Medical expert of the article
New publications
Enteropathies
Last reviewed: 29.06.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Enteropathy is a general term used to describe various diseases and disorders associated with pathologic changes in the mucosa of the gastrointestinal (GI) tract. Enteropathies can have different causes and manifest with a variety of symptoms. Some of the best known forms of enteropathies include:
- Celiac disease (coliacia): An autoimmune disease in which the mucous membrane of the small intestine is damaged by a reaction to the protein gluten. Celiac disease can lead to impaired nutrient absorption and has a variety of symptoms including diarrhea, abdominal bloating, fatigue, and weight loss.
- Crohn's disease and ulcerative colitis: These are chronic inflammatory diseases of the GI tract that can affect different parts of the GI tract. They involve inflammation of the mucous membranes and can cause abdominal pain, diarrhea, bleeding, and other symptoms.
- Lactase deficiency: In this condition, the body does not produce enough lactase, an enzyme needed to digest milk and milk products. Lactase deficiency can cause bloating, gas, and diarrhea after eating dairy products.
- Eosinophilic enteritis: This is a rare disorder in which the GI mucosa is affected by allergic reactions, which can lead to inflammation and other symptoms such as abdominal pain and diarrhea.
- Microscopic colitis: This is a group of diseases that include collagenous colitis and lymphocytic colitis. They are characterized by chronic inflammatory changes in the mucosa that can cause diarrhea and abdominal pain.
Treatment of enteropathies depends on the type and cause. It may include dietary changes, medications, symptom control, and in some cases surgery. Enteropathies are usually diagnosed and treated by a gastroenterologist.
Causes of the enteropathies
The causes and risk factors for different forms of enteropathies can be varied and depend on the specific type of enteropathy. Below are some of the most common causes and risk factors associated with different types of enteropathies:
-
Celiac disease:
- Genetics: Hereditary predisposition to celiac disease plays an important role in its development.
- Gluten intake: Celiac disease is associated with intolerance to gluten, a protein found in wheat, barley and rye.
- Environmental factors: Some environmental factors may contribute to the development of celiac disease.
-
Crohn's disease:
- Genetics: Genetic factor plays a role in the occurrence of Crohn's disease.
- Inflammation and immunologic aspects: Inflammation and immunologic aspects are key in this disease.
-
Ulcerative colitis:
- Genetics: Genetic predisposition also plays an important role in the development of ulcerative colitis.
- Immunologic factors: Immunologic disorders may contribute to mucosal inflammation.
-
Inflammatory bowel disease (IBD):
- Genetics: Genetic predisposition may be a risk factor.
- Environmental factors: Environmental factors such as infections and nutrition may play a role in the development of IBD.
-
Intestinal infections:
- Pathogens: A variety of bacteria, viruses, and parasites can cause intestinal infections.
-
Medications and supplements:
- Some medications and supplements can cause irritation and damage to the gastrointestinal mucosa.
-
Food allergies and intolerances:
- Intolerance to lactose, gluten or other foods can cause inflammation and discomfort.
- Genetic disorders and rare diseases: Some rare genetic disorders may be associated with enteropathies.
- Autoimmune diseases: Some autoimmune diseases can affect the gastrointestinal mucosa.
- Psychosocial factors: Stress and psychosocial aspects can also influence the development of some forms of enteropathy.
Pathogenesis
The pathogenesis of enteropathies can be varied, and it depends on the specific type of enteropathy and its underlying disease. Here are some general points regarding the pathogenesis of enteropathies:
- Inflammation: Many enteropathies are associated with inflammation of the gastrointestinal mucosa. Inflammation can occur due to various causes such as immune disorders, infections, allergic reactions or autoimmune diseases.
- Immune mechanisms: Some enteropathies, such as celiac disease, are associated with immune disorders. In the case of celiac disease, the immune system has an aggressive effect on its own tissues, especially the small intestinal mucosa, leading to inflammation and damage.
- Allergic reactions: In some cases, enteropathies can develop as a result of allergic reactions to certain foods or other allergens. This can cause inflammation and damage to the mucous membranes.
- Genetic factors: Some enteropathies may have a genetic predisposition. For example, some forms of celiac disease are associated with inherited genetic mutations.
