Medical expert of the article
New publications
Fetal egg detachment in early pregnancy
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
One of the problems that arise in the early stages of pregnancy is the detachment of the ovum. Let's consider the main causes of the pathology, symptoms, and treatment methods.
The first trimester of pregnancy is an important period for both the mother and the future child. At this time, the key organs and systems of the baby are laid down and a large number of spontaneous miscarriages occur. One of the reasons for the termination of pregnancy is the detachment of the ovum.
The uterus is a muscular organ that contracts periodically. During pregnancy, the fertilized egg attaches to its walls and develops. At this point, the placenta, or chorion, is formed. It is a villous membrane of the embryo covering the surface of the egg. Through the chorion, the fetus receives oxygen and all nutrients. The formation of a full-fledged placenta is observed at the end of the first month after conception.
Fertilized egg:
- It is an egg cell fertilized by a sperm that is attached to the walls of the uterus.
- It is the beginning of the embryonic development of the fetus and is the first structure determined by ultrasound.
- A month after conception, a yolk sac is detected in the egg, the presence of which indicates a healthy pregnancy.
- It has a round or oval shape, which gradually increases in size, which allows you to determine the exact period of gestation and identify possible disorders.
Unlike the uterus, the chorion does not contract, so if the organ contracts strongly in the early stages, partial or complete detachment occurs. This problem occurs in 2% of all pregnancies and varies in severity and symptoms. [ 1 ]
The term detachment implies two conditions: immediate detachment (early stages) and critical condition (middle or end of pregnancy). In the first case, it is an alarming signal about a possible miscarriage.
Epidemiology
According to the International Classification of Diseases ICD-10, spontaneous miscarriage belongs to category XV Pregnancy, childbirth and the postpartum period (O00-O99):
- O03 Spontaneous abortion.
- O02.1 Missed abortion.
- O20.0 Threatened abortion.
According to medical statistics, about 10-15% of all pregnancies end in early miscarriage. Moreover, more than 50% of sporadic (accidental) miscarriages are associated with genetic abnormalities of the fetus. [ 2 ]
The detachment of the ovum is closely related to the age of the pregnant woman; the older the woman, the higher the risk of abortion:
- Up to 35 years old – 15%
- 35-45 years old – 20-35%
- Over 45 years old – 50%
- History of miscarriages – 25%
Due to the action of certain factors, the embryo dies, and then the detachment of the fertilized egg from the uterine walls begins. During this period, the woman experiences bloody discharge, as the detachment is removed from the uterine cavity. To confirm spontaneous abortion, a quantitative determination of beta-hCG and ultrasound diagnostics are performed. [ 3 ], [ 4 ]
Causes early pregnancy detachments
There are many factors that can provoke the discharge of the fertilized egg in the first trimester. Most often, the pathological condition is associated with the following reasons:
- Hormonal disorders.
- History of abortions.
- Diseases of the reproductive system.
- New growths.
- Inflammatory pathologies of the pelvic organs.
- Anomalies of the female genital organs.
- Viral and infectious diseases during pregnancy.
- STDs.
- Arterial hypertension.
- Increased physical activity.
- Hereditary pathologies.
- Rhesus conflict between mother and fetus.
- Disturbances in the development of the placenta and embryo.
- Bad habits of women: smoking, drug addiction, alcoholism.
- Negative impact of environmental factors.
Most often, the cause of detachment is progesterone deficiency. With this pathology, the female body does not produce a sufficient amount of progesterone, which is responsible for the normal bearing of a child. [ 5 ]
Risk factors
The risk of detachment of the ovum in the early stages of pregnancy increases significantly when the body is exposed to the following factors:
- Stress and emotional experiences.
- Age over 35 years.
- Exhausting physical activity.
- Bad habits.
- Rhesus conflict.
- Tumor neoplasms.
- Progesterone deficiency.
- Diseases of pregnant women: venereal, infectious, viral, inflammatory.
- Taking certain medications.
- Hereditary pathologies and others.
Any of the listed factors can cause spontaneous termination of pregnancy. A high risk of miscarriage is typical for the period when the placenta is not yet fully formed, that is, from the first days of fertilization until the 16th week. During this period, a woman should protect herself as much as possible from the effects of any pathological factors. [ 6 ]
Pathogenesis
The mechanism of development of spontaneous miscarriage in the early stages of gestation is associated with many factors. The pathogenesis of detachment can be caused by such viruses in a woman: cytomegalovirus, herpes, parvovirus, rubella. Another possible cause of miscarriage is chromosomal or hereditary pathologies.
Let us consider the etiopathogenesis of the main causes of ovum detachment:
- Uterine pathologies – anomalies in the development of the Müllerian duct, synechia of the uterine shelf, uterine hypoplasia, organ damage due to abortion, isthmic-cervical insufficiency,
- Endocrine diseases – ovarian hypofunction, luteal insufficiency, adrenal hyperandrogenism, hyperthyroidism, hypothyroidism, diabetes. Disorders in the functioning of the ovaries, adrenal glands and other endocrine glands. In this case, miscarriage can occur both with spontaneous conception and with drug-induced pregnancy.
- Chromosomal abnormalities – structural disorders, quantitative aberrations of chromosomes. Disorders of cellular and humoral immunity in women, isoserological incompatibility by blood group and Rh factor of mother and fetus.
- Intoxication of the body - the greatest danger is poisoning with lead, mercury, gasoline, nicotine and other toxic substances. Early miscarriages are typical for women exposed to ionizing radiation or working in the chemical industry.
