Medical expert of the article
New publications
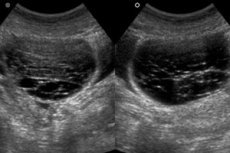
Corpus luteum cyst in pregnancy
Last reviewed: 29.06.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
The corpus luteum or corpus luteum is a gland that synthesizes progesterone, and arises in place of a burst dominant follicle. This formation prepares a woman's body for conception, pregnancy and, if it occurs, supports during the first four months of gestation, until the placenta is formed and does not take over the functions of progesterone synthesis. After which the luteal gland normally regresses.
A corpus luteum cyst in pregnancy can form in the first trimester and, for some reason, the process of reverse development may be delayed. Basically, there is nothing terrible in this. Usually such functional neoplasms spontaneously regress and do not cause serious discomfort. But sometimes a woman may encounter complications.
Epidemiology
Statistical data are not uniform. Some data say that ovarian cysts of all types are detected in one out of a thousand expectant mothers, while other sources mention the frequency of cystic neoplasms in two or even three pregnant women out of a thousand.
There are reports that cysts are detected more frequently in pregnant women of older fertile age.
Risk factors
Disrupt the harmonious work of the hormonal system, especially in the first trimester of pregnancy, when it is already unstable, can any external influence:
- Unfavorable environmental conditions;
- Physical overload;
- Psycho-emotional trauma.
Blood circulation and lymph flow in the organs of the genital system are disturbed under the influence of many internal causes that provoke the appearance of cysts in the first weeks of pregnancy, when there is a weakening of the immune system. Risk factors are the presence of the future mother:
- Chronic inflammatory ovarian disease;
- Acute infections or nonspecific inflammation;
- Of abortions in the past;
- First pregnancy after the age of 35-40;
- Ovarian cysts in close female relatives.
Pathogenesis
It is hypothesized that a combination of internal and external causes is a provoking factor for the development of corpus luteum cysts in pregnancy. It is assumed that the result of this effect is an increase in the synthesis of female sex hormones - estrogen and progesterone, which inhibits the regression of the corpus luteum. Then at the location of the last ruptured follicle begins to collect serous fluid, that is, a cyst is formed. Most often, a capsule with liquid contents measuring more than three centimeters is found in one of the ovaries.
Symptoms of the corpus luteum cysts in pregnancy
In the vast majority of cases, there are no first signs, as the cysts do not manifest themselves in any way. Women do not consult a doctor because they have no complaints and do not experience any discomfort.
Therefore, as a rule, the diagnosis of "cyst of the corpus luteum in pregnancy" is established at a routine ultrasound early in pregnancy.
Extremely rarely still, the expectant mother experiences unpleasant symptoms. This is usually due to the large size of the cystic capsule, which puts pressure on adjacent organs.
There may be complaints about:
- Aching pain on one side of the lower abdomen, although it happens that it is difficult for a woman to specify the localization of the pain, because the pulling sensations are widespread (such pains usually appear after sex or physical activity, at rest can pass and arise again);
- Pressing discomfort, a feeling of heaviness, bloating;
- Constipation;
- Frequent urination;
- Discomfort and soreness only occurs when emptying the bowel and/or bladder.
Complications and consequences
The cyst of the corpus luteum in pregnancy almost never poses a threat to the health of the owner and the development of the child. In most cases, it regresses without intervention towards the end of the first trimester or the beginning of the second trimester.
Nevertheless, even if extremely rare, complications can occur. Sometimes patients complain that the cyst of the corpus luteum hurts during pregnancy. This is not a favorable symptom, about which it is necessary to notify the doctor leading the pregnancy.
Significant hormonal imbalance can cause rapid growth of a cystic mass, which can have the following consequences:
- From the strong stretching of the walls of the capsule may rupture the corpus luteum cyst in pregnancy;
- Also happens to twist the stem of the cyst.
Rupture of the corpus luteum can occur throughout a woman's reproductive years, [1] but is more common in younger women between the ages of 16 and 30. [2], [3] Because of the abdominal pain accompanied by hemoperitoneum, corpus luteum rupture is easily confused with an ectopic pregnancy, especially when the corpus luteum that supports an intrauterine pregnancy ruptures.
When apoplexy (damage) to the cyst occurs, symptoms become vivid.
