Medical expert of the article
New publications
Rectal fistula
Last reviewed: 05.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.

A fistula of the rectum develops as a consequence of an acute purulent process in the tissue surrounding the anus - acute paraproctitis. A superficial fistula of the rectum is treated fairly quickly due to the fact that it passes close to the superficial skin. Transphincteric, deeper fistulas are more difficult to treat, since they are located parallel to the rectum in the deep layers of tissue.
The rectum, in turn, is also a passage, the final rectal zone of the digestive system. Rectum, as an excretory canal, has a length from the sigmoid colon to the anus. The length of the rectum varies from 15 to 18-20 centimeters, the diameter of the rectum depends on the functional sector: its initial part reaches 4 centimeters, in the middle the rectum can be up to 7.5-8 centimeters in diameter. The rectum differs from other parts of the intestine in that it has no bends and turns, in fact, it received its name from its direct direction. The uppermost zone of the rectum - the ampulla, is located in the sacrum, the narrowest, lower part is called canalis analis - anus, it is in this zone that paraproctitis (rectal abscess) most often develops, often ending in the formation of a fistula - a fistula.
Causes of rectal fistula
Clinicians call paraproctitis and proctitis the main cause of fistula formation in the rectum. Proctitis is an infection of the rectal canal wall itself - the rectum, and paraproctitis is an infection of the tissue that surrounds the rectum. When the infection penetrates the rectum tissue, an abscess is formed, which is subsequently drained. After opening the perianal abscess, a pathological tract is formed.
Granulomatous regional enteritis or Crohn's disease can also be the cause of the formation of a rectal fistula.
The factor that provokes internal fistulas of the rectum may be hernial inflammatory protrusions of the walls of the rectum.
Fistula of the rectum can have tuberculous etiology. Mycobacteria provoke the formation of granulomas in the intestine, then the process moves to the lower parts of the digestive tract - to the rectum. Tuberculosis of the rectum is quite rare and is a secondary disease following pulmonary tuberculosis.
Chlamydia can also provoke the development of abscesses and then fistulas in the rectum.
The oncologic process of the rectum is often accompanied by fistulas. Often, it is the recurrence of the fistula of the rectum that is the primary symptom of the pathological process and the reason for a comprehensive examination.
HIV and AIDS, syphilis are diseases that can also be accompanied by the formation of fistulas of the rectum.
How does a rectal fistula develop?
Fistula of the rectum is also called CP – chronic paraproctitis, since the fistula appears as a result of acute paraproctitis – an inflammatory process in the fatty tissue surrounding the anus. If the tissues surrounding the rectum are inflamed, damaged, infected and suppurate, a fistula of the rectum develops – a pathological passage between the intestine itself and the skin around the anus. Fistula of the rectum can be detected in both men and women, less often in children. Men suffer from chronic paraproctitis much more often than women. Removal of fistula of the rectum is often independent, spontaneous, when the abscess opens, and its contents are excreted with feces. This is a false “victory”, since the inflammation in the anal crypts (sinuses) remains, therefore, constant infection of the tissue continues. All cases of spontaneous abscess ruptures and discharge of contents to the outside are accompanied by the formation of a fistula with the preserved inflamed internal zone (in the crypt). Thus, a relapse of a fistula of the rectum lasts for a very long time, and chronic paraproctitis can haunt a person for many years, as long as the inflammation exists, that is, the root cause of the disease.
Fistula of the rectum is divided into the following types:
- Complete fistulas.
- Incomplete fistulas.
- Internal fistulas of the rectum.
Complete fistulas are a passage with two openings, one of them is internal, which is localized in the crypt (sinus) of the anus and goes out into the lumen of the rectum, the second one goes out onto the skin surface near the anus. A complete fistula can have many openings that are combined inside the layer into one passage ending on the skin surface.
An incomplete internal fistula of the rectum is a passage with an internal opening that opens onto the mucous surface. It is believed that an incomplete internal fistula of the rectum is a stage in the formation of a full-fledged fistula, followed by the inevitable process of tissue melting and the formation of an external opening.
