Medical expert of the article
New publications
Corynebacterium
Last reviewed: 06.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Diphtheria is an acute infectious disease, mainly affecting children, which manifests itself as deep intoxication of the body with diphtheria toxin and characteristic fibrinous inflammation at the site of localization of the pathogen. The name of the disease comes from the Greek word diphthera - skin, film, since a dense, grayish-white film is formed at the site of reproduction of the pathogen.
The causative agent of diphtheria - Corynebacterium diphtheriae - was first discovered in 1883 by E. Klebs in sections of film, and was obtained in pure culture in 1884 by F. Leffler. In 1888, E. Roux and A. Yersin discovered its ability to produce an exotoxin, which plays a major role in the etiology and pathogenesis of diphtheria. The production of antitoxic serum by E. Behring in 1892 and its use since 1894 for the treatment of diphtheria made it possible to significantly reduce mortality. A successful attack on this disease began after 1923 in connection with the development of a method for obtaining diphtheria anatoxin by G. Raion.
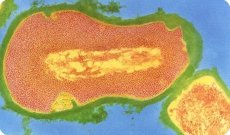
The causative agent of diphtheria belongs to the genus Corynebacterium (class Actinobacteria). Morphologically, it is characterized by the fact that the cells are club-shaped and thickened at the ends (Greek coryne - club), form branches, especially in old cultures, and contain granular inclusions.
The genus Corynebacterium includes a large number of species, which are divided into three groups.
- Corynebacteria are parasites of humans and animals and pathogenic for them.
- Corynebacteria pathogenic to plants.
- Nonpathogenic Corynebacteria. Many species of Corynebacteria are normal inhabitants of the skin, mucous membranes of the pharynx, nasopharynx, eyes, respiratory tract, urethra and genitals.
Morphology of corynebacteria
C. diphtheriae are straight or slightly curved non-motile rods 1.0-8.0 μm long and 0.3-0.8 μm in diameter; they do not form spores or capsules. They often have swellings at one or both ends and often contain metachromatic granules - volutin grains (polymetaphosphates), which acquire a bluish-purple color when stained with methylene blue. A special Neisser staining method has been proposed for their detection. In this case, the rods are stained straw-yellow, and the volutin grains are dark brown, and are usually located at the poles. Corynebacterium diphtheriae stains well with aniline dyes, is gram-positive, but in old cultures it often becomes discolored and has a negative stain according to Gram. It is characterized by pronounced polymorphism, especially in old cultures and under the influence of antibiotics. The G + C content in DNA is about 60 mol %.
Biochemical properties of corynebacteria
The diphtheria bacillus is an aerobe or facultative anaerobe, the temperature optimum for growth is 35-37 °C (growth limits are 15-40 °C), the optimal pH is 7.6-7.8. It is not very demanding to nutrient media, but grows better on media containing serum or blood. Curdled serum Roux or Loeffler media are selective for diphtheria bacteria, growth on them appears after 8-12 hours in the form of convex colonies the size of a pinhead, grayish-white or yellowish-cream in color. Their surface is smooth or slightly granular, on the periphery the colonies are somewhat more transparent than in the center. The colonies do not merge, as a result of which the culture acquires the appearance of shagreen leather. On the broth, growth manifests itself as uniform turbidity, or the broth remains transparent, and a delicate film forms on its surface, which gradually thickens, crumbles and settles in flakes to the bottom.
A feature of diphtheria bacteria is their good growth on blood and serum media containing such concentrations of potassium tellurite that they suppress the growth of other types of bacteria. This is due to the fact that C. diphtheriae reduce potassium tellurite to metallic tellurium, which, deposited in microbial cells, gives the colonies a characteristic dark gray or black color. The use of such media increases the percentage of diphtheria bacteria seeding.
Corynebacterium diphtheriae ferment glucose, maltose, galactose with the formation of acid without gas, but do not ferment (as a rule) sucrose, have cystinase, do not have urease and do not form indole. According to these characteristics, they differ from those coryneform bacteria (diphtheroids) that are most often found on the mucous membrane of the eye (Corynebacterium xerosus) and nasopharynx (Corynebacterium pseiidodiphtheriticum) and from other diphtheroids.