- Isoantigenic incompatibility of fetal blood - with this anomaly, fetal antigens penetrate the placenta into the woman's body and provoke the formation of specific antibodies. This can lead to hemolytic disease, intrauterine fetal death and other pathologies.
- Diseases and abnormalities in the development of the genitals. For example, with uterine myoma, implantation of the fertilized egg can occur on the myomatous node, which is a thinned mucous membrane. Because of this, the embryo does not receive sufficient nutrition and cannot fully develop.
- Abortions in the anamnesis – artificial termination of pregnancy causes disorders of the nervous and endocrine systems. Against this background, the development of inflammatory diseases, chronic endometritis is possible. During instrumental removal of the fetus during dilation of the cervix, damage to its muscular structures is possible. This entails insufficiency of the isthmic-cervical canal and miscarriage of all subsequent pregnancies.
- Infectious diseases – miscarriage can be caused by both chronic infections and local lesions of the genitals by bacterial flora, viruses, fungi and other pathogens. Inflammatory lesions of the genitals lead to disruption of the structure and functions of the main layers of the endometrium and myometrium. This causes adhesions, tumors in the small pelvis, fixed retroflexion and other pathologies that disrupt fetal growth.
Psychogenic factors, the action of which increases the risk of miscarriage, should also not be excluded. Any of the above causes leads to increased contractile activity of the uterus and detachment of the ovum. If a miscarriage occurs at the beginning of the first or second trimester, the ovum is separated from the uterus without rupture of the amniotic sac. [ 7 ]
Symptoms early pregnancy detachments
The symptoms of spontaneous abortion are manifested by a deterioration in the woman's health. During this period, the chorion detaches, the vessels through which it was introduced into the uterus rupture and a hematoma forms.
The main symptoms of miscarriage include:
- Back pain similar to menstrual cramps.
- Cramping attacks in the lower abdomen.
- Bloody discharge with clots, indicating the removal of a detached fertilized egg from the uterine cavity.
- Decreased or complete absence of signs of pregnancy: nausea, chest pain, mood changes, etc.
In most cases, early abortion begins with spotting, which turns into bleeding. Such symptoms are a reason to seek emergency medical care.
First signs
Spontaneous miscarriage can occur at any stage of pregnancy, but most often it happens in the first months of gestation. In the first trimester, there is a high risk of developing a retrochorial hematoma.
The first signs of fetal abruption:
- Cramping pain in the lower abdomen.
- Nagging pain in the lower back.
- Bright red or dark vaginal discharge.
- Feeling of uterine spasms.
- Heavy bleeding with clots.
If the hematoma has not begun to empty, then there is no discharge, the woman complains of pain and a general deterioration in health. The appearance of brown discharge indicates a decrease in the hematoma and is a reason for consultation with a gynecologist. In 30% of cases, miscarriage is asymptomatic and can only be diagnosed with the help of a screening ultrasound examination. [ 8 ]
Stages
There are several stages of detachment of the ovum:
- Threatened abortion - the woman feels pain, there is minor bloody discharge from the vagina. If you seek medical help in a timely manner, there is a chance to save the pregnancy.
- Miscarriage has begun - pain combined with bloody discharge. There is still a chance to save the pregnancy.
- Abortion on the go - sharp pains, profuse bloody discharge with clots. Pregnancy cannot be saved.
- A completed abortion – the fertilized egg is completely removed from the uterine cavity, and bleeding stops.
Rejection of the fetal formation before 12 weeks is called an early miscarriage, and spontaneous abortion before 22 weeks is called a late miscarriage. [ 9 ]
Forms
According to the studies, the fetal membranes separate in different ways. Therefore, there are several types of spontaneous termination of pregnancy in the early stages, let's consider them:
- Biochemical pregnancy - rejection occurred before the delay of menstruation. The ultrasound does not detect the fetal egg, but the hCG test shows elevated levels. Most often, such detachment is associated with defects in the fetal egg or hormonal disorders in the woman.
- Complete detachment - the fetal membranes have separated from the uterine walls, the embryo has died. The uterus contracts and gets rid of the fetus. The woman feels a nagging pain in the lower abdomen, which radiates to the sacrum and lower back. Heavy bleeding is possible.
- Incomplete abortion – when part of the fertilized egg passes away, tissues remain in the uterus that disrupt its contraction and hemostasis. Because of this, there is a risk of severe bleeding and hemorrhagic shock. Even if the bleeding is minor, the risk of its aggravation remains due to the remaining parts of the fertilized egg, infection, or the formation of a placental polyp.
- A failed miscarriage - the fertilized egg stops developing but is not rejected. It undergoes resorption and goes through several stages: blood, flesh, lithonedione (petrification). This anomaly can occur at any stage of gestation. The diagnosis is based on bleeding with non-coagulable blood. Such pregnant women may have a history of angina paroxysms.
- Cervical pregnancy – the fertilized egg develops in the cervical canal, i.e. in the area of its isthmus. Rejection occurs at 4-6 weeks of gestation. The woman experiences profuse bleeding, which is life-threatening. Hysterectomy and blood replacement therapy are performed for treatment.
- Septic (febrile) abortion is a serious condition caused by primary or secondary immunodeficiency. The detachment is associated with the penetration of superinfection with antibiotic-resistant flora into the vagina and uterus. The woman complains of general weakness, hyperthermia, tachycardia, acute pain in the lower abdomen, bloody-purulent discharge from the genital tract. The pregnant woman needs emergency medical care and hospitalization.
Regardless of the type of spontaneous miscarriage, a woman needs medical and psychological help.