- Infections: Some infections, such as Helicobacter pylori infection, can cause chronic gastritis and other enteropathies through mechanisms of inflammation and toxic effects.
- Damage to the mucosa: Mechanical damage to the mucosa of the gastrointestinal tract, such as prolonged use of certain medications, can lead to the development of enteropathy.
The pathogenesis of enteropathies can be complex and multifactorial, and it can vary from disease to disease. In order to accurately identify and treat enteropathies, it is important to diagnose and consult with a physician who can suggest the best treatment plan for your specific situation.
Symptoms of the enteropathies
The symptoms of enteropathies can vary depending on the specific type of enteropathy and its cause. However, some common symptoms that may be seen in various forms of enteropathies include the following:
- Diarrhea: This is one of the most common symptoms of enteropathies. Diarrhea can be characterized as liquid, frequent or prolonged.
- Abdominal pain: Abdominal pain can be acute, dull, spasmodic or persistent. They may occur in different areas of the abdomen and may be accompanied by bloating or discomfort.
- Abdominal bloating: Patients with enteropathies often experience abdominal bloating and discomfort.
- Blood in the stool: Some enteropathies can cause bleeding from the GI tract, which can manifest as blood in the stool or through rectal bleeding.
- Fatigue: Patients with enteropathies may experience generalized weakness, fatigue, and loss of energy.
- Weight Loss: Weight loss can be the result of impaired digestion and nutrient absorption.
- Changes in appetite: Enteropathies can affect appetite, causing either an increase or decrease in appetite.
- Changes in bowel habits: There may be changes in the regularity and pattern of defecation, including constipation or diarrhea.
- Allergy Symptoms: Some forms of enteropathies may have allergic symptoms such as itching, rash, and angioedema.
Symptoms can vary in severity and duration, and they can vary from case to case.
Enteropathies syndromes
There are several different enteropathy syndromes, each with its own characteristic symptoms and features. The following are some of the best known enteropathy syndromes:
- Irritable bowel syndrome (IBS): This syndrome is characterized by chronic abdominal pain, diarrhea, constipation, and/or alternating changes in stool. Symptoms may be exacerbated by stress and may persist for long periods of time.
- Syndrome of poorly explained gastroenterologic symptoms (SMGEC): This syndrome describes a situation where patients have chronic gastrointestinal symptoms, but investigations and examinations show no obvious structural or biochemical abnormalities.
- Post-infectious enteropathy: This syndrome can develop after a gastrointestinal infection and is characterized by prolonged diarrhea and other symptoms.
- Eosinophilic enteropathy: Eosinophilic granulocytes accumulate in the mucous membrane of the gastrointestinal tract, causing inflammation and symptoms such as abdominal pain and diarrhea.
- Slow Digestion Syndrome: This syndrome is characterized by the slow passage of food through the digestive tract, which can lead to constipation, bloating and discomfort.
- Diarrhea-frequency syndrome: Patients with this syndrome often experience excessive frequency of defecation and diarrhea.
- Imperfect Absorption Syndrome: This syndrome is associated with impaired absorption of certain nutrients in the gastrointestinal tract, which can lead to dietary deficiencies.
- Post-operative enteropathy: This syndrome can develop after gastrointestinal surgery and is characterized by changes in stool, abdominal pain, and other symptoms.
It is important to note that each of these syndromes has its own unique characteristics and requires an individualized approach to diagnosis and treatment. It is recommended that patients with symptoms of enteropathy consult a physician to determine a specific diagnosis and develop an appropriate treatment plan.
Enteropathy in children
This is a group of different diseases and conditions associated with pathologic changes in the gastrointestinal (GI) tract of children. These conditions can have different causes and manifestations. It is important to realize that enteropathy in children can be caused by a variety of factors and requires careful diagnosis and treatment. Here are some of the most common types of enteropathies in children:
- Celiac disease: Celiac disease is one of the most well-known types of enteropathy in children. It is an autoimmune disease caused by an intolerance to gluten, a protein found in wheat, barley, and rye. Children with celiac disease may experience symptoms such as diarrhea, abdominal bloating, poor nutrient absorption, and stunted growth.
