Medical expert of the article
New publications
Fibrosis of the retroperitoneum
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
A rare disease, retroperitoneal fibrosis, is characterized by excessive growth of fibrous tissue behind the posterior outer surface of the stomach and intestines, i.e., in the retroperitoneal space. The fibrous tissue is rough, dense, and grows in the area between the spinal column and organs such as the pancreas, kidneys, ureters, etc. When the growth is severe, pressure is exerted on these organs, which leads to secondary pathologies and symptoms.
Retroperitoneal fibrosis has another name – Ormond’s disease. This name is due to the fact that it was the urologist Dr. Ormond who first described the disease in the middle of the last century and associated it with a non-specific inflammatory process in the retroperitoneal tissue. There are also other less common terms: fibrous peritonitis, retroperitoneal fibrosis, etc.
Epidemiology
Retroperitoneal fibrosis is most often diagnosed in men aged 40-60, but can also occur at any other age. The incidence of the disease depending on gender is 2:1 (men and women).
The cause of retroperitoneal fibrosis can be found in only 15% of cases. Overall, the disease is considered relatively rare. One Finnish study found a prevalence of 1.4 per 100,000 inhabitants and an incidence of 0.1 per 100,000 person-years. [ 1 ] However, another study reported a higher incidence of 1.3 per 100,000. [ 2 ]
In childhood, the pathology occurs only in isolated cases.
Retroperitoneal fibrosis is predominantly bilateral, although unilateral lesions also occur. The most common localization of the disease process is the IV-V lumbar vertebrae zone, but the pathology can spread to the entire area from the lower curvature of the spine to the ureteropelvic region.
When the pathological focus reaches large sizes, the aorta and inferior vena cava may be affected.
Causes retroperitoneal fibrosis
Experts still cannot pinpoint the exact causes of retroperitoneal fibrosis. It is assumed that the disease occurs due to inflammatory or immune reactions. Some doctors associate the pathology with systemic connective tissue disorders. The basic pathogenetic criterion discovered is increased expression of the IgG4 complex by plasma cells.
Retroperitoneal fibrosis often becomes a secondary pathology caused by a number of possible reasons:
- Diseases affecting the kidneys, ureters or other structures located in close proximity to the retroperitoneal tissue.
- Malignant tumor processes, including rectal cancer, prostate carcinoma, bladder cancer.
- Infectious processes (brucellosis, tuberculosis, toxoplasmosis).
- Renal pelvis reflux, renal trauma with urine extravasation.
- Abdominal trauma, internal bleeding, lymphoproliferative disorders, lymphadenectomy, colectomy, aortic interventions.
- Radiation therapy targeting the abdominal and pelvic organs.
- Long-term use of ergot preparations, as well as Bromocriptine, Hydralazine, Methyldopa, high doses of antibiotics and β-blockers.
- Allergic intolerance to medications, cases of hypersensitivity reaction to medical drugs and chemicals.
The role of hereditary predisposition is not completely excluded: in particular, some cases of retroperitoneal fibrosis development were associated with carriage of the human leukocyte marker HLA-B27. Other possible genetic associations are currently being studied.
Risk factors
There are several known factors that can lead to the formation of retroperitoneal fibrosis. These include:
- tumor malignant processes;
- chronic inflammation of the pancreas;
- chronic hepatitis;
- tuberculosis of the spinal column;
- radiation damage;
- injuries to the lumbar and abdominal cavity, internal bleeding;
- intoxication (chemical, medicinal).
In many patients, no association with any factors can be found. In such cases, the retroperitoneal fibrosis is said to be idiopathic in origin.
