Medical expert of the article
New publications
Focal pneumonia in children
Last reviewed: 05.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.

Pneumonia is an acute infectious disease. It manifests itself as a respiratory distress syndrome. Infiltrative changes are visible when performing an X-ray. Focal pneumonia is most common in children, it is characterized by an infectious and inflammatory lesion observed in a limited area of lung tissue.
ICD-10 code
Pneumonia is classified under the number J12- J18. According to the ICD 10 code, there are several forms of the disease. The first of them is community-acquired. It occurs at home or 48 hours after being in the hospital. Its course is favorable, fatal outcomes are extremely rare.
The second form according to the classification is hospital-acquired. It can develop 48 hours after the patient has been discharged from the hospital. This category includes patients with ventilator-associated pneumonia. This also includes victims with pneumonia who are kept in nursing homes. The mortality rate in this case is high.
The third form is aspiration pneumonia. It develops when a large amount of oropharyngeal contents is swallowed by an unconscious patient. This is due to swallowing disorders and a weakened cough. This category includes people with alcohol intoxication, traumatic brain injury, epilepsy, etc. A chemical burn cannot be ruled out when aspirating gastric contents.
Causes of focal pneumonia in children
The development of the disease is provoked by pneumococci and streptococci, as well as viruses, fungi and even physical and chemical factors. The main causes of focal pneumonia in children are rooted in a previously suffered disease. This can be provoked by both a common allergic reaction affecting the lungs and a complicated cold.
The mucous membrane of the child's respiratory tract is too sensitive. This is due to the large "content" of a large number of vessels in it. That is why pathogenic flora, penetrating into it, causes rapid edema. Thus, disrupting the ventilation of the lungs. It becomes difficult for the ciliated epithelium to remove phlegm from the lungs, this contributes to the creation of a favorable environment for the development of microorganisms.
Focal pneumonia is characterized by the presence of a single lesion. Its area is 1 cm, and this is only the minimum. Often, the problem arises against the background of chlamydia. Its main and most dangerous complication is pneumonia. All this indicates that any diseases, including respiratory tract lesions, must be eliminated in a timely manner.
Pathogenesis
In focal pneumonia, the inflammatory process is limited to a lobe or segment of the lung. Often, the foci that have arisen can merge with each other, thereby exacerbating the situation. With superficial localization, the pleura is gradually involved in the inflammatory process. The pathogenesis of focal pneumonia is not accompanied by immediate hypersensitivity. This feature does not allow the inflammatory process to flare up instantly. Here, everything happens gradually and rather slowly than with a violation of vascular permeability.
Escudant in pneumonia contains a small amount of fibrin. Most often it is serous or mucopurulent. This does not allow creating conditions for the release of red blood cells. Focal pneumonia always has the character of bronchopneumonia. This condition is characterized by an inflammatory process with damage to the mucous membrane of the bronchi. Thus, a significant amount of escudant is contained in the lumen of the airways. This condition provokes disorders of bronchial obstruction.
The disease has a number of distinctive pathogenetic features. Thus, the inflammatory process affects a small area, within one lobe or segment. Pneumonia is characterized by a normergic or hyperergic reaction of the body. Escudant is serous or mucopurulent. The lesion can also spread to the bronchi, causing their obstruction. The disease has no clear stages of development.
Symptoms of focal pneumonia in children
The main symptoms are catarrhal phenomena. The body is in a state of general intoxication. With focal pneumonia in children, certain symptoms occur, including radiological changes.
General intoxication syndrome may also occur with a number of other diseases. It is characterized by signs of toxicosis. The baby's behavior changes, apathy may be observed, or, on the contrary, increased excitability. Severe disorders of consciousness often occur, appetite decreases, vomiting and tachycardia appear. Vomiting occurs in extremely severe cases. Fever persists for more than 3 days. Catarrhal syndrome develops against the background of an acute respiratory infection. In 50% of all cases, it indicates the presence of pneumonia. It all starts with a cough, mostly wet.
Lung damage is a typical symptom of the disease. Shortness of breath does not always manifest itself, but wheezing is present. The presence of hematological shifts indicates the presence of focal lung damage. X-ray examinations are performed to confirm the diagnosis. Pneumonia is characterized by the presence of homogeneous shadows or inhomogeneous darkening.
