Medical expert of the article
New publications
Chronic sphenoiditis
Last reviewed: 05.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Chronic sphenoiditis (chronic inflammation of the sphenoid sinus, chronic inflammation of the sphenoid sinus, chronic sphenoidal sinusitis (sinusitis sphenaiditis chronica).
"Chronic inflammation of the sphenoid sinus - sphenoiditis - is a disease whose diagnosis often causes significant difficulties. The location of the sinus in the deep sections of the base of the skull, which are important in functional terms, as well as the involvement of the adjacent paranasal sinuses in the inflammatory process contribute to the appearance of unclear, erased clinical symptoms, which complicates diagnosis. The position of the famous otolaryngologist S.A. Proskuryakov (1939) has not lost its relevance in our time, according to whom the diagnosis of "sphenoiditis" should mature in the head of the doctor himself, which requires a lot of time, experience and skill. This, apparently, explains the significant percentage of cases of chronic sphenoiditis detected at autopsy, not diagnosed during life, which emphasizes the "reputation" of the sphenoid sinus as a "forgotten" sinus.
Chronic sphenoiditis is a chronic inflammation of the mucous membrane of the sphenoid sinus, which occurs as a result of ineffective treatment of acute sphenoiditis, calculated over a period of 2-3 months. It is during this period of the inflammatory process in the sphenoid sinus that deep, often irreversible pathomorphological changes in the mucous membrane occur, often spreading to the periosteum and bone tissue of the sphenoid bone. Most often, the chronic inflammatory process occurs in both sphenoid sinuses; according to V.F. Melnik (1994), their bilateral lesion is observed in 65% of cases, in 70% of cases, chronic sphenoiditis is combined with inflammation of other paranasal sinuses. Isolated lesions of the sphenoid sinus, observed in 30% of cases, probably arise in connection with their primary infection from foci of infection localized in the lymphadenoid formations of the nasopharynx, for example, in chronic adenoiditis.
Causes chronic sphenoiditis
The cause of the development of chronic sphenoiditis is the same as that of chronic inflammatory processes in other paranasal sinuses.
The causative agents of the disease are most often representatives of the coccal microflora. In recent years, there have been reports of the isolation of three opportunistic microorganisms as causative agents - Haemophilus influenzae, Streptococcus pneumoniae and Moraxella catharrhalis. The formation of various types of aggressive associations characterized by increased virulence is noted. Fungi, viruses and anaerobes have often been isolated as causative agents of the disease.
Pathogenesis
Most often, the main role in the pathogenesis of chronic sphenoiditis is played by preceding chronic inflammatory diseases of other paranasal sinuses and mainly by chronic sluggish inflammation of the posterior cells of the ethmoid labyrinth. An important role in the pathogenesis of chronic sphenoiditis is played by the anatomical position of the sphenoid sinus and its close connections with the nasopharyngeal lymphadenoid formations. Localization of the chronic focus of infection in them is an important factor in the occurrence of primary chronic inflammation of the mucous membrane of the sphenoid sinus. The famous French otolaryngologist G. Portmann, describing chronic sphenoiditis as a disease with scanty symptoms, an erased clinical picture, often masked by diseases of other paranasal sinuses, notes that chronic sphenoiditis often manifests itself indirectly through the complications it causes (optic neuritis, basal pachymeningitis, optic-chiasmatic arachnoiditis, etc.).
Due to the narrowness of the natural outlet, it closes when the swelling spreads and the inflamed mucous membrane of the nasal cavity infiltrates. In this situation, the latter begins to quickly absorb oxygen and release carbon dioxide, and the oxygen content decreases sharply when purulent exudate appears in the lumen of the sinus. The disease also occurs when unfavorable factors directly affect the mucous membrane of the sinus.
Symptoms chronic sphenoiditis
Chronic sphenoiditis manifests itself with various and vague symptoms, probably related to the deep location of the sinus in the area of the base of the skull, close to the diencephalic and other important structures of the brain. This often causes neurological complications and the appearance of asthenovegetative symptoms: sleep disorders, loss of appetite, memory impairment, paresthesia, persistent subfebrile temperature, impaired glucose tolerance. Most often, chronic sphenoiditis manifests itself with dull pain in the back of the head and discharge into the nasopharynx, mainly in the morning, hyperthermia with subfebrile numbers and severe general weakness. The disease is characterized by a long course with inexpressive symptoms. The inflammatory process is often bilateral, isolated damage to the sinuses is observed in 30% of cases.