Pathogenesis
In the vast majority of cases, the development of retroperitoneal fibrosis is associated with the presence of lymphocytic plasma cells that produce IgG4. The disease is often systemic in nature, since fibrous changes are also observed in the lymph nodes, pancreas, and pituitary structures. Tumor edema of the affected organs, fibrous sclerotic reaction, and lymphoplasmatic infiltration of varying intensity are observed. The fibrotic process leads to compression of the ureter and vascular network (blood and lymphatic), as well as the kidneys. [ 3 ]
In some cases, the formation of retroperitoneal fibrosis is caused by the appearance of malignant tumors. The growth of fibrous tissue is noted against the background of the presence of malignant cells in the retroperitoneal space, or with the occurrence of lymphoma, sarcoma, in the presence of metastases from other organs. [ 4 ]
The fibrous infiltrate is represented by multiple lymphocytes, lymphocytic plasma cells, macrophages, and, less frequently, neutrophils. Proinflammatory structures are embedded in collagen clusters that unite near small vessels. The disease is classified as IgG4-related if there is a moire fibrous pattern, eosinophilic infiltration, and obliterating phlebitis. Myeloid tissue cells are degranulated, and an active inflammatory-fibrous reaction is observed. [ 5 ]
Symptoms retroperitoneal fibrosis
The clinical picture of retroperitoneal fibrosis is most often characterized by the following symptoms:
- vague pain in the abdomen, side, lower back, groin area;
- periodically elevated temperature, which then normalizes and rises again, often accompanied by chills;
- swelling of the lower body;
- venous disorders, thrombophlebitis;
- sometimes – increased blood pressure;
- emaciation;
- diarrhea, nausea, indigestion, increased gas formation and other dyspeptic symptoms;
- attack of renal colic;
- urinary disorders (most often – dysuria, hematuria);
- feeling of heaviness in the legs, severe fatigue.
The primary symptoms of retroperitoneal fibrosis are caused by deterioration of blood circulation in the abdominal cavity. The initial clinical picture may include the following signs:
- dull pain in the abdomen or back, with the inability to determine a clear localization;
- pain in the side, lower limb;
- swelling and pallor of one or both lower limbs.
As the disease progresses, abdominal pain becomes severe and other symptoms appear:
- loss of appetite;
- emaciation;
- increase in temperature;
- nausea, dyspepsia;
- lack of urination;
- clouding of consciousness.
Signs of renal failure may develop later. [ 6 ]
First signs
The most common first complaint of patients with retroperitoneal fibrosis is constant dull pain in the abdomen, or lower back, or right and left hypochondrium. The pain radiates to the groin area, external genitalia, legs. The early stage of the pathology may be manifested by a moderate increase in temperature and leukocytosis, an increase in ESR.
Signs indicating compression of tubular retroperitoneal structures gradually appear: arterial hypertension, pyelonephritis, hydronephrosis develop. Chronic renal failure appears somewhat later: over a period of 4 weeks to two years. Partial or complete ureteral obstruction occurs in approximately 80% of patients, and oligo or anuria develops in 40% of cases. [ 7 ]
Stages
Clinical symptoms of retroperitoneal fibrosis depend on the stage of the pathological process. As a rule, the disease is characterized by slow development, with gradual progression. During its course, the disease goes through the following stages:
- The initial period of disease development.
- An active period characterized by the spread of the cellular and fibrous process to the retroperitoneal structures.
- The period of compression of fibrous masses of structures involved in the pathological process. [ 8 ]
Forms
It is customary to distinguish between primary (idiopathic) retroperitoneal fibrosis and secondary lesions. Specialists point to the autoimmune origin of idiopathic retroperitoneal fibrosis. Secondary pathology usually develops as a result of other various painful conditions and diseases:
- malignant tumors;
- infectious lesions;
- chronic liver pathologies;
- diseases of the intestines, pancreas;
- urogenital pathologies;
- tuberculous lesions of the spinal column;
- various intoxications (including drug-induced ones). [ 9 ]
Primary idiopathic retroperitoneal fibrosis most often begins in the retroperitoneal tissue that surrounds the iliac vessels, with further spread to the sacral promontory and renal hilum. [ 10 ]
Complications and consequences
Every second patient with retroperitoneal fibrosis develops high blood pressure, compression of the ureters with further development of renal failure is noted. [ 11 ]
Remote complications may include:
- excess accumulation of fluid in the abdominal cavity (ascites);
- vascular disorders (phlebitis, thrombosis);
- hydrocele in men;
- obstruction of the bile ducts, jaundice;
- intestinal obstruction;
- compression of the spine, compression of spinal nerves, disruption of blood supply to the spinal cord.