- Lactase deficiency: This condition occurs when children do not produce enough lactase, an enzyme needed to digest milk and milk products. Symptoms may include diarrhea, abdominal pain, and gas after eating dairy products.
- Infectious enteropathies: Various infections such as viruses, bacteria, and parasites can cause enteropathies in children. Symptoms depend on the type of infection but may include diarrhea, vomiting, abdominal pain, and fever.
- Eosinophilic enteropathy: This is a condition in which the GI mucosa undergoes inflammation caused by a build-up of eosinophils. Children with this enteropathy may experience abdominal pain, diarrhea, and vomiting.
- Other Enteropathies: There are other forms of enteropathies in children, including allergic reactions to certain foods, genetic disorders, inflammatory GI disease, and other conditions.
Treatment for enteropathy in children will depend on the type of enteropathy and the cause. It may include dietary changes, medication, symptom control and, in rare cases, surgery. To diagnose and treat children with enteropathy, it is important to see a doctor, usually a pediatrician or pediatric gastroenterologist, to perform appropriate tests and develop a treatment plan.
Enteropathy in children has its own characteristics that need to be considered in the diagnosis, treatment and management of these conditions. Here are some of the main features of enteropathy in children:
- Variety of causes: Enteropathy in children can be caused by a variety of factors such as infections, allergies, genetic disorders, autoimmune diseases, food intolerance and other conditions. It is important to perform a diagnosis to determine the underlying cause.
- Development and growth: Children are in a stage of active physical and psychological development. This means that enteropathy can have a negative impact on a child's normal growth and development, so early detection and treatment are very important.
- Symptoms and manifestations: The symptoms of enteropathy may appear differently in children, depending on their age and the type of enteropathy. In infants and young children, these may include abdominal pain, diarrhea, vomiting, poor weight gain, and irritability. Older children may experience similar symptoms, as well as fatigue, concentration problems, and delayed growth and development.
- Diagnosis: Diagnosisof enteropathy in children requires a special approach. This may include blood tests, biopsies of the GI mucosa, immunologic studies and other methods.
- Treatment and diet: Children with enteropathy may require a special diet, including restricting certain foods or introducing special food formulas. Medication, including antibiotics, anti-inflammatory drugs, and other medications, may also be prescribed depending on the type of enteropathy.
- Support and education: Parents of children with enteropathy may require education and support in diet, care and symptom management. Consultation with physicians, dietitians, and other professionals can help manage these challenges.
Forms
Enteropathies can take many forms depending on their cause, characteristics, and symptoms. Here are some of the most common forms of enteropathies:
- Celiac disease (product intolerance to gluten): This is a chronic autoimmune disease in which the immune system is stunned by the ingestion of gluten, a protein found in wheat, barley, and rye. This can lead to damage to the mucous membrane of the small intestine and impaired absorption of nutrients.
- Crohn's disease and ulcerative colitis: These are chronic inflammatory bowel diseases that can affect different parts of the digestive system. They can cause inflammation, ulcers, and other complications.
- Non-specific colorectal ulcer: This is another inflammatory bowel disease that can cause inflammation and ulcers in the large intestine.
- Microscopic colitis: This is a condition in which inflammation of the bowel is not visible on routine endoscopic examination, but is visible on microscopic analysis of biopsy specimens.
- Food allergies: Some people may have allergic reactions to certain foods, which can cause enteropathic symptoms such as diarrhea and abdominal pain.
- Infectious Enteropathies: Enteropathies can be caused by an infection such as bacterial or viral inflammation of the intestines.
- Pseudomembranous colitis: This is an acute inflammatory bowel disease that is often associated with antibiotic use and can lead to pseudomembranous growths on the colonic mucosa.
Different types of enteropathies can have different causes and symptoms. Here is a brief description of each of these enteropathies:
- Gluten enteropathy (celiac disease): Also known as celiac disease, is a chronic autoimmune disease in which patients develop an intolerance to the protein gluten, which is found in wheat, barley, and rye. Symptoms include diarrhea, abdominal bloating, fatigue and weight loss. The disease can also cause damage to the mucous membrane of the small intestine.