The three most important symptoms of the disease are constant, the main one being headache of constant localization: with minor pneumatization of the sinus - in the parietal region, and with major spreading to the occipital region. Characteristic of sphenoiditis is the irradiation of headaches to the retroorbital and frontal regions with the appearance of sensations of "pulling out" or "catching" the eyes.
Another feature is the appearance or increase of pain in the sun and hot rooms, and at night. It is assumed that this is due to the active evaporation of secretion due to high air temperature, the appearance of crusts that close the outlet of the sinus. Such features of headache in chronic sphenoiditis are called "sphenoidal pain syndrome". The second important clinical sign is a subjective odor from the nose, felt only by the patient himself. The appearance of the odor is caused by the fact that the natural opening of the sinus opens in the olfactory region. The third sign is the flow of scanty and viscous exudate along the vault of the nasopharynx and the back wall of the pharynx, which causes irritation of the mucous membrane and often lateral pharyngitis on the side of the lesion.
The symptoms of chronic sphenoiditis depend mainly on the form of the process (closed, open) and the routes of spread of humoral derivatives of the inflammatory process, which in turn is determined by the anatomical structure of the sphenoid sinus (its volume, thickness of the bone walls, the presence of dihiscenses, vascular emissaries, etc.). The location of the sphenoid sinus at the base of the skull and in close proximity to important brain centers (pituitary gland, hypothalamus, other subcortical ganglia, cavernous sinus system, etc.) can cause the appearance of direct and repercussion symptoms indicating the involvement of these formations in the pathological process. Therefore, the symptoms of chronic sphenoiditis, although erased, hidden, and masked by signs of, for example, ethmoiditis, still contain elements of "specificity" related to the above-mentioned "repercussion" symptoms, which are not very characteristic of diseases of other paranasal sinuses. An example of such symptoms may be the initial manifestations of optic-chiasmatic arachnoiditis, paresis of the abducens nerve, etc.
The "closed" form of chronic sphenoiditis, characterized by the absence of communication between the sinus and the nasopharynx (absence of drainage function), manifests itself with significantly more pronounced symptoms than the "open" form, in which the exudate formed in the sinus is freely released through natural drainage openings. In the closed form (absence of discharge in the nasopharynx), patients complain of fullness and heaviness in the head, distension in the perinasal region and in the depth of the orbits; constant, periodically worsening headaches radiating to the crown and orbits, intensifying when shaking the head. The pain syndrome in chronic sphenoiditis is characterized by the symptom of a "constant pain point", the localization of which is strictly individual for each patient, strictly repeating in the same place with each exacerbation of the inflammatory process. Headaches in the closed form of chronic sphenoiditis are caused not only by pressure on the sensory nerves by accumulating exudate, but also by neuritis of the sensory nerve endings, which is characteristic of any chronic sinusitis, the alteration of which by inflammatory toxins leads to the development of perivascular neuralgia and neuropathies, characteristic of Slader, Charlin, Harris syndromes, etc. Such fixed pain loci may include pain radiating to the supra- and infraorbital areas, to certain teeth, to the mammillary process area, and to the upper neck. When chronic sphenoiditis is combined with chronic ethmoiditis, hyposmia is possible. The closed type of the process leads to putrefactive decay of the sphenoid sinus tissues and to objective and subjective cacosmia. A characteristic sign of chronic sphenoiditis is a decrease in visual acuity even in the absence of signs of optic-chiasmatic arachnoiditis, and cases of temporary hypoacusis, until complete recovery, are also common.
In the "open" form of chronic sphenoiditis, the main complaint of patients is the presence of viscous, foul-smelling discharge in the nasopharynx, which dries into yellow-gray-green crusts. To remove these discharges and crusts, patients are forced to resort to rinsing the nasal cavity and nasopharynx with various solutions.