Characterized by the following:
- Sharp pain in the lower abdomen;
- Nausea, possible vomiting,
- Pre-syncope caused by a sudden drop in blood pressure;
- There may be bloody vaginal discharge.
The appearance of such symptoms requires emergency medical intervention. Complications associated with untimely treatment are necrosis and peritonitis.
Diagnostics of the corpus luteum cysts in pregnancy
No tests do not detect the presence of cystic formation. They are prescribed to assess the general condition of the expectant mother or as an additional diagnosis:
- Clinical blood test - if inflammation, rupture or torsion of the cyst pedicle is suspected;
- A blood chemistry test to determine the presence and level of oncomarkers HE-4 and CA-125, usually synthesized by cancer cells.
A corpus luteum cyst in pregnancy is detected most often at the first scheduled ultrasound examination - this is the main instrumental diagnosis in this case. A corpus luteum cyst on ultrasound looks like a cavity with fluid inside.
Ultrasound screenings are considered safe for the expectant mother and fetus, so if a neoplasm is detected, they are scheduled regularly to have information about the dynamics of its development. The size of the cyst of the corpus luteum in pregnancy can be different. Mostly they grow up to five centimeters. Such cysts do not manifest themselves with symptoms and, usually, regress independently. Larger formations can cause some discomfort, usually alarmed by the rapid growth of the cyst. Then ultrasound with Doppler ultrasound is appointed. However, the decision to take any action is made solely by the doctor.
It is impossible to determine in advance what may happen to the cyst throughout the pregnancy. According to ultrasound and localization, even the type of cyst is only assumed. Based on the nature of the complaints and the results of ultrasound monitoring, the doctor makes a hypothetical prognosis and continues monitoring. functional cysts, usually regress by the end of 16 weeks of gestation, but sometimes persist until delivery.
Early detected masses are usually differentiated with ectopic pregnancy.
Differential diagnosis
The differential diagnosis, in cases where the cyst has not regressed at term, is made with endometrioma, cystadenoma or dermoid cyst. In pregnant women, due to high levels of progesterone, the walls of the cyst have a very unusual appearance due to decidualization, and ultrasound alone may not be enough, so additional studies may be prescribed to rule out malignancy.
Who to contact?
Treatment of the corpus luteum cysts in pregnancy
A corpus luteum cyst in pregnancy usually has no pathologic effect on its course and the developing fetus. In the vast majority of cases, such formations regress independently by the time of formation of a full-fledged placenta, by the 12th, maximum - by the 16th week of gestation.
When a cyst is detected, the doctor usually takes a wait-and-see attitude towards the pregnant woman - observes her well-being and monitors the size of the mass with the help of ultrasound screenings. Small cysts (up to 5cm) that do not cause discomfort to the future mother and do not show rapid growth, just observe. In case of progesterone deficiency, hormonal drugs containing progesterone may be prescribed. Even if the cyst does not dissolve in time, it is not touched. Sometimes women give birth safely with a cyst of the corpus luteum.
However, if the neoplasm is large, rapidly growing, suppuration or signs of malignancy, surgical treatment may be prescribed. Pregnant women undergo surgery only on strict indications. Emergency - in case of "acute abdomen" - cyst rupture or torsion of its legs, planned - in case of danger of developing such conditions.
Scheduled surgeries are not performed at early gestation. If intervention is necessary, a woman is operated on at 14-16 weeks of gestation preferably by the method laparoscopy as less traumatic.
If a large cyst or its rupture (twisting) is detected at a late stage, or if there are strong suspicions of a malignant process, surgical delivery may be ordered by means of cesarean section, during which the cyst is also removed.
Prevention
Women planning a pregnancy are advised to do pelvic ultrasound to rule out the presence of cysts even before the onset of pregnancy.
If the cyst of the corpus luteum is detected early in pregnancy, it is not a cause for concern, but the woman needs to regularly monitor her condition in a medical institution in order to prevent complications. If a cystic formation is detected, the future mother is advised to avoid excessive physical activity, lifting and carrying heavy weights, violent sexual pleasures and other sudden movements.
Forecast
In most cases, the cyst of the corpus luteum in pregnancy has a favorable prognosis for mother and child.
At the same time, it is impossible to assume in each specific case, how the neoplasm will behave under the influence of changing hormonal background. Therefore, a woman should be under the control of a specialist. Dynamic monitoring of her condition is also a guarantee of a favorable outcome of pregnancy.