Internal rectal fistulas are passages in which two openings are located directly in the wall of the rectum.
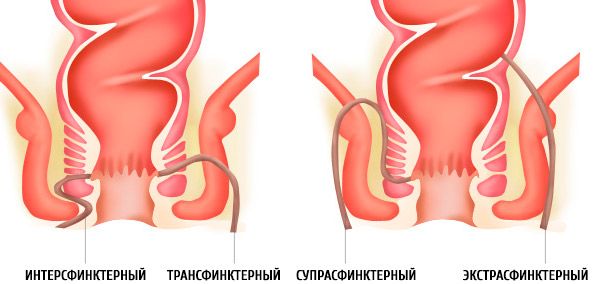
Fistulas are also distributed according to the location of the internal outlet and are systematized according to localization relative to the anus and can be as follows:
- On exit:
- Fistula of anterior localization.
- Fistula of the rectum of posterior localization.
- Lateral fistula.
- By localization:
- Intrasphincteric fistula of the rectum.
- Transsphincteric fistula.
- Extrasphincteric fistula of the rectum (high fistula).
Intrasphincteric fistula of the rectum is a passage that is localized along the edges of the anus in the subcutaneous-mucous layers. Such fistulas are characterized by a straight channel with an external opening directly near the anal sphincter. The internal opening goes into one of the anal crypts. Intrasphincteric fistula of the rectum is diagnosed in 30-35% of all patients suffering from proctological problems. In 100% of patients with anal fistulas, the history of the disease shows that the fistula of the rectum is recurrent.
Transsphincteric fistulas are characterized by the location of the channel in the subcutaneous or superficial layer, less often in the deep layers of the sphincter. The passages are usually multiple, with purulent pockets, accompanied by scarring of the surrounding tissues. Transsphincteric are also called transsphincteric fistulas, they are a typical clinical form of chronic neglected paraproctitis.
External or extrasphincteric fistulas seem to bypass, envelop the anus, folding the internal outlet into crypts. This type of fistula is a typical consequence of acute paraproctitis, which has several degrees of complexity:
- Narrow opening inside, straight passage, fistula without scars and infiltrates, without pus.
- The internal opening heals without inflammation or pus.
- The internal opening is not scarred because a purulent process is developing in the tissue.
- The hole inside expands, becomes scarred, has infiltrates, and purulent “pockets”.
Fistulas of the rectum: symptoms
A fistula cannot be asymptomatic, since the patient, as a rule, already has a proctological history of the disease; a fistula of the rectum is only a consequence of it.
The fistula tract begins to bother the patient with itching, discharge containing purulent ichor. Self-treatment of the fistula with folk remedies at this stage only worsens the patient's condition, severe irritation in the anus area appears, pain, and body temperature may increase. The disease progresses in waves, remission is possible, and then a relapse of the fistula of the rectum.
 [ 5 ]
[ 5 ]
Chronic form of paraproctitis
The fistula looks like a small wound with seals at the edges. In chronic cases, serous-purulent discharge is scanty but constant. It has a characteristic unpleasant odor and is irritating to the tissues of the anus. If there is insufficient drainage, pus begins to accumulate in the fistula passage, aching pain appears, which intensifies during defecation. After defecation, the pain subsides, and the outflow of exudate from the fistula is activated.
Aggravation of the process
During exacerbation and formation of an abscess in the tissue, the temperature rises, the pain becomes intense, radiating to the pelvic area, to the lower abdominal part of the body, to the rectum. Stool and urination are disturbed, swelling appears, most often in the legs. Improvement is possible from the moment the abscess opens, when the inflammation subsides, however, after some time, a relapse of the fistula of the rectum is possible.
Fistula of the rectum: treatment
Fistula of the rectum is directly related to the presence of infection and the conditions of its spread in the rectum. Therefore, the operation mainly neutralizes the fistula of the rectum. During the surgical intervention, both the fistula (fistula) and the inflamed anal crypt, which is a constant source of infection of the surrounding tissues, are removed. Thus, if chronic paraproctitis is confirmed, the fistula shows characteristic symptoms and signs, removal of the fistula of the rectum is inevitable. In the presence of serious contraindications, excision of the fistula of the rectum is postponed until the condition improves, and is carried out on a planned basis.