Objective local symptoms include hyperemia of the nasal mucosa and parenchymatous hypertrophy of the nasal turbinates; insufficiently effective action of vasoconstrictors; purulent discharge in the nasal passages, drying into crusts that are difficult to separate; accumulation of viscous pus and small polyps is determined in the olfactory cleft, which may indicate concomitant chronic ethmoiditis. On the back wall of the pharynx - viscous pus and crusts flowing from the nasopharynx; during posterior rhinoscopy, a polyp can sometimes be detected originating from the sphenoid sinus, covered with purulent discharge flowing from the superior nasal passage and covering the posterior end of the middle turbinate. The latter is hypertrophied, often changed by polyps. Purulent discharge flowing down the back wall of the pharynx accumulates in the laryngopharynx and dries into crusts that are difficult to expectorate.
Chronic sphenoiditis, as a rule, is characterized by a sluggish course, some scarcity of rhinological symptoms and can basically be characterized by the same criteria as chronic inflammatory processes in other paranasal sinuses. However, in chronic sphenoiditis, symptoms of a general nature often come to the fore, such as signs of neurological and asthenovegetative disorders (sleep disturbances, memory impairment, loss of appetite, increased irritability). Gastrointestinal disorders are not uncommon due to the constant swallowing of purulent masses accumulating in the hypopharynx. As A.S. Kiselev (1997) notes, some patients may develop a severe hypochondriacal condition requiring psychiatric treatment. Probably, the indicated neurological disorders are caused by the toxicogenic and pathoreflexive influence of the focus of chronic inflammation, located in close proximity to the pituitary-hypothalamic and limbic-reticular systems. This is evidenced, in particular, by signs of emotional disturbances, the appearance of central dizziness, changes in carbohydrate metabolism, etc.
The evolution of chronic sphenoiditis, as with chronic inflammatory processes in other paranasal sinuses, can occur both in the direction of recovery and in the direction of worsening of local and general manifestations of the disease, and under unfavorable conditions (general infections, decreased immunity, some systemic diseases) there is a danger (more often than with chronic inflammatory processes in other paranasal sinuses) of the occurrence of a number of severe complications (orbital phlegmon, optic neuritis, pachymeningitis of the skull base, optic-chiasmatic arachnoiditis, brain abscess, thrombophlebitis of the cavernous sinus, etc.).
Diagnostics chronic sphenoiditis
A method for mass examination of a large contingent of people could be fluorography or CT of the paranasal sinuses.
At the stage of collecting anamnesis, it is necessary to obtain information about the duration of the disease, the features of clinical symptoms, which at first glance do not even have any relation to this type of sinusitis. This concerns, first of all, neurological visual disorders that appear against the background of constant long-term headache and discharge in the nasopharynx.
Physical examination
It is impossible due to the peculiarities of the location of the sphenoid sinus,
Laboratory research
In the absence of complications, as with other types of sinusitis, general blood and urine tests are of little information. Observation of the dynamics of blood glucose levels is mandatory.
Instrumental research
Posterior rhinoscopy reveals edema and hyperemia of the mucous membrane of the nasopharyngeal vault, crusts on its surface, and a "strip of pus" flowing down its lateral wall. In chronic sphenoiditis, hyperplasia of the mucous membrane of the posterior edge of the vomer, the upper edge of the choanae, and the posterior ends of the superior and middle nasal turbinates is often detected. The appearance of a "strip of pus" can be detected during repeated posterior rhinoscopy after careful anemization of the mucous membrane of the olfactory cleft. Most patients have constant edema and hyperemia of the middle nasal turbinates, which creates the illusion of overgrowth of the posterior-superior parts of the nose.
Oropharyngoscopy can reveal signs of granular pharyngitis.
The main method of instrumental diagnostics remains radiography. Performed in axial projection, it makes it possible to clarify the features of sinus pneumatization, the presence and number of chambers, the location of the intersinus septum, the nature of the decrease in the transparency of the sinuses. The introduction of a water-soluble contrast agent into the sinus through a catheter inserted during diagnostic probing of the sphenoid sinus will allow more accurate localization of changes caused by the inflammatory process.