Many complications can end fatally. In particular, pathological processes in the ureters provoke the development of pyelonephritis, hydronephrosis, chronic renal failure. Approximately 30% of patients have atrophic changes in the kidneys, aortic changes are observed, which can ultimately cause the development of an aneurysm.
Diagnostics retroperitoneal fibrosis
Retroperitoneal fibrosis is difficult to diagnose. Firstly, the disease is relatively rare. Secondly, it has no specific symptoms and is disguised as various other pathologies. There is no specificity in the results of laboratory tests. Very often, patients are prescribed incorrect, inaccurate treatment: instead of retroperitoneal fibrosis, patients are treated for urological and gastroenterological pathologies that are not related to fibrotic processes. Meanwhile, the disease worsens and spreads, worsening the prognosis.
In order to suspect the presence of retroperitoneal fibrosis in a patient, the doctor must adhere to the following diagnostic algorithm:
- Laboratory tests show the following pathological changes:
- increased levels of proinflammatory markers (ESR, C-reactive protein);
- an increase in IgG4 over 135 mg/dl against the background of histological signs.
- It is mandatory to study the levels of urea, creatinine, and glomerular filtration rate to assess renal function.
- Urinalysis may show hematuria, proteinuria, low specific gravity.
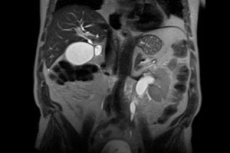
- Instrumental diagnostics should include visualization techniques such as magnetic resonance imaging and computed tomography. Computer diagnostics allows us to distinguish between idiopathic and secondary fibrous pathology. Ultrasound examination is necessary to confirm the initial stage of the disease process, to obtain characteristics of hydronephrosis, and to identify changes in the aorta. Contrast is used to obtain clearer results. Positron emission tomography is prescribed to identify hidden infectious and inflammatory and malignant diseases.
- A biopsy is indicated to clarify the diagnosis. The early stage of fibrotic process development is characterized by the detection of hypervascular tissue with perivascular lymphocytic infiltrate, as well as macrophages with lipid inclusions. At the late stage of retroperitoneal fibrosis development, a characteristic avascular mass is detected that has no cellular structuring.
Differential diagnosis
The symptoms of a retroperitoneal abscess often have much in common with other pathological conditions, in particular, with urological pathologies:
- bilateral hydronephrosis (renal dropsy);
- ureteral strictures (abnormal narrowing of the canal);
- achalasia of the ureters (neuromuscular dysplasia).
The main difference between retroperitoneal fibrosis and the above-mentioned pathologies is the obstruction of the ureters in the area of their intersection with the iliac vessels: above this intersection, an expansion of the ureters is noted, and below it, no changes are detected.
Who to contact?
Treatment retroperitoneal fibrosis
Treatment of retroperitoneal fibrosis depends on the exact location of the pathology, its scale, the degree of compression of internal organs and the presence of an infectious component. Since the disease is rare, with a poorly understood etiology, there is currently no single standard for its treatment. There is no clear definition of the role of conservative therapy and the optimal method of surgical treatment.
The scale of drug treatment generally depends on the underlying cause of retroperitoneal fibrosis. For example, intoxication fibrosis disappears after the toxic agent has ceased to act. If we are talking about a malignant tumor process, then the treatment is appropriate.
The idiopathic form of retroperitoneal fibrosis is cured in many patients by using immunosuppressants and proteolytic drugs. According to indications, anti-inflammatory, antibacterial, detoxifying and symptomatic therapy is used. Surgery may be prescribed in the development of acute conditions or if drug therapy is ineffective.
If chronic pyelonephritis is diagnosed, appropriate therapy for the disease is prescribed.
Surgical treatment
Patients with early stage retroperitoneal fibrosis without clear indications for surgical treatment are prescribed drug therapy with the use of corticosteroid and proteolytic drugs.