First signs
You can determine the presence of pneumonia at home, without a doctor's examination. Thus, the condition is characterized by a lack of air. At the same time, the breathing rate begins to increase, and the skin turns blue. This condition is the first signs of the disease, it occurs against the background of damage to the alveoli and smooth muscles of the bronchial wall.
The baby becomes irritable, cries constantly. The body temperature is within 38-40 degrees. The presence of such symptoms requires immediate hospitalization. The child has decreased reflexes. Changes in the process of digestion of food, as well as weight loss are possible. The child may refuse food, he often vomits. This indicates the presence of pathological changes in the intestines, which can provoke respiratory diseases.
Cardiovascular pathology is often observed. It may be accompanied by a violation of blood supply in the pulmonary circulation. Clinical symptoms may intensify. The presence of the disease can be determined by the cyanosis of the skin, as well as swelling of the extremities. Against this background, heart rhythm disturbances develop. The baby may be overly active, or, on the contrary, lethargic. Refusal to eat, intestinal upset and vomiting are other signs of the disease.
Consequences
Focal pneumonia can lead to serious changes in the cardiovascular system. Tachycardia, widening of percussion boundaries and even muffled first heart sound at the apex are often observed. Some patients have darkening of medium or low intensity. In this case, their contours are disturbed. These consequences occur against the background of infiltration. But if the acini are affected, then the foci of inflammation may not be detected on the radiograph.
The lung shadow becomes significantly larger. Leukocytosis can be detected in the victim's blood. The number of leukocytes may be unchanged, even within the normal range, but there is pronounced leukopenia. The ESR indicator is increased.
Today, focal pneumonia does not pose a particular danger. It can be eliminated by means of modern effective antibiotic treatment. Antibacterial therapy gives a positive result and significantly reduces the risk of developing consequences.
Complications
Focal pneumonia is not capable of leading to the development of serious complications. Today, it is perfectly treatable. Thus, it is possible to eliminate not only the annoying symptoms, but also the disease as a whole. Modern antibacterial drugs really do wonders.
Despite such an optimistic prognosis, it is not worth completely excluding the possibility of consequences. Thus, the cardiovascular system may suffer first. Tachycardia may develop. The circulatory system may also suffer. What is most interesting is that the number of leukocytes remains within the normal range, but leukocytosis or leukopenia is still detected. The ESR indicator is elevated.
If you start timely treatment, it will be easy to get rid of symptoms and reduce the risk of further consequences. Focal pneumonia does not often cause a fatal outcome. There is no need to worry about this.
Diagnosis of focal pneumonia in children
The presence of the disease is recognized by cough and the presence of signs of acute respiratory infections; pneumonia is characterized by a high temperature that persists for more than 3 days. In this case, differentiation of the process is necessary. When diagnosing focal pneumonia, the doctor must examine the lower respiratory tract in children. The disease is characterized by the presence of a shortened percussion sound, difficulty breathing and wheezing.
At the second stage, pneumonia should be differentiated from bronchitis. It is characterized by rapid breathing, especially in cases where the lesion is extensive. This symptom is really significant if there are no signs of obstruction. During diagnostics, the specialist detects a shortening of the percussion sound. Small bubbling or crepitating wheezing can be noticed above the lesion.
When making a diagnosis, they rely on laboratory data. The presence of leukocytosis may indicate focal pneumonia. This condition is characterized by a certain leukocyte rate, fluctuating within the range below 10 109 / l. As for ESR, this indicator is equal to 30 mm / h, or significantly exceeds it. In some cases, C-reactive protein is prescribed for diagnosis. Its level should be more than 30 mg / l.
Tests
When making a diagnosis, doctors pay attention not only to external data. Laboratory tests and biochemical indicators play an important role. Laboratory blood test is taken from the finger. An increase in leukocytes or lymphocytes is typical for an inflammatory process in the body. The ESR indicator plays a special role; in a normal state, it should not exceed the norm.
An increased number of leukocytes indicates the presence of bacterial inflammation in the body. With severe intoxication, an increase in rod-shaped forms is observed. Lymphocytes are capable of producing antibodies, the main purpose of which is to destroy viruses.