In nature, there are three main variants (biotypes) of the diphtheria bacillus: gravis, intermedins and mitis. They differ in morphological, cultural, biochemical and other properties.
The division of diphtheria bacteria into biotypes was made taking into account the forms of diphtheria in patients with which they are isolated with the greatest frequency. The gravis type is most often isolated from patients with a severe form of diphtheria and causes group outbreaks. The mitis type causes milder and sporadic cases of the disease, and the intermedius type occupies an intermediate position between them. Corynebacterium belfanti, previously attributed to the mitis biotype, is isolated as an independent, fourth, biotype. Its main difference from the gravis and mitis biotypes is the ability to reduce nitrates to nitrites. Corynebacterium belfanti strains have pronounced adhesive properties, and both toxigenic and non-toxigenic variants are found among them.
 [ 6 ], [ 7 ], [ 8 ], [ 9 ], [ 10 ]
[ 6 ], [ 7 ], [ 8 ], [ 9 ], [ 10 ]
Antigenic structure of corynebacteria
Corynebacterium is very heterogeneous and mosaic. Several dozen somatic antigens have been found in all three types of diphtheria pathogens, according to which they are divided into serotypes. In Russia, a serological classification has been adopted, according to which 11 serotypes of diphtheria bacteria are distinguished, of which 7 are main (1-7) and 4 are additional, rarely encountered serotypes (8-11). Six serotypes (1, 2, 3, 4, 5, 7) belong to the gravis type, and five (6,8,9,10,11) belong to the mitis type. A disadvantage of the serotyping method is that many strains, especially non-toxigenic ones, have spontaneous agglutination or polyagglutinability.
 [ 11 ]
[ 11 ]
Phage typing of Corynebacterium diphtheriae
Various phage typing schemes have been proposed for differentiating diphtheria bacteria. According to M. D. Krylova's scheme, using a set of 9 phages (A, B, C, D, F, G, H, I, K), it is possible to type most toxigenic and non-toxigenic strains of the gravis type. Taking into account sensitivity to the specified phages, as well as cultural, antigenic properties and the ability to synthesize corycins (bactericidal proteins), M. D. Krylova identified 3 independent groups of corynebacteria of the gravis type (I-III). Each of them contains subgroups of toxigenic and their non-toxigenic analogues of diphtheria pathogens.
Corynebacterium resistance
Corynebacterium diphtheriae exhibits high resistance to low temperatures, but quickly dies at high temperatures: at 60 °C - within 15-20 minutes, when boiling - after 2-3 minutes. All disinfectants (lysol, phenol, chloramine, etc.) in the usually used concentration destroy it in 5-10 minutes. However, the diphtheria pathogen tolerates drying well and can remain viable for a long time in dried mucus, saliva, and dust particles. In a fine aerosol, diphtheria bacteria remain viable for 24-48 hours.
Pathogenicity factors of corynebacteria
The pathogenicity of Corynebacterium diphtheriae is determined by the presence of a number of factors.
Factors of adhesion, colonization and invasion
The structures responsible for adhesion have not been identified, but without them the diphtheria bacillus would not be able to colonize cells. Their role is performed by some components of the pathogen's cell wall. The invasive properties of the pathogen are associated with hyaluronidase, neuraminidase, and protease.
A toxic glycolipid contained in the cell wall of the pathogen. It is a 6,6'-diester of trehalose containing corynemycolic acid (C32H64O3) and corynemycolic acid (C32H62O3) in equimolar ratios (trehalose-6,6'-dicorynemicolate). The glycolipid has a destructive effect on tissue cells at the site of pathogen reproduction.
Exotoxin, which determines the pathogenicity of the pathogen and the nature of the pathogenesis of the disease. Non-toxigenic variants of C. diphtheriae do not cause diphtheria.