However, quite often it is necessary to resort to surgical treatment: the operation is called ureterolysis, it involves freeing the ureters from the surrounding fibrous tissue. Some patients are shown resection of the ureter and subsequent imposition of anastomosis, transplantation of the small intestinal segment, or the use of prosthetics. [ 12 ], [ 13 ]
In advanced stages, with pronounced hydronephrosis and development of chronic pyelonephritis, reconstructive plastic surgery is performed simultaneously with the removal of the urinary canal by the method of pyelo or nephropyelostomy, puncture nephrostomy under ultrasound observation. After surgery, the patient is prescribed long-term corticosteroid support, which is necessary to suppress fibrous growth. Most often, the drug of choice is Cortisol 25 mg per day for 8-12 weeks.
An initial dose of prednisone 1 mg/kg per day (maximum dose 80 mg/day) is usually given for about 4-6 weeks. The dose can then be gradually reduced over 1-2 years depending on the progression of the disease. If the disease does not respond adequately to steroid therapy alone, immunosuppressants can be used concomitantly with steroids. Agents that have been used with apparent success in case reports and case series include azathioprine, methotrexate, mycophenolate mofetil, cyclophosphamide, cyclosporine. [ 14 ] Additionally, drugs that accelerate resorption (Lidase, Longidaza) are used. [ 15 ], [ 16 ]
Prevention
Specific prevention of retroperitoneal fibrosis has not been developed, which is due to the unclear causes of the disease. This is especially true for idiopathic forms of pathology. Secondary retroperitoneal fibrosis can be prevented in most cases if you follow these recommendations:
- give up bad habits, do not smoke, do not abuse alcohol;
- avoid stressful situations, physical and emotional overstrain;
- do not overeat, do not starve, eat little by little several times a day;
- give preference to high-quality food of plant and animal origin, refuse semi-finished products, fast food, fatty and salty foods, smoked foods;
- observe hygiene rules, brush your teeth regularly, wash your hands before eating, as well as after visiting the street and the toilet;
- spend more time outdoors and be physically active;
- avoid abdominal trauma;
- If any symptoms appear, consult a doctor and do not self-medicate;
- after abdominal surgery, strictly follow all doctor’s orders and recommendations;
- avoid hypothermia and overheating of the body;
- drink enough clean water every day;
- During meals, pay attention to chewing food thoroughly, do not be distracted by conversations, the computer, etc.
Our health largely depends on our lifestyle. Therefore, following these simple rules will help to support and preserve it for many years.
Forecast
Retroperitoneal fibrosis is a rare and difficult to diagnose disease, which often causes a delayed start of treatment and prolonged ineffective medication. Often, patients are mistakenly treated for other similar pathologies or directed therapy to eliminate already developed complications, such as arterial hypertension, tumor processes, chronic enterocolitis, cholecystopancreatitis, ulcerative lesions of the stomach and duodenum, pyelonephritis, hydronephrosis, chronic renal failure, anuria, etc.
Early initiation of treatment can significantly improve the prognosis of the pathology. Retroperitoneal fibrosis in the early stages of development responds well to treatment with corticosteroids, but therapy should be prescribed before the development of irreversible fibrotic processes. The recurrence rate after cessation of treatment ranges from less than 10-30%, although one series reported a recurrence rate of more than 70%. [ 17 ] Advanced disease is treated only by surgical intervention, and mortality depends on the degree of obstruction and complications associated with it.
A rare disease, retroperitoneal fibrosis, is characterized by excessive growth of fibrous tissue behind the posterior outer surface of the stomach and intestines, i.e., in the retroperitoneal space. The fibrous tissue is rough, dense, and grows in the area between the spinal column and organs such as the pancreas, kidneys, ureters, etc. When the growth is severe, pressure is exerted on these organs, which leads to secondary pathologies and symptoms.
Retroperitoneal fibrosis also has another name – Ormond’s disease. This name is due to the fact that it was the urologist Dr. Ormond who first described the disease in the middle of the last century and associated it with a non-specific inflammatory process in the retroperitoneal tissue. There are also other less common terms: fibrous peritonitis, retroperitoneal fibrosis, etc. [ 18 ]