Changes in the body can be noticed by the ESR indicator. It determines the level of the erythrocyte column at the bottom of the capillary. It is formed within an hour due to sedimentation. Normally, the speed is 1-15 mm per hour. In pneumonia, the indicator can increase several times and be 50 mm / hour. ESR is the main marker of the course of the pathology.
Biochemical analyses allow us to assess the impact of the pathological process on other organs and systems of the body. An increase in uric acid levels indicates problems with the kidneys. An increase in liver enzymes indicates the destruction of hepatocytes.
Instrumental diagnostics
Carrying out diagnostic measures implies specifying the nature and specificity of the pathogen, as well as the severity of the inflammatory process. Instrumental diagnostics, using special techniques, helps to cope with this task.
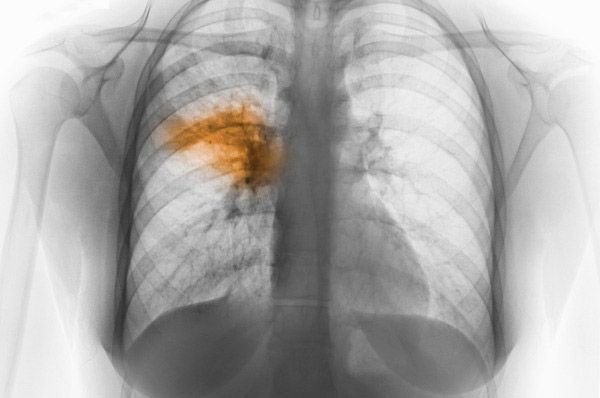
The most important method in this case is an X-ray examination of the chest organs. In the presence of focal lesions, the image clearly shows types of darkening or shadow. No less effective way to diagnose the disease is computed tomography. Thanks to it, it becomes possible to detect infiltration of the lung tissue. As for bronchography, it makes it possible to detect decay cavities. Often resort to the help of a radionuclide study of pulmonary blood flow.
It is impossible to make a diagnosis solely based on instrumental examinations. For a complete picture, it is necessary to obtain laboratory examination results. The doctor decides which instrumental methods to use.
Differential diagnostics
The first step is to examine the patient. Pneumonia is characterized by a high temperature, within 38 degrees, chills and general weakness. At this stage, differential diagnostics are used, because it is necessary to identify changes occurring in the circulatory system. A blood test allows you to notice pronounced leukocytosis. In addition to blood, sputum is also examined, this will help to determine the causative agent of the disease.
Other "raw materials" are not submitted for examination. At least, at the stage of disease detection, there is no need for this. Over time, urine is submitted for examination. A high level of acid in it indicates the spread of the inflammatory process. Most likely, the kidneys are affected. The diagnosis is made on the basis of the combined data of differential and instrumental studies. This will allow you to notice all the nuances and prescribe effective treatment that will prevent the development of complications.
Who to contact?
Treatment of focal pneumonia in children
First of all, the child must be hospitalized, the disease cannot be eliminated on its own. When the diagnosis has been accurately made, erythropic therapy begins. In case of some doubts, before starting focal therapy in a child, an X-ray should be taken.
Today, the disease is eliminated by means of antibiotics of the penicillin series. Together with them, enzyme inhibitors are often used. Such drugs as Augmentin and Timentin have proven their effectiveness in this case.
At home, you need to provide the child with normal care. In addition to medications, you need to eat right and establish a drinking regime. The diet should consist of light dishes and products. Preference is given to beef, vegetables, fruits and lean chicken. Drinking regime plays a special role. Fever can lead to dehydration. A large amount of liquid allows you to remove phlegm from the body. Children should drink 3 liters of water, giving preference to alkaline mineral water, fruit juices and milk.
It is necessary to observe bed rest. It is important that the baby's bed linen and underwear are always clean. After all, when the baby has a fever, we sweat a lot. The room temperature should not exceed 20 degrees. The room should be ventilated, but at the same time, do not create drafts.
Infants should be given 150 ml of liquid per kilogram of weight per day. If the baby is breastfed, the mother should monitor the amount of liquid consumed. In a hospital setting, the missing amount of liquid is administered intravenously.