CT and MRI, when taken in axial and coronal projections, undoubtedly provide a significantly greater volume of information, revealing the involvement of other paranasal sinuses and nearby structures of the facial skeleton in the inflammatory process.
Differential diagnosis of chronic sphenoiditis
The closest disease in clinical manifestations is diencephalic syndrome, often manifested by subjective sensations of alternating “flushes” of heat and cold, which is not observed in patients with sphenoiditis.
It is necessary to differentiate the disease from arachnoiditis of the anterior cranial fossa. Sphenoiditis, mainly chronic, differs from this pathology by the presence of "spheroidal pain syndrome", typical localization of exudate secretions and X-ray data,
 [ 19 ]
[ 19 ]
Indications for consultation with other specialists
Observation of the patient by a neurologist and ophthalmologist in dynamics is mandatory. Consultation with an endocrinologist is desirable to clarify the state of the endocrine glands, especially with an elevated level of plasma glucose. Before and after surgical intervention on the sphenoid sinus, consultation with a neurologist is mandatory.
What do need to examine?
How to examine?
Who to contact?
Treatment chronic sphenoiditis
The goals of treatment of chronic sphenoiditis are to restore drainage and aeration of the affected sinus, eliminate formations that interfere with this, remove pathological discharge, and stimulate reparative processes.
Indications for hospitalization
The presence of sphenoidal pain syndrome, discharge into the nasopharynx, characteristic X-ray signs, as well as the lack of effect of conservative treatment within 1-2 days and the appearance of clinical signs of complications are indications for hospitalization. For patients with chronic sphenoiditis, such complications are considered to be an exacerbation of the disease with a previously established diagnosis or long-term unsuccessful treatment, various and vague symptoms associated with nasal pathology.
Non-drug treatment of chronic sphenoiditis
Physiotherapeutic treatment: endonasal electrophoresis with penicillin antibiotics, intrasinus irradiation with helium-neon laser beams.
Drug treatment of chronic sphenoiditis
Until the results of the microbiological examination of the discharge are obtained, broad-spectrum antibiotics can be used - amoxicillin, including in combination with clavulanic acid, cephaloridine, cefotaxime, cefazolin, roxithromycin, etc. Based on the results of the culture, targeted antibiotics should be prescribed; if the discharge is absent or cannot be obtained, the treatment is continued. Fenspiride can be used as part of anti-inflammatory therapy. At the same time, hyposensitizing therapy is carried out with mebhydrolin, chloropyramine, ebastine, etc. Vasoconstrictor nasal drops (decongestants) are prescribed, at the beginning of the treatment of a mild action (ephedrine solution, dimethindene in combination with phenylzfrip, and instead of nightly intake of drops or spray, a gel can be used); if there is no effect within 6-7 days, treatment is carried out with imidazole drugs (naphazoline, xylometazoline, oxymetazoline, etc.). The use of immunomodulators (thymic group drugs of the 3rd and 5th generations, azoximer) is mandatory.
Anemia of the mucous membrane of the olfactory cleft is carried out using various decongestants.
 [ 20 ], [ 21 ], [ 22 ], [ 23 ], [ 24 ]
[ 20 ], [ 21 ], [ 22 ], [ 23 ], [ 24 ]
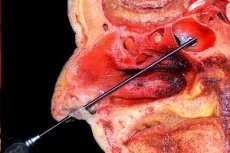
Surgical treatment of chronic sphenoiditis
Treatment of acute sphenoiditis includes probing of the sphenoid sinus with catheter needles. Preliminary surgical correction of the nasal cavity structures (nasal septum deformities, hypertrophy of the posterior end of the middle turbinate, adhesions, adenoids) that prevent sedation should be performed. Careful step-by-step superficial anesthesia and anemization of the mucous membrane of the middle nasal passage are performed. The anatomical landmarks are the lower edge of the piriform opening, the upper edge of the choana, the middle turbinate and the nasal septum. Probing is performed along the Zuckerkandl line, which starts from the anterior nasal spine, passes through the middle of the middle turbinate to the middle of the anterior wall of the sphenoid sinus. It should be remembered that the outlet opening of the sinus is 2-4 mm lateral to the nasal septum and 10-15 mm above the edge of the choana. A sign of entry into the lumen of the sinus through the natural outlet is the sensation of "falling through" and the impossibility of vertical displacement of the catheter. After aspiration of the contents, the cavity is washed with antiseptic solutions or a warm 0.4% sodium chloride solution. Then the patient is placed on her back with her head slightly thrown back, the drug is introduced into the lumen of the sphenoid sinus and left for 20 minutes for maximum absorption of the drug.