Complications and consequences
The risk of complications after a miscarriage depends on many factors. First of all, it is the period at which the rejection of the fertilized egg occurred, the woman's age, the type of spontaneous abortion, etc.
The main consequences of this pathology include:
- An incomplete abortion, in which part of the fertilized egg and placenta remain in the uterus. This is dangerous due to severe bleeding and infection syndrome.
- Infectious and inflammatory diseases of the reproductive system.
- Hormonal disorders.
- Difficulties with further conception and bearing a fetus.
- Hematometra is a disorder of blood evacuation from the uterine cavity. Due to poor contractility or spasms of the cervix, blood clots accumulate in it. The woman complains of acute pain in the lower abdomen and a feeling of distension, there is no bloody discharge.
- Menstrual cycle disorders.
- Isthmic-cervical insufficiency.
- Cervical erosion.
- Placental polyp - when the ovum is not completely detached, part of the placenta remains in the uterus, which over time grows into connective tissue and is tightly attached to the walls of the organ. The woman suffers from pain and periodic spotting, which can develop into heavy bleeding.
- Psychological problems, depression. [ 10 ]
In most cases, the consequences of detachment of the ovum in the early stages of gestation do not pose a danger to the life and health of the woman. To prevent possible complications, gynecologists recommend mandatory curettage of the uterus and a control ultrasound examination after 2-3 weeks.
Diagnostics early pregnancy detachments
To assess the patient's condition and diagnose spontaneous miscarriage, anamnesis is collected, complaints are analyzed, physical examination and a set of additional studies are performed. A primary assessment of hemodynamic parameters is mandatory.
- Analysis of complaints and collection of anamnesis - features of the menstrual cycle, previous pregnancies and abortions, gynecological diseases, ultrasound results. The presence of symptoms of early pregnancy: bloody discharge from the vagina, pain in the lower abdomen and lower back, delayed menstruation. Urine test for hCG.
- Physical examination – temperature, blood pressure, heart rate. Examination and palpation of the abdomen (pain, bloating, tension of the muscles of the anterior abdominal wall), vaginal examination (examination with speculums to determine the source and assess the volume of bleeding). Bimanual assessment of the consistency and length of the cervix, the condition of the cervical canal, soreness of the appendages and vaginal vaults.
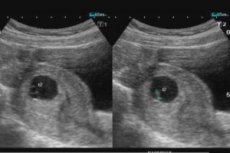
- Instrumental examination of the pelvic organs (transvaginal or transabdominal ultrasound) and laboratory tests.
A comprehensive diagnostic approach makes it possible to detect the detachment of the ovum at an early stage and, if possible, prevent a complete miscarriage. Also, timely seeking medical help helps to avoid serious complications in the case of incomplete detachment of the embryo. [ 11 ]
Tests
Laboratory tests in combination with ultrasound results allow diagnosing a miscarriage. The tests that the patient must take are:
- Clinical blood test.
- Determination of hCG levels.
- Determination of blood type (if there is a risk of blood loss).
- STD testing.
- Analysis for infectious diseases.
- Microscopic examination of cervical discharge.
Analysis of human chorionic gonadotropin is a hormone formed after the implantation of the embryo in the uterine cavity. After a miscarriage, the level of hCG is elevated, which allows for the diagnosis of spontaneous abortion. Analysis for infectious diseases and other laboratory studies allow us to determine what caused the miscarriage and, if possible, prevent miscarriages in future pregnancies. [ 12 ]
Instrumental diagnostics
In case of early pregnancy loss, a transvaginal or transabdominal ultrasound is performed to detect signs of detachment of the ovum and retention of its remains in the uterus. The first ultrasound is a study through the vagina using an endovaginal sensor, which allows for a detailed examination of the structure of the uterus and ovaries.
If transvaginal examination is impossible, transabdominal examination is indicated. It is performed with a full bladder. It allows to study the condition of the pelvic organs, uterus and appendages, to identify pathologies of the reproductive organs.
Possible research results:
- Complete abortion – average internal diameter of the ovum >20-25 mm, embryo is not visualized. Endometrial thickness is less than 15 mm, remaining products of conception were previously identified.
- Non-viable pregnancy – embryo >7-8 mm, heartbeat not visualized.
- In an incomplete miscarriage, there is tissue in the uterus with a diameter of more than 15 mm.
- Ectopic pregnancy - the uterine cavity is empty, but enlarged in size, as are the appendages. There are signs of endometrial hyperplasia.
- Septic miscarriage – signs of complete or incomplete abortion, ascending infectious lesion of the uterine cavity and its appendages, peritoneum, pelvic abscess.
If a woman has a long or irregular menstrual cycle, a repeat ultrasound is indicated a week after the first.
Differential diagnosis
A mandatory component of examinations for rejection of a fetal formation in the early stages of pregnancy is differential diagnostics.
Miscarriage is differentiated from the following pathologies:
- Neoplasms of the vagina and cervix. Abundant bloody discharge may indicate ectropion, i.e. eversion of the mucous membrane of the cervical canal. To detect the disease, a speculum examination and colposcopy are performed.
- Another possible cause of vaginal bleeding is an anovulatory cycle, which often involves delays in menstruation. For diagnosis, an hCG test (negative) and a bimanual examination of the uterus are performed.
- Differentiation is carried out with hydatidiform mole. With this pathology, discharge in the form of bubbles appears, and the size of the uterus is larger than the expected gestation period. Ultrasound is indicated to confirm the diagnosis.