- Protein enteropathy: This term can refer to various forms of enteropathies related to proteins in food. It can often include an allergic reaction to proteins in food such as cow's milk, soy proteins, and others. Symptoms can vary, but usually include diarrhea, abdominal pain, and other food allergic reactions.
- Exudative enteropathy: This is a condition in which the mucous membrane of the gastrointestinal tract secretes exudate (plasma or other fluids) into the stomach or intestines. This can be due to a variety of causes, including inflammatory diseases, infections, or medication effects.
- Chronicenteropathy: The term "chronic enteropathy" describes any long-term or prolonged enteropathy that lasts for a long time. Causes can vary and include chronic inflammatory diseases, autoimmune conditions, and other factors.
- Allergic enteropathy: This is a condition in which the mucous membrane of the gastrointestinal tract is affected by an allergic reaction to certain allergens in food or other substances. Symptoms may include diarrhea, abdominal pain, vomiting, and other allergic symptoms.
- Diabetic enteropathy: This is a complication of diabetes in which high blood sugar levels can damage nerves and blood vessels, including those in the gastrointestinal tract. Diabetic enteropathy can lead to digestive problems and symptoms such as diarrhea, constipation, and abdominal pain.
- Autoimmune enteropathy: This is a condition in which the body's immune system begins to attack its own mucous membrane in the gastrointestinal tract. An example of such an enteropathy is celiac disease.
- Secondary enteropathies: These enteropathies develop as a consequence of other conditions or diseases. For example, viral infections or immunodeficiency conditions can lead to enteropathy.
- Enteropathy induced by food proteins: This form of enteropathy can develop in response to a food allergy or intolerance to certain proteins or food components. An example is lactose-induced enteropathy in lactose intolerance.
- Functional enteropathy: This is a condition in which patients experience symptoms related to the gastrointestinal tract but no structural or biochemical abnormality is detected. An example is irritable bowel syndrome (IBS).
- Alcoholic enteropathy: This type of enteropathy is associated with prolonged and excessive alcohol consumption. Alcohol can damage the mucous membrane of the gastrointestinal tract, leading to inflammation, ulcers and other changes. This can cause symptoms such as abdominal pain, diarrhea, and digestive disorders.
- Enzyme enteropathy: This type of enteropathy is associated with a deficiency of enzymes necessary for normal digestion. For example, celiac disease is a form of enzyme enteropathy in which the immune system attacks the mucosa of the small intestine aggressively when gluten, a protein found in wheat, barley, and rye, is consumed.
- Steroid-dependent enteropathy: This condition is associated with long-term use of glucocorticosteroids (steroids), which can cause a variety of gastrointestinal side effects, including ulcers, bleeding, and mucosal abnormalities.
- Uremic enteropathy: This type of enteropathy is associated with chronic kidney failure and the accumulation of waste products in the body. This can lead to various gastrointestinal disturbances and symptoms such as nausea, vomiting and diarrhea.
- Membranous digestive enteropathy: This term may describe enteropathies associated with impaired digestion in the mucosa of the gastrointestinal tract, which may include impaired absorption of nutrients.
- Proliferative enteropathy: This is a condition in which the mucosa of the gastrointestinal tract undergoes abnormal or excessive cell proliferation. This can lead to the formation of polyps or other neoplasms. Proliferative changes may be associated with various diseases and may require surgical intervention.
- Congenital bundle enteropathy: This rare genetic enteropathy is characterized by lactose intolerance (a sugar found in milk and milk products) from birth. Patients with this enteropathy cannot digest lactose, which can cause diarrhea, abdominal bloating, and other symptoms.
- Necrotizing enteropathy: This is a condition in which the mucous membrane of the gastrointestinal tract undergoes necrosis (cell death) due to various factors such as infections, hemorrhage, or ischemia (impaired blood supply).
- Glycine enteropathy: This is an inherited disorder associated with an abnormal metabolism of the amino acid glycine. It can lead to a variety of neurological and psychomotor disorders, as well as other problems including glycinuronuropathic enteropathy, which can affect the digestive system.
- Lymphoid enteropathy: This is a condition in which the intestinal mucosa contains excessive amounts of lymphoid tissue. It can be associated with a variety of conditions including Crohn's disease, ulcerative colitis, and other inflammatory diseases of the GI tract.
