - "spasm" or tension - is characterized by an increase in IR in the ACA basin (over 0.7) and continues on average up to 3-4 months of life. Then there is a "negative turn" of IR from increased to decreased, i.e. from above 0.72 to less than 0.65.
- Phase 2 - relaxation of blood vessels - lasts up to 6-7 months in acute hypoxia and 8-11 months in chronic intrauterine hypoxia. IR is reduced.
- Phase 3 - the phase of recovery phenomena lasts until the age of 12-15 months, and possibly older. In this phase, we can judge the restoration of the tone of the vascular bed. IR returns to values of 0.65-0.69, which has significant prognostic value. Based on this phase, we can assume a persistent residual change in the regulation of the tone of the arterial vascular bed if IR remains reduced (less than 0.65). The phases of changes in arterial blood flow indicators during the first year of life in our work coincide with the clinical phases of the course of perinatal encephalopathy according to Yu.A. Barashnev.
The study of venous blood flow revealed that the venous outflow rate through the vein of Galen is significantly higher in children with hypertensive-hydrocephalic syndrome (HHS) than in children in the control group (p<0.01). A correlation is observed between the clinical picture of HHS and the appearance of pseudo-arterial venous outflow in the vein of Galen. When conducting a correlation analysis of venous outflow with other major neurological syndromes of the first year of life (syndrome of increased neuroreflex excitability, muscle dystonia syndrome, syndrome of vegetative-visceral dysfunctions, asthenoneurotic syndrome, delayed psychomotor development), no reliable relationship was found between these syndromes and the outflow rate through the vein of Galen or the nature of the venous curve. When comparing the rates of normalization of arterial blood flow and venous outflow indicators, it was found that venous outflow is restored significantly faster than arterial blood flow indicators (p<0.01).
Identification of a group of children with only vascular disorders (without structural brain damage in neurosonography) is important for clinicians. Correct interpretation of intracranial blood flow parameters in children of the first year of life in the norm and especially in combination with the clinical picture of perinatal brain damage allows for a more individual selection of corrective therapy aimed at eliminating vascular disorders and preventing structural changes in brain tissue. The use of Dopplerography allows one to answer the question of which link of intracranial blood flow is affected - arterial or venous, which determines the choice of drugs used in rehabilitation programs for children with perinatal CNS damage.
A comprehensive ultrasound examination using Dopplerography of intracranial arterial and venous vessels in young children significantly expands the possibilities of early topical diagnosis of vascular pathology, which is the cause of perinatal encephalopathy.


 [
[