- With an ectopic pregnancy, there are bloody discharges, sharp pains, a feeling of pressure on the bladder. The hCG test is positive. Bimanual diagnostics reveals pain when moving the cervix. The organ is smaller in size than it should be at the expected pregnancy period. When palpating the fallopian tubes, thickening and bulging of the vaults is possible. An ultrasound scan reveals a fertilized egg in the fallopian tube. When it ruptures, blood accumulates in the abdominal cavity.
The results of differential diagnostics allow us to make a final diagnosis regarding spontaneous abortion in the early stages. [ 13 ]
Who to contact?
Treatment early pregnancy detachments
If suspicions of abruption of the ovum are confirmed, the woman is sent to the hospital. A pregnancy that can be saved requires inpatient treatment and medical supervision, so the patient is hospitalized. The main goal of treatment is to relax the uterus, stop bleeding and prolong gestation, provided the embryo/fetus is viable.
At this stage, the woman should be provided with complete rest, both physical and emotional. Even too active intestinal peristalsis is dangerous, so a dietary diet is recommended, refusing products that weaken or provoke flatulence. Sexual intercourse is also prohibited. [ 14 ]
An obligatory component of therapy is medications that stop bleeding, reduce uterine tone and relieve pain. But when using medications in the first trimester, the risk of their teratogenic and embryotoxic effects should be taken into account. [ 15 ]
Medicines
In most cases, early ovum detachment requires medication. The doctor selects medications based on the pregnant woman's condition, type of rejection, period, and general health.
- Hormonal therapy is often used in cases of threatened or started miscarriage. In cases of previously diagnosed corpus luteum insufficiency, gestagens are used: Allylestrenol, Turinal. But such drugs are contraindicated for women with adrenal hyperandrogenism, so they are prescribed corticosteroids: Prednisolone, Dexamethasone.
- Progesterone preparations have a positive effect on the hormonal status of the pregnant woman and eliminate the threat of miscarriage. Most often, patients are prescribed Acetomepregenol.
- For women with uterine developmental abnormalities, hypoplasia, and ovarian hypofunction, in addition to gestagens, estrogens are prescribed: Ethinyl estradiol, Microfollin, Folliculin, Estradiol dipropionate.
- For patients with correctable ovarian hypofunction, the drug Choriogonin is used against the background of therapy with gestagens and estrogens.
- When detachment with bleeding has begun, Ascorutin, Dicynone, and Etamsylate are used.
- In case of incomplete abortion, intravenous drip administration of Oxytocin or Prostaglandin F2 can be used to remove the fertilized egg.
- In case of prolonged bleeding after emptying the uterus, it is recommended to use drugs that promote contraction of the organ: Methylergometrine, Ergotal, Ergotamine hydrotartrate. These drugs are administered subcutaneously, intramuscularly, slowly into a vein or the cervix.
Let us consider in more detail the main groups of drugs used for the rejection of the fertilized egg in the first trimester:
- Antispasmodic drugs
- Papaverine
Myotropic antispasmodic agent. Reduces tone and contractility of smooth muscles. Has vasodilatory and antispasmodic properties.
- Indications for use: spasms of smooth muscles of abdominal organs, spasms of the urinary tract and cerebral vessels, spasms of peripheral vessels.
- Method of administration: subcutaneously, intramuscularly and intravenously. The dosage and duration of therapy is determined by the attending physician.
- Contraindications: intolerance to the components of the drug, arterial hypotension, coma, respiratory depression, glaucoma, renal failure, broncho-obstructive syndrome.
- Side effects: headaches and dizziness, drowsiness, temporary decrease in visual acuity, nausea, bowel disorder, dry mouth, increased activity of liver enzymes. Arrhythmia, increased heart rate, skin allergic reactions, apnea. Overdose has similar symptoms. There is no specific antidote, treatment is symptomatic.
Release form: 2 ml ampoules, 10 pieces per package.
- No-shpa
A medicinal product with the active component drotaverine. It has a strong and long-lasting antispasmodic effect on the body. It dilates blood vessels and normalizes intestinal peristalsis. It does not penetrate the blood-brain barrier and does not have a negative effect on the central nervous system.
- Indications for use: smooth muscle spasms of various etiologies and localizations, headaches and tension, algomenorrhea, colitis, gastritis.
- Method of administration: 120-240 mg per day, divided into 2-3 doses. Duration of therapy depends on the severity of the disease.
- Side effects: headaches, dizziness, CNS disorders, difficulty in defecation, nausea and vomiting, tachycardia, hypotension, allergic reactions.
- Contraindications: hypersensitivity to the components of the drug, renal/hepatic insufficiency, lactose intolerance, lactation, heart failure,
- Overdose: disturbance of rhythm and conduction of the heart muscle. Treatment is aimed at maintaining normal functioning of the body.
Release form: 10 tablets per blister, 2 blisters per package.
- Metacin
M-anticholinergic agent used in diseases with smooth muscle spasms. Prescribed for ulcers of the gastrointestinal tract, gastritis, renal and hepatic colic. In anesthesiology to reduce the secretion of the salivary and bronchial glands.
Method of administration: orally 20-40 mg 2-3 times a day, parenterally 0.5-2 ml of 0.1% solution. Side effects and overdose symptoms include difficulty urinating, dry mouth, constipation. Metacin is contraindicated in cases of increased intraocular pressure and prostatic hypertrophy. The drug is available in two forms: 20 mg tablets, 10 pieces per package, 1 ml ampoules of 0.1% solution, 10 pieces per pack.
- Baralgin
It has pronounced antispasmodic and analgesic properties. It is used for smooth muscle spasms: ureteral spasms, spastic dysmenorrhea, stomach and intestinal spasms, bladder tenesmus and other pathologies.