- Reactive enteropathy: This is a condition in which the mucous membrane of the gastrointestinal tract becomes inflamed or irritated in response to certain factors. This can include infection (such as viral or bacterial), an allergic reaction to food or medications, and other irritating influences. Reactive enteropathy may present with symptoms similar to enteritis or gastroenteritis.
- Toxic enteropathy: This is a condition in which the mucous membrane of the gastrointestinal tract is damaged or destroyed by exposure to toxins or poisons, such as certain drugs, chemicals, or infections. Examples include toxic gastroenteritis, caused by the bacterium Clostridium difficile, or toxic enteropathy due to the misuse of certain medications.
- Atrophic enteropathy: This is a condition in which the mucosa of the gastrointestinal tract undergoes atrophy, that is, reduction in size and functional changes. Examples of such conditions are celiac disease and atrophic gastritis, which can lead to impaired nutrient absorption and other digestive problems.
- Enzyme deficiency enteropathies: These enteropathies are associated with a deficiency of certain enzymes necessary for normal digestive function. Examples of these conditions are lactase deficiency (lactose intolerance), in which the body cannot properly digest the milk sugar lactose, and other enzyme deficiency conditions.
Complications and consequences
Complications and consequences of enteropathies can vary depending on their cause and severity. Some of the common complications and consequences of enteropathies include:
- Diarrhea: One of the most common symptoms of enteropathies is diarrhea, which can be chronic or remain for a long time.
- Nutrient deficiencies: Due to impaired intestinal function, the absorption of nutrients such as vitamins, minerals and proteins may be impaired. This can lead to a lack of important elements and the development of nutrient deficiencies.
- Weight Loss: Persistent diarrhea and nutrient deficiencies can lead to weight loss and debility.
- Anemia: Some enteropathies can lead to iron deficiency and anemia due to lack of red blood cells.
- Growth retardation in children: Children with chronic enteropathies may have delayed growth and development.
- Medication Complications: Treatment of enteropathies may involve the use of medications that can also cause various side effects and complications.
- Autoimmune complications: Some forms of enteropathies may be associated with autoimmune processes that can affect other organs and systems in the body.
- Complications if not treated correctly: If enteropathy is misdiagnosed or treated, it can lead to worsening of the condition and the development of more serious complications.
Diagnostics of the enteropathies
Diagnosis of enteropathies involves a number of methods and tests that allow the doctor to determine the type and cause of the enteropathy. The approach to diagnosis will depend on the specific symptoms and suspicion of the disease. Here are some common diagnostic methods:
- Medical history: The physician interviews the patient to learn about the symptoms, duration and nature of the disease, as well as the presence of other medical conditions, hereditary factors and risk factors.
- Physical Exam: The physician performs a physical examination of the patient, including evaluation of the abdomen and other organs to look for signs that might indicate enteropathy.
- Laboratory blood tests: Various laboratory blood tests are performed, including inflammation tests (e.g., C-reactive protein and red blood cell counts), antibody tests, biochemical values (e.g., glucose, protein, and other markers), and other tests that may indicate the presence of enteropathy.
- Instrumental Investigations:
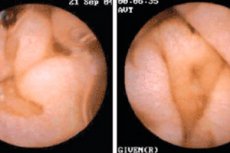
- Gastroenteroscopy: This is a procedure in which a thin, flexible tube with a camera (endoscope) is inserted through the mouth or nose to view the mucosa of the gastrointestinal tract and take biopsies for laboratory analysis.
- Radiologic studies: When gastroenteroscopy is not appropriate, radiologic techniques such as barium studies may be used to evaluate the structure and function of the gastrointestinal tract.
- Computed tomography (CT) or magnetic resonance imaging (MRI): Sometimes these techniques are used to look at the abdominal organs and surrounding tissues in more detail.
- Endoscopic biopsies: During a gastroenteroscopy or colonoscopy, tissue (biopsy) may be taken from the mucosa for laboratory analysis to detect abnormal changes, inflammation, or the presence of specific diseases.
- Tests for allergies or food intolerances: In some cases, specific tests are performed to detect allergic reactions to certain foods.