The exotoxin is synthesized as an inactive precursor - a single polypeptide chain with a molecular weight of 61 kD. It is activated by the bacterial protease itself, which cuts the polypeptide into two peptides linked by disulfide bonds: A (m.w. 21 kD) and B (m.w. 39 kD). Peptide B performs an acceptor function - it recognizes the receptor, binds to it and forms an intramembrane channel through which peptide A penetrates the cell and implements the biological activity of the toxin. Peptide A is an ADP-ribosyltransferase enzyme, which ensures the transfer of adenosine diphosphate ribose from NAD to one of the amino acid residues (histidine) of the protein elongation factor EF-2. As a result of the modification, EF-2 loses its activity, and this leads to the suppression of protein synthesis by ribosomes at the translocation stage. The toxin is synthesized only by those C. diphtheriae that carry the genes of the moderate converting prophage in their chromosome. The operon encoding the synthesis of the toxin is monocistronic, it consists of 1.9 thousand nucleotide pairs and has a toxP promoter and 3 regions: toxS, toxA and toxB. The toxS region codes 25 amino acid residues of the signal peptide (it ensures the release of the toxin through the membrane into the periplasmic space of the bacterial cell), toxA - 193 amino acid residues of peptide A, and toxB - 342 amino acid residues of peptide B of the toxin. Loss of the prophage by the cell or mutations in the tox operon make the cell slightly toxigenic. On the contrary, lysogenization of non-toxigenic C. diphtheriae by the converting phage turns them into toxigenic bacteria. This has been proven unambiguously: the toxigenicity of diphtheria bacteria depends on their lysogenization by tox-converting corynephages. Corynephages integrate into the chromosome of corynebacteria using the mechanism of site-specific recombination, and strains of diphtheria bacteria can contain 2 recombination sites (attB) in their chromosomes, and corynephages integrate into each of them with the same frequency.
Genetic analysis of a number of non-toxigenic strains of diphtheria bacteria, carried out using labeled DNA probes carrying fragments of the corynephage tox operon, showed that their chromosomes contain DNA sequences homologous to the corynephage tox operon, but they either encode inactive polypeptides or are in a "silent" state, i.e. inactive. In this regard, a very important epidemiological question arises: can non-toxigenic diphtheria bacteria transform into toxigenic ones under natural conditions (in the human body), similar to what happens in vitro? The possibility of such a transformation of non-toxigenic cultures of corynebacteria into toxigenic ones using phage conversion was demonstrated in experiments on guinea pigs, chicken embryos and white mice. However, whether this occurs during the natural epidemic process (and if so, how often) has not yet been established.
Due to the fact that diphtheria toxin in the body of patients has a selective and specific effect on certain systems (the sympathetic-adrenal system, heart, blood vessels and peripheral nerves are mainly affected), it is obvious that it not only inhibits protein biosynthesis in cells, but also causes other disturbances in their metabolism.
The following methods can be used to detect the toxicity of diphtheria bacteria:
- Biological tests on animals. Intradermal infection of guinea pigs with a filtrate of a broth culture of diphtheria bacteria causes necrosis at the injection site. One minimal lethal dose of toxin (20-30 ng) kills a guinea pig weighing 250 g when injected subcutaneously on the 4th-5th day. The most characteristic manifestation of the toxin's action is damage to the adrenal glands, which are enlarged and sharply hyperemic.
- Infection of chicken embryos. Diphtheria toxin causes their death.
- Infection of cell cultures. Diphtheria toxin causes a distinct cytopathic effect.
- A solid-phase enzyme-linked immunosorbent assay using peroxidase-labeled antitoxins.
- Use of a DNA probe for direct detection of the tox operon in the chromosome of diphtheria bacteria.
However, the simplest and most common method for determining the toxicity of diphtheria bacteria is serological - the gel precipitation method. Its essence is as follows. A strip of sterile filter paper measuring 1.5 x 8 cm is moistened with antitoxic antidiphtheria serum containing 500 AE in 1 ml and applied to the surface of the nutrient medium in a Petri dish. The dish is dried in a thermostat for 15-20 minutes. The test cultures are seeded with plaques on both sides of the paper. Several strains are seeded on one dish, one of which, obviously toxic, serves as a control. The plates with the cultures are incubated at 37 °C, the results are taken into account after 24-48 hours. Due to the counter diffusion of the antitoxin and toxin in the gel, a clear precipitation line is formed at the site of their interaction, which merges with the precipitation line of the control toxigenic strain. Non-specific precipitation bands (they are formed if, in addition to the antitoxin, other antimicrobial antibodies are present in small quantities in the serum) appear late, are weakly expressed and never merge with the precipitation band of the control strain.