- The drug is taken orally 1-2 tablets 2-3 times a day. In particularly severe cases, Baralgin is administered intramuscularly or intravenously.
- Contraindications: intolerance to the components of the drug, granulocytopenia, tachyarrhythmia, glaucoma, prostatic hypertrophy, coronary circulatory insufficiency.
- Side effects: allergic reactions. Overdose has similar signs, treatment is symptomatic.
Release form: tablets of 20 pieces and ampoules of 5 ml of 5 pieces per package.
Also, intramuscular injection of a 25% solution of magnesium sulfate will help to relax the uterine muscles.
- Hemostatic
- Etamsylate
Increases the formation of mucopolysaccharides in the capillary walls and increases their stability. Normalizes their permeability, improves microcirculation and has a hemostatic effect.
Stimulates the formation of factor III of blood coagulation, normalizes the rate of platelet adhesion. Does not affect prothrombin time, does not cause increased blood clotting and does not promote the formation of blood clots.
- Indications for use: capillary bleeding in diabetic angiopathies. Surgical interventions in otolaryngology and ophthalmology, dentistry, urology in surgical and gynecological practice. Emergencies in intestinal and pulmonary bleeding and hemorrhagic diathesis.
- Method of administration: intravenously, intramuscularly, orally, subconjunctivally, retrobulbarly. The dosage and duration of therapy are determined by the attending physician.
- Contraindications: bleeding caused by anticoagulants. It is prescribed with caution to patients with a history of thrombosis and embolism. Cases of overdose and adverse reactions have not been identified.
Release form: 12.5% solution in 2 ml ampoules of 10, 50 ampoules per package. 250 mg tablets of 50 and 100 pieces per package.
- Trenaxa
Antifibrinolytic drug, contains the active substance - tranexamic acid. Slows down the process of fibrinolysis, has a local and systemic hemostatic effect. Penetrates well into the synovial fluid, creating concentrations equal to plasma. In the cerebrospinal fluid, the level of active components is about 10%. Tranexamic acid does not bind to plasma albumins. It is excreted by the kidneys unchanged and in the form of metabolites.
- Indications for use: short-term therapy of hemorrhage for patients with increased general fibrinolysis, including malignant lesions of the pancreas and prostate gland, surgical interventions, postpartum hemorrhage. Nasal, uterine and gastrointestinal bleeding, hematuria, bleeding after conization of the cervix, prostatectomy. Hereditary angioedema and skin allergic diseases.
- Method of administration: orally 1-1.5 g 2-3 times a day. The duration of treatment depends on the severity of the disease.
- Side effects: pain in the epigastric region, nausea, vomiting, bowel disorders, headaches and dizziness, urticaria, itching, thrombosis, thromboembolism.
- Contraindications: individual intolerance to the components of the drug, severe renal dysfunction, thrombophlebitis, macroscopic hematuria, myocardial infarction, subarachnoid hemorrhage, high risk of thrombus formation.
- Overdose: pain in the epigastric region, nausea and vomiting, orthostatic hypotension. There is no specific antidote, treatment is symptomatic.
Release form: 6 tablets per strip, 2 strips per package.
- Ascorutin
Reduces capillary permeability, blocks the enzyme hyaluronidase. Prevents lipid peroxidation of cell membranes. Used for increased vascular permeability, hypovitaminosis and avitaminosis P.
The drug is taken 1 tablet 2-3 times a day. Not used in case of intolerance to the active components. No cases of overdose and side effects have been identified. Ascorutin is available in the form of tablets of 10 and 50 pieces per package.
- Dicynone
Antihemorrhagic agent. Suppresses the breakdown of mucopolysaccharides of the vascular wall, normalizes its permeability in pathological processes. The drug acts hemostatically, increases the rate of formation of the primary thrombus. Does not affect prothrombin time and does not have a hypercoagulation effect.
It becomes active in 5-10 minutes after injection and in 1-2 hours after oral administration. It remains effective for 4-8 hours. During the course of treatment, the therapeutic effect lasts for 5-8 days.
- Indications for use: parenchymatous and capillary bleeding during surgical interventions in otolaryngology, ophthalmology, dentistry, gynecology. Emergency surgery to stop acute bleeding, blood system diseases, hemorrhagic diathesis.
- Method of administration: intravenous/intramuscular, oral. The dosage and duration of treatment are determined by the attending physician.
- Side effects: headaches and dizziness, numbness of the lower extremities. Nausea, vomiting, heartburn, heaviness in the epigastric region. Decreased blood pressure, hyperemia of the skin.
- Contraindications: hemorrhages and bleeding due to overdose of anticoagulants, porphyria, thromboembolism, thrombosis. Cases of acute overdose have not been recorded.
Release form: tablets of 50 and 500 mg, 5% and 12.5% injection solution.
- Sedatives
- Persen
A medicinal product with a soft sedative effect on a plant basis. Contains extract of valerian and lemon balm. Calms, relieves irritability and psycho-emotional stress, agitation. Improves falling asleep, but does not cause drowsiness during the day.
- Indications for use: neuroses, psycho-emotional agitation, decreased attention, insomnia, anxiety, vegetative-vascular dystonia. Psychosomatic disorders in stress factors. Withdrawal of strong sedatives.
- Directions for use: orally 2-3 capsules 1-3 times a day. The duration of treatment is determined by the attending physician.
- Side effects: hypersensitivity reactions, tendency to constipation.
- Contraindications: intolerance to the components of the drug, pediatric practice.
- Overdose: weakness, headaches and dizziness, nausea, spastic pain in internal organs, tremor of the extremities, mydriasis. Painful symptoms disappear on their own within 24 hours after administration.