How to treat a fistula of the rectum is a question that worries the patient, but not an experienced proctologist. There is a standard scheme of surgical intervention for chronic paraproctitis. The duration of radical surgery depends on the clinical course of the disease. If the process is in the acute stage, there are infiltrates, abscesses, they are opened, the inflammation is eliminated with the help of conservative antibacterial therapy, both internal and external, and then the fistula of the rectum is excised. They usually try not to postpone the operation for a long time, since a relapse of the fistula of the rectum is possible, and a new exacerbation can provoke the formation of scars on the walls of the anus. The operation is postponed only in the case of persistent remission, when the fistula openings are closed.
Types of operations for rectal fistula:
- The fistula is dissected into the lumen of the rectum. This type of surgery, despite all its advantages, has significant disadvantages: the wound above the fistula may heal too quickly, and the external part of the sphincter may be damaged during surgery.
- Gabriel's operation is an excision of a fistula of the rectum. The operation consists of the following actions: a special solution is introduced into the fistula, a probe is passed through the fistula, after which the fistula is cut off, and the channel itself is removed. The skin covering the fistula and all tissues affected by inflammation are also excised.
- Excision of the rectal fistula with subsequent drainage.
- Excision of the fistula with subsequent suturing of the sphincter.
- Excision of a fistula using the ligature technique (for high, extrasphincteric fistulas). The ligature (thread) is inserted using a Bilroth clamp, grasped with another clamp and brought out of the intestine.
- Excision of a rectal fistula using a plastic method: the fistula tract is excised, purulent leaks are drained, the tissue is anesthetized and a flap of mucomuscular tissue is cut off, moved, closing the fistula opening.
The prognosis for surgical treatment of fistulas is favorable; as a rule, operations lead not only to stable remission, but also to complete recovery.
Fistula of the rectum after surgery
How to treat a fistula of the rectum after surgery. Fistula of the rectum how to treat after surgery must be under the supervision of a doctor, at least for one or two days. The patient is prescribed conservative treatment, which includes taking painkillers (especially before defecation) - ketanov, ketarol, zaldiar, antibacterial drugs that relieve inflammation. Also shown are recumbent baths in warm water, in which antiseptics are dissolved - nitrofural (furacilin) or potassium permanganate. Healing of the postoperative wound occurs within a month, the period of tissue regeneration depends on the scope of the operation and compliance with all medical prescriptions. After the operation, physical exertion, lifting weights and any physical activity are excluded.
 [ 16 ], [ 17 ], [ 18 ], [ 19 ]
[ 16 ], [ 17 ], [ 18 ], [ 19 ]
Treatment of fistula of the rectum with folk remedies
Fistula of the rectum does not require treatment with folk remedies, but there are situations when it is necessary to quickly alleviate the patient's condition, and the operation is still far away. Decoctions, infusions of medicinal herbs, which are used in the form of compresses, microclysters or rectal baths, can have an anti-inflammatory effect. Calendula, aloe, St. John's wort, plantain, oak bark and sage have proven themselves well. You can also use homemade ointments with the addition of honey or propolis. Honey can be used not only externally, it should be taken internally, mixed with ground aloe leaves, the leaves are often replaced with aloe juice (proportion - 1/1). Fistula of the rectum after surgery is also well treated with folk recipes. Lotions from a decoction of chamomile or a decoction of calendula accelerate tissue healing. The herb is brewed in the following way: 2 tablespoons of dry herb are poured with a liter of boiled water, left to boil for 5 minutes, cooled to an acceptable temperature. Tampons soaked in such a decoction are applied to the already healed wound, the tampon can be kept for no more than an hour, then it should be changed for a fresh one.
Please note that treatment of rectal fistula with folk remedies can in no way be an alternative to drug or surgical treatment, as it is not highly effective and threatens the recurrence of new fistulas.