The tactics of treating chronic sphenoiditis are determined by the clinical form of the disease. Exudative forms (catarrhal, serous, purulent) are treated conservatively with probing and prolonged drainage, constant administration of drugs into the sphenoid sinuses. Productive forms (polypous and polypous-purulent) are subject to surgical treatment.
The most gentle typical method of opening the sphenoid sinus is transseptal. After a typical incision, the mucoperichondrium is exposed to the quadrangular cartilage. Only its altered sections are removed, as is the case with the bone part, where the sections located on the way to the rostrum are resected. The mucous membrane and periosteum of the anterior wall of the sphenoid sinus are peeled off, which is opened with Hayek's pincers. Pathologically altered sections of the mucous membrane, polyps and other formations are removed. The operation is completed by washing the sinus with the imposition of a wide anastomosis and tamponade of the nasal cavity.
In the endonasal opening of the sphenoid sinus by the Hayek method modified by Bockstein, most of the anterior part of the middle nasal concha is resected, then the posterior cells of the ethmoid sinus are opened. After the removal of bone fragments, the anterior wall of the sphenoid sinus is visualized. The anterior wall is broken with a hook inserted into its natural outlet, and the opening is widened with Hayek forceps.
When performing endonasal opening of the sphenoid sinus using endoscopes or under microscope control, the use of a microdebrider is considered more gentle.
Surgical treatment of chronic sphenoiditis is aimed primarily at creating a wide drainage opening for the sphenoid sinus, which in itself can lead to the elimination of the inflammatory process. If there are pathological tissues in the sinus (polyps, granulations, areas of necrotic bone, detritus, cholesteatoma masses), they are subject to removal, while observing the principle of preserving areas of the mucous membrane capable of reparative processes.
Indications for surgical treatment of chronic sphenoiditis are determined by the duration of the disease, its combination with inflammatory processes in other paranasal sinuses, ineffectiveness of non-surgical and semi-surgical treatment, the presence of pronounced subjective and objective symptoms, including nasal polyposis, signs of visual impairment, suspicion of orbital and intracranial complications. When determining indications for surgical treatment, one should also be guided by the position of old authors that any chronic sphenoiditis is a "powder keg" on which the brain "sits", "smoking a cigar" due to insufficiently attentive attitude to this disease of both the patient and the attending physicians.
There are quite a lot of surgical treatment methods, all of them are differentiated by the nature of access to the sphenoid sinus and are divided into the following methods:
- direct endonasal ethmoidosphenoidectomy;
- transsinomaxillary ethmoidosphenoidectomy;
- transorbital ethmoidosphenoidectomy;
- transseptal sphenoidectomy.
Since the isolated form of chronic sphenoiditis is extremely rare and is often accompanied by disease of other paranasal sinuses, the most frequently and most effectively used method is that of Pietrantonide Lima, which allows for a single access through the maxillary sinus to revise all sinuses on one side, including the main one, without affecting or destroying the anatomical structures of the internal nose, as, for example, with endonasal and transseptal methods. Opening the sphenoid sinus is rarely performed as an independent operation; most often, the sphenoid sinus is opened together with the ethmoid labyrinth.
The Pietrantoni-de Lima Method
This method ensures the opening and drainage of all paranasal sinuses in case of geminal sinusitis while preserving the nasal turbinates and restoring the physiological functions of the nasal cavity.
Indications: chronic pansinusitis (simple and complicated by orbital phlegmon, optic neuritis, optic-chiasmatic arachnoiditis, meningitis, cavernous sinus thrombophlebitis, brain abscess - temporal and parietal lobes - as well as visceral toxic infections).