Post-infectious immunity
Strong, persistent, practically lifelong, repeated cases of the disease are observed rarely - in 5-7% of those who have had the disease. Immunity is mainly antitoxic in nature, antimicrobial antibodies are of lesser importance.
The Schick test was previously widely used to assess the level of anti-diphtheria immunity. For this purpose, 1/40 of the guinea pig toxin in a volume of 0.2 ml was injected intradermally into children. In the absence of antitoxic immunity, redness and swelling with a diameter of more than 1 cm appear at the injection site after 24-48 hours. Such a positive Schick reaction indicates either a complete absence of antitoxin or that its content is less than 0.001 AE/ml of blood. A negative Schick reaction is observed when the antitoxin content in the blood is higher than 0.03 AE/ml. If the antitoxin content is lower than 0.03 AE/ml but higher than 0.001 AE/ml, the Schick reaction can be either positive or, sometimes, negative. In addition, the toxin itself has a pronounced allergenic property. Therefore, to determine the level of anti-diphtheria immunity (quantitative content of antitoxin), it is better to use RPGA with an erythrocyte diagnosticum sensitized with diphtheria toxoid.
Epidemiology of diphtheria
The only source of infection is a person - a sick person, a recovering person, or a healthy carrier of the bacteria. Infection occurs through airborne droplets, airborne dust, and through various objects used by sick or healthy carriers: dishes, books, linen, toys, etc. In case of contamination of food products (milk, creams, etc.), infection is possible through the alimentary route. The most massive excretion of the pathogen occurs in the acute form of the disease. However, people with latent, atypical forms of the disease are of the greatest epidemiological significance, since they are often not hospitalized and are not detected immediately. A patient with diphtheria is infectious during the entire period of the disease and part of the recovery period. The average period of carriage of bacteria in recovering people varies from 2 to 7 weeks, but can last up to 3 months.
Healthy carriers play a special role in the epidemiology of diphtheria. In conditions of sporadic morbidity, they are the main distributors of diphtheria, contributing to the preservation of the pathogen in nature. The average duration of carriage of toxigenic strains is somewhat shorter (about 2 months) than non-toxigenic (about 2-3 months).
The reason for the formation of healthy carriage of toxigenic and non-toxigenic diphtheria bacteria has not been fully disclosed, since even a high level of antitoxic immunity does not always ensure complete liberation of the body from the pathogen. Perhaps the level of antibacterial immunity has a certain significance. Of primary epidemiological significance is the carriage of toxigenic strains of diphtheria bacteria.
 [ 12 ], [ 13 ], [ 14 ], [ 15 ], [ 16 ], [ 17 ], [ 18 ], [ 19 ]
[ 12 ], [ 13 ], [ 14 ], [ 15 ], [ 16 ], [ 17 ], [ 18 ], [ 19 ]
Symptoms of diphtheria
People of any age are susceptible to diphtheria. The pathogen can penetrate the human body through the mucous membranes of various organs or through damaged skin. Depending on the localization of the process, diphtheria of the pharynx, nose, larynx, ear, eye, genitals and skin are distinguished. Mixed forms are possible, for example, diphtheria of the pharynx and skin, etc. The incubation period is 2-10 days. In the clinically expressed form of diphtheria, a characteristic fibrinous inflammation of the mucous membrane develops at the site of localization of the pathogen. The toxin produced by the pathogen first affects the epithelial cells, and then the nearby blood vessels, increasing their permeability. The outgoing exudate contains fibrinogen, the coagulation of which leads to the formation of a grayish-white filmy coating on the surface of the mucous membrane, which is tightly fused with the underlying tissue and, when torn off, causes bleeding. The consequence of damage to blood vessels may be the development of local edema. Diphtheria of the pharynx is especially dangerous, as it can cause diphtheritic croup due to edema of the mucous membrane of the larynx and vocal cords, from which 50-60% of children with diphtheria used to die as a result of asphyxia. Diphtheria toxin, entering the blood, causes general deep intoxication. It mainly affects the cardiovascular, sympathetic-adrenal systems and peripheral nerves. Thus, the symptoms of diphtheria consist of a combination of local signs depending on the localization of the entry gate, and general symptoms caused by poisoning with the toxin and manifested in the form of adynamia, lethargy, pale skin, low blood pressure, myocarditis, paralysis of the peripheral nerves and other disorders. Diphtheria in vaccinated children, if observed, usually proceeds in a mild form and without complications. The mortality rate in the period before the use of serotherapy and antibiotics was 50-60%, now it is 3-6%.