Medicines
Drug treatment involves the use of antibacterial therapy. Antibiotics are prescribed immediately after diagnosis. When conducting antibacterial therapy, the duration of the drug in the body should be taken into account. At the beginning of treatment, preference is given to broad-spectrum antibiotics. Most often, Ampicillin, Levomycetin and Tetracycline are prescribed. If pneumonia was caused by Pseudomonas aeruginosa, preference is given to Nizoral, Nystatin and Metronidazole.
- Ampicillin. The drug is taken orally, regardless of food intake. A single dose is 0.5 grams. The maximum dosage should not exceed 3 grams. Children under 3 years of age should not take the drug. Allergic reactions, nausea, diarrhea and stomatitis are possible.
- Levomycetin. The drug is used 30 minutes before meals. Dosage - 0.5 grams, maximum - 3 grams. The drug should not be taken in case of skin diseases, as well as by newborns. Side effects: dyspeptic phenomena, hallucinations.
- Tetracycline. The drug is used 4 times a day, one tablet at a time. It is advisable to do this 30-60 minutes before meals. Contraindications: children under 8 years of age, hypersensitivity. Allergic reactions may develop.
- Nizoral. The drug is used once a day. The duration of treatment depends on the patient's condition. People with severe liver and kidney dysfunction are prohibited from using it. It can lead to dyspeptic symptoms.
- Nystatin. The drug is used regardless of food intake. The dose is prescribed individually, the treatment period does not exceed 10 days. The drug cannot be used in case of hypersensitivity. Negative reactions from the body, in the form of allergies and dyspeptic phenomena, are not excluded.
- Metronidazole. The drug can be taken both in the form of tablets and suppositories. The daily dose does not exceed 2 tablets per day. Suppositories are inserted rectally at night for 10 days. The drug cannot be used in case of hypersensitivity. It can cause a number of side effects, including a metallic taste in the mouth, nausea, general malaise.
The broad-spectrum antibiotics used include: Cefamandole, Mezlocillin and Tobromycin. The duration of treatment should not exceed 15 days.
- Cefamandole. The drug is administered intravenously or intramuscularly. 50-100 mg per kilogram of weight is sufficient. The dose is selected by the attending physician. The drug cannot be used by newborns. Nausea, vomiting, and skin rash may develop.
- Mezlocillin. The drug is prescribed at a dose of 75 mg per kilogram of weight. The drug can be used even by newborns, but with special caution. People with increased sensitivity to the components of the drugs are at risk. The development of dyspeptic phenomena and allergies is not excluded.
- Tobromycin. Before use, it is necessary to conduct a sensitivity test. The dose is prescribed strictly on an individual basis. It is highly recommended not to use the drug in case of hypersensitivity. Headache, nausea, general lethargy may occur.
These are far from all the drugs that are used in the treatment of focal pneumonia. The most common options were presented above. How to conduct treatment and help, what medications to resort to, the attending physician decides.
Folk remedies
Traditional medicine is famous for its large number of effective recipes. All of them allow you to eliminate the disease without harming the body. But when using traditional medicine, one fact should be taken into account: it is not recommended to use it without the knowledge of a doctor. Medicinal herbs are not always able to help as well as a quality antibiotic.
The child is recommended to drink a hot infusion of violet grass. It is advisable to use lemongrass tincture, 2 times a day, 30 drops. The most favorable time for this is morning and afternoon. Ordinary olive oil can also help, the main thing is that it is at room temperature. Oatmeal with butter and honey will help to cope with the disease, the main thing is that it is very liquid.
It is recommended to take a decoction of aloe leaves with honey 3 times a day. It is easy to prepare the remedy, just cut an aloe leaf and mix it with 300 grams of honey. All this is mixed together with half a glass of water and boiled on low heat for 2 hours.
 [ 26 ], [ 27 ], [ 28 ], [ 29 ]
[ 26 ], [ 27 ], [ 28 ], [ 29 ]
Herbal treatment
To prepare effective remedies, it is enough to simply acquire medicinal herbs. Traditional methods of treatment have been used for a long time. Thanks to them, any disease can be eliminated, but before choosing herbal treatment, it is worth consulting a doctor.