The operational technique includes the following stages:
- opening of the maxillary sinus using the Caldwell-Luc method;
- opening of the ethmoid labyrinth in the area of the posterior-superior-inner angle of the maxillary sinus;
- removal of the anterior and posterior cells of the ethmoid labyrinth (dissection of the ethmoid labyrinth according to Jansen-Winkler);
- trepanation of the anterior wall of the sphenoid sinus, starting from the crest of the sphenoid bone;
- endonasal opening of the frontal sinus (as indicated) and formation of wide drainage of all opened sinuses;
- examination of the general postoperative cavity, its pulverization with a powder mixture of antibiotics;
- tamponade of all opened sinuses with a single tampon, starting from their deepest sections; the length of the tampon is calculated so that its end extends beyond the incision of the nasolabial fold in the vestibule of the mouth, through which it will subsequently be removed.
Transseptal opening of the sphenoid sinus according to Hirsch
This method is the most convenient in terms of surgery, providing a good overview of the surgical site in the sphenoid sinus, wide opening of both its halves, the most radical removal of pathological contents and ensuring its stable effective drainage. The effectiveness of surgical intervention is significantly increased by using video endoscopic technology in the final part, which allows identifying on the monitor screen and eliminating all, even the most insignificant, fragments of pathological tissues, while observing the principle of sparing viable areas of the mucous membrane. In addition, this method allows reaching the pituitary gland in case of its tumors.
Operational technology:
- Incision and separation of the mucous membrane with the perichondrium, as in the septum operation up to and including the vomer; moving the mucoperichondrium plate to the lateral side.
- Mobilization of the cartilaginous part of the nasal septum to the opposite side, for which V.I. Voyachek proposed making incisions (breaks) on the cartilaginous part of the nasal septum without cutting the perichondrium and mucous membrane of the opposite side; if it is necessary to expand access to the anterior wall of the sphenoid sinus, it is permissible to remove only individual sections in the cartilaginous section, especially those curved and interfering with orthograde access to the sphenoid sinus. In the bony section of the nasal septum, only those sections that are on the way to the rostrum of the sphenoid sinus are removed. A.S. Kiselev (1997) draws special attention to the need to preserve the upper part of the perpendicular plate of the ethmoid bone as a median landmark (the lower part is removed to expand access to the rostrum of the sphenoid sinus).
- Insertion of Killian's mirrors with successively longer branches between the nasal septum and the mucoperichondrium to the anterior wall of the sphenoid sinus and its opening with an extended West chisel, forceps or burr. In the absence of a video monitoring device with fiber optics, the condition and volume of the sinus, its contents, the presence and position of the intersinusal septum are checked using a button probe, successively palpating all its walls, paying special attention to the upper and lateral ones.
- The opening in the sphenoid sinus is widened using convenient instruments (long chisels, spoons, long rotating Gaek forceps). After removing a significant portion of the anterior wall of the sphenoid sinus and dissecting the mucous membrane behind it, a large portion of the intersinusal septum is also bitten off.
- Revision and curettage of the mucous membrane, while observing the principle of its sparing. This stage of the operation is most effective in relation to both the preservation of viable areas of the mucous membrane and the total removal of non-viable tissues using the microvideo surgical method with the display of the surgical field on the monitor screen.
- Reposition of parts of the nasal septum by removing the Killian mirror. A subclavian catheter of the appropriate length is inserted into the sinus for subsequent care (rinsing with ozonized distilled water, administering medications) and anterior loop tamponade of both halves of the nose is performed, as after septum-oneration. The tampons are removed after 24-48 hours, the catheter - after a week.
Postoperative treatment
For a week, general and local antibiotic therapy is carried out, daily rinsing of the sinus with antiseptic solutions, general symptomatic treatment, and drugs are prescribed that increase the specific and non-specific resistance of the body.