Release form: enteric-coated tablets in blisters of 40 pieces, capsules of 20 pieces per package.
- Novo-Passit
A combination product that includes guaifenesin and a complex of medicinal plant extracts: hawthorn, hops, St. John's wort, lemon balm, passionflower, black elderberry, valerian. It has calming and anti-anxiety properties. Eliminates mental stress and fear. Promotes relaxation of smooth muscles.
- Indications for use: irritability, mild forms of neurasthenia, anxiety, fear, fatigue, memory impairment, mental exhaustion. Sleep disorders, headaches, migraine, neuromuscular excitability. Dermatoses, functional gastrointestinal diseases, vegetative-vascular dystonia.
- Method of administration: syrup and tablets are taken orally. The dosage and duration of therapy is determined by the doctor, individually for each patient.
- Side effects: headaches and dizziness, fatigue, decreased concentration, nausea, vomiting, heartburn, muscle weakness, itching, constipation.
- Contraindications: muscle weakness, hypersensitivity to the components of the drug, severe gastrointestinal disorders, pediatric practice.
Release form: solution for oral administration in 100 ml bottles, 10 tablets in a blister.
As a sedative, you can use an infusion of valerian root or motherwort herb, 1 tablespoon three times a day. Teas and decoctions based on mint, lemon balm, and chamomile will be useful.
- Adrenergic agonists that have an inhibitory effect on the contractile activity of the myometrium.
- Partusisten
A tocolytic agent from the pharmacological group of beta2-adrenergic stimulants. Its mechanism of action is similar to Fenoterol.
- Indications for use: threat of premature birth. Does not have a negative effect on the fetus and baby.
- Method of administration: intravenously by drip 0.5 mg in 250-500 ml of 5% glucose solution. Orally 5 mg every 2-3 hours, maximum daily dosage 40 mg. Duration of treatment is 1-3 weeks.
- Side effects: tachycardia, tremors of the extremities, decreased blood pressure, sweating, nausea and vomiting, muscle weakness.
- Contraindications: cardiac arrhythmia, heart defects, thyrotoxicosis, glaucoma.
Release form: tablets of 0.5 mg and ampoules of 0.025 mg.
- Fenoterol
Adrenomimetic agent, stimulates beta-adrenoreceptors of the uterus and bronchi. It is used to relieve attacks of bronchial asthma, pulmonary emphysema, spastic asthmatic bronchitis. The method of administration and dosage are individual for each patient, therefore they are selected by the attending physician.
Side effects include tremors of the extremities, tachycardia, increased anxiety, fatigue, sweating, headaches. Dosage reduction is indicated for treatment.
The medication is contraindicated in cardiac arrhythmia, severe atherosclerosis. Fenoterol is available in the form of 5 mg tablets, 0.5 mg injection ampoules, and also in the form of a 15 ml aerosol can (300 single doses).
- Ritodrine
A medication that is similar in its mechanism of action to fenoterol, salbupartur and other beta2-adrenomimetics. Relaxes the uterine muscles. It is used as a tocolytic agent in case of a threat of premature termination of pregnancy.
- Method of administration: orally 5-10 mg 3-6 times a day. Duration of treatment is 1-4 weeks. If there is a suspicion of detachment of the ovum in the early stages, the drug is administered intravenously. 50 mg of the drug is diluted in 500 ml of isotonic sodium chloride solution and administered dropwise (10-15 drops per minute).
- Side effects: increased heart rate, tremors of the extremities, muscle weakness, increased sweating, nausea and vomiting, decreased blood pressure. Painful symptoms are reduced by intravenous administration of 30 mg of Verapamil.
- Contraindications: heart rhythm disturbances, thyroid disease, heart defects, increased intraocular pressure.
Release form: ampoules of 10 mg and tablets of 5 mg.
- Hormonal agents
- Utrozhestan
A medicinal product with the active substance – natural micronized progesterone. When introduced into the body, it normalizes secretory transformations in the uterine mucosa. It promotes the transition of the endometrium from the proliferative phase to the secretory phase. During pregnancy, it reduces the contractility and excitability of the myometrium and fallopian tubes. It stimulates transformation in the terminal elements of the mammary glands. [ 16 ]
- Indications for use: the drug is used orally for infertility due to corpus luteum insufficiency, menstrual cycle disorders, mastopathy, and premenstrual syndrome.
- Intravaginal administration of capsules is indicated for maintaining the luteal phase of menstruation, as hormone replacement therapy for premature menopause. It is prescribed for infertility due to corpus luteum insufficiency, for the prevention of uterine fibroids and endometriosis. The drug is effective in threatened abortion and for the treatment of habitual pregnancy loss due to progesterone deficiency.
- Method of administration: tablets are taken orally at 200-300 mg per day, divided into two doses. Capsules are inserted deep into the vagina with a dosage selected by the attending physician. In case of threatened abortion and in preventive treatment of habitual miscarriage, 400-800 mg are used intravaginally.
- Side effects: intermenstrual bleeding, headaches and dizziness, drowsiness, hypersensitivity reactions. Overdose has similar signs, treatment is symptomatic.
- Contraindications: bleeding from the genital tract, tendency to thrombosis, incomplete abortion, malignant lesions of the reproductive organs and mammary glands, porphyria. Not used in case of severe liver dysfunction, allergic reactions to the components of the drug. [ 17 ]
Release form: tablets 100 mg, 30 pieces in a blister, capsules for intravaginal administration 200 mg, 14 pieces in a package.