- Genetic tests: Genetic tests may be performed to diagnose inherited forms of enteropathies such as celiac disease.
Diagnosis of enteropathy requires collaboration between physicians from different specialties, including gastroenterologists, allergists-immunologists, surgeons, and pathologists.
Various laboratory tests and assays are performed to diagnose gluten enteropathy. Here are the main tests and investigations that can be used to diagnose celiac disease:
- Antibodies to transglutaminase (tTG antibodies): This antibody test is one of the most commonly used tests to diagnose celiac disease. High levels of tTG antibodies may indicate the presence of an autoimmune reaction to gluten. This test is usually performed on blood.
- Immunoglobulin A (IgA): IgA levels in the blood may also be measured, as low IgA levels can affect the accuracy of antibody test results. If IgA levels are low, your doctor may suggest using other diagnostic methods.
- Endomysium antibodies (EMA antibodies): This antibody test can be performed to confirm a diagnosis of celiac disease. A positive EMA test result indicates an increased likelihood of celiac disease.
- Gastroscopy (endoscopy): Gastroscopy allows the doctor to visually assess the condition of the small intestine mucosa and take a biopsy for laboratory analysis. In celiac disease, inflammation and lesions may be seen on the mucosa.
- Small intestinal mucosal biopsy: This is the gold standard for diagnosing celiac disease. During gastroenteroscopy, a small sample of tissue from the small intestine is taken to analyze for characteristic changes such as inflammation and damage to the villi.
- Other tests: Additional tests may include genetic tests to detect an inherited predisposition to celiac disease and tests for serum iron and ferritin levels to assess iron deficiency that may result from poor absorption in the small intestine.
Differential diagnosis
Differential diagnosis of enteropathies involves the process of identifying and distinguishing between different forms of enteropathies, as they may have similar symptoms. This is important to determine the correct diagnosis and prescribe appropriate treatment. Here are some steps in the differential diagnosis of enteropathies:
- Gatheringmedical and medical history: The physician begins by gathering detailed medical and medical history information, including symptoms, duration of symptoms, dietary habits, medical history, and medication intake.
- Physical Examination: The doctor performs a physical examination of the patient to look for signs such as abdominal pain, abdominal bloating, skin rashes, and other physical symptoms.
- Laboratory tests: Various laboratory tests are done to evaluate the condition of the intestines and the body as a whole. This may include blood tests, stool tests, urine tests, and others.
- Instrumental examinations: Endoscopic examinations such as gastrofibroscopy or colonoscopy may be used to visually inspect the internal structures of the bowel and take biopsy samples.
- Immunologic tests: Immunologic tests such as antibody tests may be performed to determine autoimmune enteropathies.
- Genetic Testing: To diagnose celiac disease, genetic testing is performed to look for genes associated with the disease.
- Exclusion of other diseases: The differential diagnosis also includes the exclusion of other diseases that may mimic the symptoms of enteropathy, such as irritable bowel syndrome (IBS), gastritis, peptic ulcer disease, infectious diseases, and others.
- Monitoring response to treatment: Once a diagnosis is made and treatment is started, it is important to monitor how the patient responds to therapy to make sure it is effective.
Treatment of the enteropathies
Treatment for enteropathy depends on its type, cause, and symptoms. Enteropathies can be caused by a variety of factors, including infections, inflammation, allergies, genetic disorders, and other conditions. Treatment is usually prescribed by a doctor and may include the following:
-
Medication treatment:
- Antibiotics: If enteropathy is caused by a bacterial or infectious cause, antibiotics may be prescribed.
- Anti-inflammatorydrugs: Anti-inflammatory drugs such as mesalamine or steroids may be used to treat inflammatory forms of enteropathy, such as Crohn's disease or ulcerative colitis.
- Immunomodulators and biologics: In cases of chronic inflammatory GI disease, your doctor may prescribe immunomodulatory drugs or biologics to suppress inflammation and control symptoms.
-
Nutritional therapy:
- In the case of food allergies or intolerance to certain foods, it may be necessary to eliminate these foods from the diet. For example, in the case of celiac disease, gluten should be completely eliminated from the diet.
- Lactose restriction may be required in patients with lactase deficiency.