Endonasal polysinusotomy
A.S. Kiselev described this type of operation as "modern", which was probably dictated by his own extensive experience. The operation is preceded by a detailed examination of the nasal cavity using modern endoscopic equipment. The purpose of this examination is to identify endonasal anatomical features that must be taken into account during the operation, and if violations are detected that may interfere with the endonasal access to the sphenoid sinus, a plan for their elimination is outlined. Such violations and pathological conditions include a pronounced curvature of the nasal septum, especially in its deep sections, the presence of hypertrophied nasal turbinates, especially middle ones, polyps, especially choal localization, as well as a number of dysmorphological phenomena that can significantly interfere with orthograde penetration to the rostrum.
If there are no mechanical obstacles to performing this surgical intervention, the next step is luxation of the middle nasal concha to the nasal septum to identify the uncinate process by palpating it with a button probe. Behind the process, the anterior wall of the ethmoid bulla is determined, which together with it forms a semilunar fissure. Next, with a sickle-shaped knife, with a top-down movement, the uncinate process is cut off and removed with nasal forceps. Removal of the uncinate process opens access to the bulla, which is opened with the same forceps or another convenient instrument. Opening the bulla provides access to the remaining cells of the ethmoid labyrinth, which are sequentially removed, which leads to exposure of the "roof" of the ethmoid bone. When moving the instrument in the medial direction and with excessive force directed upward, there is a risk of damaging the ethmoid plate and penetrating the anterior cranial fossa. Conversely, excessive lateral displacement of the instrument may result in damage to the paper plate and orbital contents.
The next step is to widen the maxillary sinus ostium, for which the end of the endoscope with a 30° viewing angle is inserted into the middle nasal passage and the natural ostium of the maxillary sinus is found using a button probe. It is located posterior to the upper edge of the inferior turbinate and anterior to the level of the lacrimal tubercle; its diameter is normally 5-7 mm. Next, using special pliers with a reverse nipper or a curette and a sharp spoon, widen the natural ostium. However, it should be borne in mind that widening the ostium beyond the level of the lacrimal tubercle usually results in damage to the lacrimal ducts, and posterior to the level of the posterior end of the middle turbinate may result in damage to the sphenopalatine artery (a. sphenopalatine). Excessive upward widening of the ostium may result in penetration into the orbit.
The next stage is opening the sphenoid sinus, which is done through its anterior wall using bone forceps. The resulting opening is widened using Gaek's nippers. After this, the sinus is examined using an endoscope and curettage is performed, observing the principle of sparing the mucous membrane.
Next, an intranasal opening of the frontal sinus is performed, which, according to A.S. Kiselev, is the most complex type of endonasal sinusotomy. After preliminary removal of the bone shaft and opening of the anterior cells of the ethmoid labyrinth, which form the anterior wall of the frontonasal canal, the entrance to the frontal sinus becomes visible, into which a probe is inserted for orientation. In order to widen the entrance to the frontal sinus, it is necessary to remove the frontonasal bone mass, which poses the risk of penetration into the anterior cranial fossa, especially in case of developmental anomalies of the frontal bone. Therefore, if it is not possible to insert a probe into the frontal sinus, it is necessary to abandon its intranasal opening and, if there are appropriate indications, to switch to external access to it.
Further management
Self-rinsing of the nasal cavity and nasopharynx with a warm 0.9% sodium chloride solution using devices such as "Rinolife" or "Dolphin".
Approximate periods of disability in acute and exacerbation of chronic sphenoiditis without signs of complications in the case of conservative treatment with sinus probing are 8-10 days. Endonasal intervention extends the treatment period by 1-2 days.
Information for the patient
- Beware of drafts.
- Get vaccinated against influenza.
- At the first signs of acute respiratory viral infection or flu, consult a specialist.
- Upon recommendation of the attending physician, perform surgical sanitation of the nasal cavity to restore nasal breathing and correct the anatomical structures of the nasal cavity.
Drugs
Forecast
The prognosis of chronic sphenoiditis is favorable in most cases, even with some intracranial complications, if they are detected in time and radical treatment is carried out. The most dangerous in functional terms are rapidly progressing orbital phlegmon, optic neuritis, and optic-chiasmatic arachnoiditis. The prognosis is very serious, and in some cases pessimistic, with paraventricular and brainstem abscesses, rapidly progressing thrombophlebitis of the cavernous sinuses with its spread to neighboring venous systems of the brain.