- Duphaston
A medicinal product with the active substance – dydrogesterone (analogue of natural progesterone). Does not have estrogenic, corticoid or androgenic effects. Does not disrupt thermogenesis and does not affect metabolic processes. Selectively affects progestin receptors of the uterine mucosa. Does not affect follicle ovulation.
- Indications for use: endogenous progesterone deficiency, threatened abortion, habitual loss of the fetus, premenstrual syndrome. Hormone replacement therapy, menopausal syndrome.
- Method of administration: in case of threatened abortion, take 40 mg once a day, then 10 mg every 8 hours for 1 week. The dosage is then reduced, but if there is a new threat of abortion, the doses are restored. The drug can be taken until the 12th-20th week of gestation. In case of dysfunctional bleeding, take 10 mg twice a day in combination with ethinyl estradiol 0.05 mg. When planning a pregnancy or habitual miscarriage - 10 mg twice a day from the 11th to the 25th day of the menstrual cycle.
- Side effects: bleeding may develop in rare cases. Hypersensitivity to the drug may develop.
- Contraindications: intolerance to dydrogesterone or other components of the drug, Rotor syndrome and Dubin-Johnson syndrome. No cases of overdose have been recorded.
Release form: tablets for oral use.
According to statistics, with timely treatment, about 80% of cases of rejection of the fetal formation end with the patient's recovery without complications. If medical care is sought late, maintaining the pregnancy is impossible. In case of incomplete emptying of the uterine cavity, surgical curettage of the products of conception is performed. The duration of treatment is individual for each patient, but on average it is at least 10-14 days. [ 18 ]
Vitamins
Vitamin therapy is an essential component of treatment for any disease or pathological condition. Vitamins are recommended in early pregnancy and during ovum detachment. Most often, women are prescribed the following beneficial substances:
- Vitamin E
Tocopherol improves reproductive functions, so it is prescribed for successful conception. It has antioxidant properties, normalizes the nervous system, protects against stress. It promotes normal fetal development in the first trimester and is responsible for the baby's central nervous system, protects against negative environmental factors. [ 19 ]
Vitamin E should be taken after consultation with your doctor. This is due to the risk of developing allergic reactions and gastrointestinal disorders. Tocopherol is available in liquid form and in capsules that are taken orally. In the early stages, the vitamin is taken at 200 mg per day, divided into two doses. The duration of treatment should not exceed 1 month. [ 20 ], [ 21 ]
- Folic acid
Vitamin B9 belongs to the group of antianemic water-soluble substances. Stimulates hematopoiesis, participates in the formation of erythrocytes, leukocytes and platelets. Promotes the absorption of iron. Folic acid participates in the synthesis of amino acids DNA and RNA, maintaining normal levels of homocysteine and in the maturation of the egg. [ 22 ]
B9 stimulates brain function, improves memory and mood. Normalizes female hormonal levels. Taking the vitamin before conception and in the first trimester reduces the risk of developing pathologies in the fetus. [ 23 ]
Folic acid deficiency can provoke placental abruption and spontaneous abortion. Increases the likelihood of congenital defects and anomalies in the fetus, such as neural tube defects, cleft palate, etc. Folic acid is taken at 0.4 mg per day. An overdose of the drug causes increased excitability, gastrointestinal disorders, and functional changes in the kidneys. [ 24 ]
- Magne B6
Magnesium is involved in many biochemical processes in the body. The substance normalizes the functioning of the immune, nervous and muscular systems, accelerates metabolic processes, and also promotes the restoration of bone tissue. During pregnancy, the body's need for this microelement increases by 2-3 times. [ 25 ]
Magnesium B6 deficiency has a negative impact on women's health and fetal development. This can lead to malformations of the joints and mitral valve of the heart. The risk of miscarriage and premature birth increases. The dosage of the vitamin and the duration of its use are determined by the attending physician, individually for each patient.
Physiotherapy treatment
If there is a risk of detachment of the ovum in the early stages of pregnancy, the woman may be prescribed physiotherapy. Such treatment is aimed at eliminating the threat of termination of pregnancy and reducing the drug load on the body.
Most often, patients are prescribed physiotherapy procedures that affect the contractility of the uterus, central or peripheral mechanisms.
Physiotherapy treatment is indicated in the following cases:
- Risk of spontaneous abortion.
- Early toxicosis with nausea and vomiting.
- Gestosis.
- Fetal growth retardation.
- Post-term pregnancy.
- Divergence of the pubic bones.
- Lactostasis, postpartum endometritis.
In case of a threat of rejection of the fetal formation, the following physiotherapy procedures are used:
- Endonasal galvanization.
- Electrophoresis of magnesium with sinusoidal modulated current.
- Inductothermy of the kidney area.
- Electrorelaxation of the uterus using alternating sinusoidal current.
If the cause of the detachment is isthmic-cervical insufficiency, then drug therapy and physiotherapy are auxiliary methods. The main method of treatment is surgical correction.
Folk remedies
Alternative treatments for ovum detachment are in most cases ineffective and even dangerous. But some women still resort to folk therapy. Let's look at the safest methods based on medicinal plants:
- Pour 500 ml of boiling water over a tablespoon of viburnum bark and simmer for 10 minutes. Cool and strain. Take ½ cup 3 times a day.
- Grind and combine 100 g of dry yarrow herb and 50 g of knotweed herb. Take the herbal powder ½ teaspoon 3 times a day 30 minutes before meals.
- Take 5 g of fresh dandelion leaves or roots. Pour boiling water over them and boil for 5-7 minutes over medium heat. Take 50 ml 3 times a day.