-
Symptomatic treatment:
- Medications to relieve symptoms, such as pain medications, antispasmodics, or antiemetics, may be used to improve patient comfort.
-
Treatment of the underlying cause:
- When enteropathy is due to an underlying condition, such as an autoimmune disease or genetic disorder, it is important to treat and manage that underlying condition.
-
Surgical intervention:
- In some cases, such as external masses, polyps, or certain complications, surgery may be required to remove the affected areas of the GI tract.
Diet for enteropathy
Depends on the specific type and cause of the condition. For effective nutritional therapy, a specific diagnosis must be determined and a diet plan must be developed based on that diagnosis. Here are some general recommendations for diet in different types of enteropathies:
-
Gluten enteropathy (celiac disease):
- The main thing in this case is the complete elimination of gluten from the diet. Gluten is found in wheat, barley and rye.
- Foods you can eat: corn, rice, potatoes, potatoes, buckwheat, oats (if labeled gluten-free), meat, fish, fruits, vegetables, milk and dairy products (if they do not contain gluten additives).
- Avoid foods and dishes that contain wheat flour, barley, rye, maltodextrin and other ingredients with gluten.
-
Enzyme enteropathy:
- To aid in digestion, enzyme supplements (such as for lactose or bromelain) can be used to help the body digest food.
- Avoid foods that can cause severe fermentation in the stomach, such as legumes, cabbage, soda, and carbonated drinks.
-
Alcoholic enteropathy:
- It is important to avoid alcohol completely.
- Pay attention to the condition of the liver and digestive system.
-
Uremic enteropathy:
- The diet for chronic kidney failure may include protein, phosphorus, and potassium restriction.
- Sodium and fluid intake may be restricted depending on the stage of the disease.
-
Enteropathy with impaired membrane digestion:
- Enzyme supplements may be used to improve digestion.
- Avoid foods that can irritate the mucous membranes, such as hot spices and acidic foods.
It is important to note that diet recommendations can vary greatly depending on the specific diagnosis and stage of the disease. Before making any changes to your diet, be sure to consult with your doctor or dietitian to get personalized recommendations and follow the recommendations that are right for you.
Clinical Guidelines
Clinical guidelines for the management of enteropathies depend on the specific form of this disease and may include different methods of diagnosis, treatment and care. Here are general clinical guidelines that may be applicable in the context of enteropathies:
-
Diagnosis and evaluation:
- Evaluation of the patient's medical and family history.
- Collection of detailed symptoms and complaints.
- Conducting a physical examination.
- Laboratory tests of blood, stool, urine, and others to evaluate gut function and detect inflammatory or autoimmune processes.
- Instrumental investigations such as endoscopy with biopsy to visualize and assess bowel health.
-
Treatment:
- Treatment depends on the specific form of enteropathy and may include the following:
- Use of drug therapy such as antibiotics, anti-inflammatory drugs, immunosuppressive drugs and others, depending on the diagnosis.
- Dietary recommendations and dietary changes. For example, in celiac disease, it is important to eliminate gluten from food.
- Control of symptoms such as diarrhea or abdominal pain.
- Surgical intervention may be required in some cases, especially if there are complications or damage to the intestines.
-
Monitoring and follow-up treatment:
- Regular medical monitoring and examinations to assess the effectiveness of treatment and changes in the patient's condition.
- Modify treatment as needed based on monitoring results.
-
Lifestyle and support:
- Patients with enteropathies can receive guidance on maintaining a healthy lifestyle, including proper nutrition, physical activity levels, and stress management.
- Support from a psychologist or psychiatrist can be helpful, especially in chronic forms of enteropathies such as Crohn's disease.
-
Investigation of causes and prevention: In some cases, such as celiac disease, it is important to determine the causes of the disease and take steps to prevent it in the patient's relatives.
-
Patient education: Educating the patient about their disease, dietary restrictions, and proper care practices can be a key aspect of successful management of enteropathy.
Clinical guidelines may vary depending on the patient's specific diagnosis and condition, so it is important to obtain medical advice from specialists, such as gastroenterologists or allergists, for an individualized approach to the diagnosis and treatment of enteropathy.