- Recipe #1. Take equal parts of lungwort, centaury, sage, wormwood, and plantain. Grind all ingredients and pour one and a half liters of boiling water over them. Infuse the remedy overnight and strain in the morning. Drink 2-3 times a day until complete recovery.
- Recipe #2. Take equal amounts of thyme, knotweed, dill, anise, licorice root and pine buds. Grind all ingredients thoroughly and pour half a liter of boiling water over them. Leave the remedy to infuse overnight and strain in the morning. Take it 2-3 times a day until complete recovery.
- Recipe #3. Take birch leaves or buds, St. John's wort, eucalyptus, string, motherwort and sweet clover. Dilute all this with marshmallow, elecampane, bluebottle and angelica roots. Mullein flowers are added to the whole bouquet. All ingredients must be ground in a coffee grinder and poured with half a liter of boiling water. The remedy is infused overnight, then ground and used up to 3 times a day.
Homeopathy
Homeopathic remedies have proven themselves since ancient times. However, they cannot help everyone. The fact is that they are based on natural components. It is important that a person does not have an allergy to certain components. Otherwise, homeopathy will cause harm.
There are certain medications that help fight inflammatory processes in the respiratory tract, including pneumonia. Improvements from taking these medications are observed already on the second day. If this does not happen, it is worth giving preference to another drug.
Arsenicum album. This remedy has a pronounced effect in right-sided pneumonia. Antimonium tartaricum. It is used when mucus appears, as well as a gurgling sound from the chest. Bryonia alba. It is used for high temperature, as well as chest pain. Kali carbonicum. It is used during an exacerbation, when the baby is very shivery, and his eyelids are swollen. Lycopodium. It helps well with right-sided pneumonia. Phosphorus. It is used for chest heaviness, especially when the pain appears when the baby lies on the left side. Pulsatilla. It helps to cope with the inflammatory process and calms the child. Sulphur is used for burning in the lungs.
It is highly discouraged to take homeopathic remedies on your own. This should only be done under the guidance of an experienced specialist in this field.
Surgical treatment
Surgical intervention is used extremely rarely. It is indicated for certain categories of victims. Thus, surgical treatment is widely used only if complications have begun or there is a risk of their development.
In some cases, conservative therapy shows its ineffectiveness. This happens with an adequate degree of activity. This phenomenon is possible with the prevalence of the process, as well as its duration of at least one year. The lesion can go beyond the lung, and this requires surgical correction. At the age of over 7 years, as well as with the development of complications, surgical intervention is the only chance to overcome the disease.
Surgical intervention has its contraindications. Thus, it cannot be used in case of an extensive bilateral process that arose against the background of genetically determined hereditary diseases. Systemic diseases are also among the contraindications.
Prevention
Preventive measures include hardening. The baby should be accustomed to air baths and wet rubdowns from an early age. This will help strengthen the immune system. Thus, the child will have an increased ability to resist bacteria, viruses and colds. Therefore, prevention from an early age is very important.
In most cases, focal pneumonia develops against the background of influenza. Therefore, the first preventive action is timely elimination of the disease. Do not neglect methods for strengthening the child's immunity.
If the baby suffers from protracted diseases, it is necessary to prevent the development of hypostases. The child should turn over more often while lying down. Timely elimination of cardiovascular diseases will help to avoid possible consequences. Finally, the child should be taught not to inhale air through the mouth. This should be excluded in winter and autumn. The respiratory tract can be slightly covered with a scarf. It is advisable to move slowly, so as not to provoke an acceleration of the breathing rhythm.
Forecast
If the child received timely antibacterial therapy, the further course of the disease will be favorable. After discharge, the child should be registered with a dispensary. This will prevent the development of a relapse. After discharge from the hospital, the child should not visit children's institutions. After all, his body is weakened and there is a risk of re-infection. If you follow these rules, the prognosis will be purely positive.
The rehabilitation period should not be ignored. It is advisable to spend it in special hospital departments or sanatoriums. Daily breathing exercises will be useful. As for nutrition, it is important that it is rational. Rehabilitation with medications should be carried out according to individual indications.
Physiotherapy is widely used. The child should be given mustard plasters, ozokerite applications on the chest. Chest massage is performed. If all recommendations are followed strictly, the prognosis will be exclusively positive.
 [ 30 ]
[ 30 ]
Использованная литература