- Mix fresh St. John's wort and calendula flowers in equal proportions. Pour 250 ml of boiling water and let it brew for 30-40 minutes. Strain and take 2 glasses a day, adding a spoonful of honey.
All the above recipes are used when there is a threat of miscarriage in the first trimester. Before using traditional medicine methods, you should consult with your doctor and get his permission.
Herbal treatment
Medicinal herbs are another alternative approach to treating early pregnancy abruption.
To prevent miscarriage, the following herbal recipes can be used:
- Take 2 parts of erysipelas, marigold flowers and angelica herb. Combine them with 1 part of stinging nettle leaves and cinquefoil rhizomes. Pour 500 ml of boiling water over two tablespoons of the mixture and let it brew for 3 hours. Strain and take ½ cup 3 times a day 30 minutes before meals.
- Pour 1 liter of water over three tablespoons of calendula (leaves and inflorescences) and place on medium heat. The liquid should boil down to half. Strain the cooled decoction and take 50 ml 2-3 times a day before meals.
- Take 3 parts of licorice and elecampane roots, add 2 parts of blackcurrants. Mix the herbs thoroughly and combine with 1 part of cinquefoil and stinging nettle roots. Pour 250-300 ml of boiling water over 2-3 spoons of the mixture, boil over medium heat for 20-30 minutes. Cool, strain and take ½ cup 3 times a day before meals.
Before using the above recipes, you should consult with your doctor and make sure that there are no allergic reactions to the herbal ingredients of the recipes.
Homeopathy
An alternative method of treating spontaneous abortion in the first months of pregnancy is homeopathy. If there is a threat of miscarriage, the following homeopathic preparations can be used:
- Aconite – threat of abortion after nervous experience, stress, fit of anger.
- Arnica – rejection of the fertilized egg after injury, severe bleeding.
- Belladonna – nagging pain in the lower abdomen and back, profuse bloody discharge.
- Caulophyllum – habitual miscarriage, painful sensations in the back and abdomen. Contractions of the uterus with slight bloody discharge.
- Chamomilla - abortion after strong nervous excitement.
- Cimicifuga – sharp pain in the lower abdomen.
- Sabina – profuse bloody discharge. Back pain, spreading to the lower abdomen.
- Secale – risk of detachment, heavy bleeding, severe pain.
- Sepia – sharp pains and weakness, muscle spasms.
- Viburnum – history of miscarriages, pain in the abdomen, back and hips.
All medications and their dosage are selected by a homeopathic doctor, assessing the patient's condition.
Surgical treatment
In case of incomplete miscarriage, septic abortion and massive bleeding, surgical treatment is indicated. Before the operation, an ultrasound examination is performed, which reveals the remains of the fertilized egg in the uterine cavity. Depending on the ultrasound results, the following types of curettage may be prescribed:
- Aspiration curettage – the remains of the embryo are small and can be sucked out with a vacuum. [ 26 ]
- Curettage - the fetus has died, but has not completely exited the uterus.
The treatment is performed under general or local anesthesia. Special instruments are used for the operation, opening the cervix and removing the upper layer of the endometrium. The procedure takes about 15-25 minutes. After that, the patient spends a couple of hours under medical supervision and, if there are no complications, goes home.
After curettage, the following complications may develop, some of which are normal:
- Moderate pain in the lower abdomen, similar to menstrual pain. It lasts from a couple of hours to several days and does not require treatment.
- Heavy bloody discharge. Normally lasts no more than 10 days. If bleeding persists longer, it may be a sign of cervical spasm and requires additional treatment.
- Risk of infection and development of sepsis.
- Risk of incomplete extraction of fetal tissue remnants. Causes severe blood loss and requires urgent surgical intervention.
- Risk of damage to the cervix or body of the uterus during surgery. Incorrect actions by the surgeon can lead to perforation of the uterus or rupture of its tissues.
The tissues obtained as a result of the operation after a miscarriage are sent for histological examination. This is necessary to confirm the intrauterine pregnancy, exclude ectopic pregnancy, trophoblastic disease.
In order to minimize the risk of miscarriages in the future, you should undergo a comprehensive medical examination. This will help determine the causes of the rejection of the fetal formation and eliminate them.
Prevention
There are no specific methods for preventing abruption of the ovum in the first months of pregnancy. To reduce the risk of developing neural tube defects in the fetus, which can cause miscarriages, taking folic acid is recommended during pregnancy planning and during the first trimester.
Planning of conception is of no small importance. In preparation for pregnancy and to reduce the risk of spontaneous abortion, future parents should undergo a medical examination and take a number of tests:
- Analysis for STDs and infectious diseases.
- Genetic tests.
- Examination of the reproductive system.
- Ultrasound of the pelvic organs in women.
- Determination of biocompatibility of spouses and other tests.
Regular visits to the gynecologist and timely registration at the antenatal clinic are also a preventive method. Medical consultation and early screenings allow you to assess the state of the ongoing pregnancy.
The expectant mother is recommended to have a balanced diet, moderate physical activity and a minimum of stress. She should also give up bad habits that have a negative impact on both the female body and the development of the fetus.
Forecast
Detachment of the ovum in early pregnancy has a favorable outcome. With one spontaneous abortion, the risk of disruption of the next pregnancy is about 20%. If a woman has two spontaneous miscarriages in a row, a comprehensive examination is carried out to identify the causes of this anomaly.
Do not forget about psychological rehabilitation. After a miscarriage, a woman faces severe stress and depression, so she needs rehabilitation therapy. You can plan a new pregnancy no earlier than in 6-12 months. It is very important to exclude all factors that led to an abortion in the past.