Laboratory diagnostics of diphtheria
The only method of microbiological diagnostics of diphtheria is bacteriological, with mandatory testing of the isolated culture of corynebacteria for toxicity. Bacteriological studies for diphtheria are carried out in three cases:
- for the diagnosis of diphtheria in children and adults with acute inflammatory processes in the pharynx, nose, and nasopharynx;
- according to epidemiological indications of persons who were in contact with the source of the diphtheria pathogen;
- persons newly admitted to orphanages, nurseries, boarding schools, and other special institutions for children and adults, in order to identify possible carriers of the diphtheria bacillus among them.
The material for the study is mucus from the pharynx and nose, film from the tonsils or other mucous membranes, which are the entry point for the pathogen. Sowing is done on tellurite serum or blood media and simultaneously on coagulated serum Roux (coagulated horse serum) or Loeffler (3 parts bovine serum + 1 part sugar broth) media, on which corynebacteria growth appears after 8-12 hours. The isolated culture is identified by a combination of morphological, cultural and biochemical properties, using sero- and phage typing methods whenever possible. In all cases, a toxicity test using one of the above methods is mandatory. The morphological features of corynebacteria are best studied using three methods of staining a smear preparation: Gram, Neisser and methylene blue (or toluidine blue).
Treatment of diphtheria
A specific treatment for diphtheria is the use of anti-diphtheria antitoxic serum containing at least 2000 IU per 1 ml. The serum is administered intramuscularly in doses from 10,000 to 400,000 IU depending on the severity of the disease. An effective treatment method is the use of antibiotics (penicillins, tetracyclines, erythromycin, etc.) and sulfonamides. To stimulate the production of its own antitoxins, anatoxin can be used. To get rid of the bacterial carriage, antibiotics should be used to which the given strain of corynebacteria is highly sensitive.
Specific prophylaxis of diphtheria
The main method of combating diphtheria is mass planned vaccination of the population. For this purpose, various vaccine options are used, including combined ones, i.e. aimed at the simultaneous creation of immunity against several pathogens. The most widespread vaccine in Russia is DPT. It is a suspension of whooping cough bacteria adsorbed on aluminum hydroxide, killed by formalin or thimerosal (20 billion in 1 ml), and contains diphtheria toxoid in a dose of 30 flocculating units and 10 units of tetanus toxoid binding in 1 ml. Children are vaccinated from the age of 3 months, and then revaccinations are carried out: the first after 1.5-2 years, the next ones at the age of 9 and 16 years, and then every 10 years.
Thanks to mass vaccination, which began in the USSR in 1959, the incidence of diphtheria in the country by 1966, compared to 1958, was reduced by 45 times, and its indicator in 1969 was 0.7 per 100,000 population. The subsequent reduction in the volume of vaccinations in the 1980s led to serious consequences. In 1993-1996, Russia was swept by a diphtheria epidemic. Adults, mainly those who had not been vaccinated, and children fell ill. In 1994, almost 40 thousand patients were registered. In connection with this, mass vaccination was resumed. During this period, 132 million people were vaccinated, including 92 million adults. In 2000-2001, the coverage of children with vaccinations within the established period was 96%, and with revaccination - 94%. Due to this, the incidence of diphtheria in 2001 decreased by 15 times compared to 1996. However, in order to reduce the incidence to isolated cases, it is necessary to vaccinate at least 97-98% of children in their first year of life and ensure mass revaccination in subsequent years. It is unlikely that diphtheria will be completely eliminated in the coming years due to the widespread carriage of toxigenic and non-toxigenic diphtheria bacteria. It will also take some time to solve this problem.

