Medical expert of the article
New publications
Ethylene glycol vapor poisoning
Last reviewed: 12.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
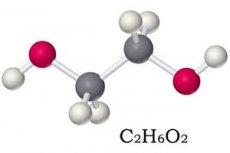
Although 1,2-dioxyethane (ethanediol-1,2) is classified as the third toxicity class out of four in terms of its negative impact on the body, ethylene glycol poisoning leads to very serious consequences and can result in death.
This slightly oily, sweet-tasting, transparent, colorless, odorless liquid is a dihydric alcohol. Worldwide, about two-thirds of ethylene glycol is used as a chemical intermediate and in automotive antifreeze, brake fluid, and anti-corrosion additives.
Read more about the production of ethylene glycol, its properties and applications in the publication – Ethylene glycol.
Epidemiology
According to statistics from the Agency for Toxic Substances and Disease Registry (USA), from 2006 to 2013 inclusive, 45,097 cases of ethylene glycol poisoning were registered among Americans, and in 154 cases the outcome was fatal.
Every year in the United States, over 5.5 thousand cases of poisoning with this substance are recorded. In 84% of cases, poisoning occurs accidentally, two thirds of victims are men. And the mortality rate due to intoxication fluctuates from 1 to 22% - depending on the amount of ethylene glycol that has entered the body and the timeliness of medical care.
In the UK, there are up to 400 ethylene glycol poisonings per year, but 18% of cases involve children under five, and 65% of cases among adults are suicidal.
Causes ethylene glycol poisoning
The minimum lethal dose of ethylene glycol for adults is considered to be 1.4-1.6 ml per kilogram of body weight, i.e. with a weight of 80 kg it is 200-220 ml (according to other data, 90-100 ml). Causes of poisoning are accidental or intentional consumption of a certain amount of ethylene glycol; for example, alcoholics who replace vodka with antifreeze or brake fluid may have repeated poisoning with ethylene glycol.
The pathogenesis of the toxic effects of ethanediol-1,2 lies in the products of its metabolism, which disrupt the functioning of the kidneys, cardiovascular and nervous systems.
Ethylene glycol is rapidly absorbed through the gastrointestinal tract, and its vapor or aerosol is absorbed through the respiratory tract. After absorption, ethylene glycol is distributed in internal fluids.
In the liver and kidneys it undergoes enzymatic metabolism. First, with the help of aldehyde oxidase and aldehyde dehydrogenase it is broken down to glycaldehyde, which is quickly converted into glycosyl acid (glycolate) and dialdehyde ethanedioic acid (glyoxal).
Further transformation of glycosyl acid leads to the formation of glyoxylate, which, in turn, breaks down into: formate (methanoic acid salt), ethanedioic or oxalic acid salt (oxalate), glycine (aminoacetic acid) and carbon dioxide gas.
As a result of the accumulation of acidic metabolites, the acid-base balance of the body is disrupted (including changes in the pH of arterial blood), provoking a state of metabolic acidosis, which negatively affects the functioning of the nervous system, lungs and heart.
Elimination of ethylene glycol occurs via exhaled carbon dioxide and urinary excretion of ethylene, glycol, and glycolic acid. The half-life in humans is thought to be in the range of 2.5–8.4 hours.
 [ 11 ]
[ 11 ]
Risk factors
Risk factors for ethylene glycol poisoning, as well as its cause, are its ingestion. This also applies to cases where poisoning occurs with brake fluid, which contains 1,2-dioxyethane.
When this substance is poured out at an industrial plant or from a container located in a residential area, poisoning does not occur. However, people working in industries that use ethylene glycol may have prolonged contact with raw materials or products containing it, which may cause ethylene glycol poisoning in small doses. In particular, airport service workers involved in the treatment of runways and aircraft against icing in the winter (by spraying appropriate liquids) may be exposed to low levels of ethylene glycol on the respiratory tract. Therefore, ethylene glycol has now begun to be replaced by propylene glycol.
Experts note that factors influencing the risk of poisoning from exposure to ethylene glycol include its dose, duration and nature of contact. At the same time, it is believed that background concentrations of ethylene glycol in the air, soil, surface and ground water do not lead to poisoning.
Symptoms ethylene glycol poisoning
After ingesting ethylene glycol, the first signs of CNS depression manifest themselves as alcohol intoxication - with dizziness, agitation or increased drowsiness. But this short latent period is quickly replaced by the first phase (stage or step) of toxic effects, which can last up to 12 hours and manifests itself in gastrointestinal upset (with nausea, vomiting and abdominal pain), as well as tachycardia, confusion, convulsions, headache, nystagmus and decreased urination.
In the second stage (12-36 hours after ingestion), metabolic acidosis and associated cardiac and pulmonary symptoms of ethylene glycol poisoning develop: shallow rapid breathing (tachypnea) with tachycardia, increased pulmonary ventilation (hyperpnea), cyanosis, pulmonary edema and/or cardiac arrest.
Often in the second phase of poisoning, cardiopulmonary symptoms are not so obvious, so attention should be paid to acidosis, acute renal failure and suppression of CNS functions, which can manifest as neurological symptoms, including hearing loss and facial paralysis.
During the third phase of intoxication, which lasts on average 24-72 hours, nephrotoxicity of ethylene glycol metabolites comes to the fore - kidney damage (with parenchyma necrosis and deposition of oxalate crystals), causing pain in the lumbar region and impaired diuresis (anuria or oliguria).
Inhalation exposure to ethylene glycol at an average concentration in the air of up to 140-200 mg/m3 for five minutes causes ethylene glycol vapor poisoning – severe irritation of the upper respiratory tract, including a burning sensation in the trachea and coughing, and also negatively affects the lungs, heart, central and peripheral nervous systems, liver, hematopoietic and lymphoreticular systems.
At lower concentrations, chronic ethylene glycol poisoning is possible, accompanied by a feeling of weakness, dizziness, irritation of the mucous membranes of the nose and eyes, increased heart rate and blood pressure, and immunosuppression.
Complications and consequences
Ethylene glycol intoxication is quite common, and without prompt detection and treatment, the risk of death from this substance remains high. This is due to consequences and complications such as acute renal failure, hemodynamic instability, and brain damage leading to coma.
A decrease in calcium levels in the crocodile's blood – hypocalcemia – leads to severe convulsions, tetany, irregular heartbeats and heart block.
Diagnostics ethylene glycol poisoning
Because many of the clinical symptoms of ethylene glycol poisoning are present in other types of intoxication, diagnosis is often difficult.
In addition, patients, especially children, who are admitted to a healthcare facility within an hour of ethylene glycol ingestion may not yet show signs.
The following tests help diagnose ethylene glycol poisoning:
- blood test for ethylene glycol content;
- blood and urine analysis for osmolar range, that is, to determine the osmolarity of blood serum;
- biochemical blood tests to determine pH, serum electrolytes (calcium, potassium, chlorides), glucose, urea and creatinine levels;
- urine analysis for pH, nitrogen and creatinine content; levels of protein, β-N-acetylglucosaminidase and β-2-microglobulin;
- urine microscopy to detect calcium oxalate crystals.
Differential diagnosis
Based on the totality of the results of these analyses, differential diagnostics are also performed, since differential diagnostics include poisoning with salicylates, metformin, methanol, isopropyl alcohol, chloroethanol, dimethyl sulfate, as well as alcoholic or diabetic ketoacidosis, lactic acidemia or acute renal failure.
Read also the article – Diagnosis of acute poisoning
Treatment ethylene glycol poisoning
First of all, emergency assistance is required for ethylene glycol poisoning: emptying the stomach and washing it with a large amount of soda solution (a tablespoon per liter of water), which is effective only immediately after swallowing ethanol - within the first hour.
But there is no point in using activated carbon, since it does not adsorb 1,2-dioxyethane.
Further treatment of ethylene glycol poisoning is aimed at blocking the formation of its toxic metabolites and the development of acidosis, for which an antidote for ethylene glycol poisoning is administered intravenously - ethanol or 4-methylpyrazole.
In most cases, ethanol (ethyl alcohol) is used: intravenously – 10 ml/kg of 10% ethanol in 5% dextrose for 30 minutes; orally – diluted 95% ethyl alcohol (at the rate of 1 ml/kg).
At a sufficient concentration of ethanol in the blood (up to 100 mg/dl), the biochemical transformation of ethylene glycol almost completely stops. In emergency situations, toxicologists recommend taking an equivalent amount of any strong alcoholic beverage internally.
Hemodialysis helps to quickly reduce the content of ethanediol-1,2 metabolites in the blood in acute poisoning.
Further efforts of doctors are directed:
- to correct acidosis and hyperkalemia by intravenous drip administration of sodium bicarbonate solution (150-200 ml/hour) during the first few hours with monitoring of potassium levels in the blood;
- to remove the body from states of acidosis (with blood pH <7.25-7.3) – also by performing hemodialysis or peritoneal dialysis;
- to maintain adequate diuresis (administration of fluids orally or intravenously);
- to combat hypocalcemia – with calcium gluconate infusions (10% solution with dextrose or saline).
Depending on the pathological consequences of intoxication, appropriate medications are used to support the functions of individual organs and systems.
Vitamins are also necessary: thiamine (B1) 100 mg daily and pyridoxine (B6) - 10-25 mg per day. Taking these vitamins helps break down one of the toxic metabolites - glycosyl acid.
Outside the acute phase of poisoning, it is possible to use physiotherapeutic treatment, in particular, with the help of therapeutic hypothermia, as well as hyperbaric oxygenation.
Also read – Methods to Stimulate Natural Detoxification.
Forecast
It should be borne in mind that ethylene glycol poisoning is a potentially fatal intoxication. And a favorable prognosis for its outcome largely correlates with early diagnosis and treatment.
If medical attention is sought at later stages of poisoning, the prognosis may be poor, especially in patients with severe acidosis. Even if they survive, there is a high probability of developing chronic neurological impairment, as well as kidney damage, often requiring permanent dialysis or a kidney transplant.

