Ureaplasma during pregnancy
Last reviewed: 23.04.2024

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Often, women are faced with such a concept as ureaplasma during pregnancy.
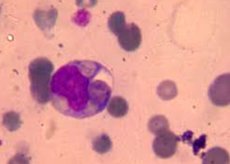
What is ureaplasma (Ureaplasma urealyticum)? This is a medium-sized species of gram-negative bacteria that do not have a cell wall and their own carrier of genetic information. Therefore ureaplasma lives only in symbiosis with other types of microorganisms. It has the property of generating ATP exclusively by the method of hydrolysis of urea, therefore mass contamination with ureaplasma occurs mainly in the urogenital tract, less often in the respiratory tract, as well as in the upper and lower parts of the digestive tract.
Causes of ureaplasmosis during pregnancy
Dysbiosis of the genital tract is a violation of the quantitative and qualitative balance of the total microflora present. Some initially neutral microorganisms (in particular, the gardnerella) prepare the flora of the vagina for possible pathogenization of the process of coexistence of bacteria. As a consequence, under certain circumstances, the symbiosis of gardnerella and ureaplasma in pregnancy can lead to the multiplication of microbial colonies and the development of inflammation.
Ureaplasma urealyticum have an intermediate structure, something between the virus and the common bacterium. Due to the inherent function of ureoleisis, infection occurs primarily in the genitourinary sphere. Therefore, the most common method of infection is considered to be the sexual way. Men are also possible carriers of infection, although they do not occur as often as women. Other contact methods of transmission of infection, such as using a public toilet, visiting the pool or a common bath, are much less likely, and many experts exclude them altogether.
Therefore, it is commonly believed that infection with the infection occurs during unprotected sex.
With the beginning of pregnancy, when there is a significant hormonal changes in the body, a natural decrease in immunity promotes a surge in the activity of microorganisms and their transition to a pathogenic state. Previously, peacefully coexisting bacteria begin to multiply rapidly, this leads to a violation of the microbiocenosis of the genitourinary sphere. This creates optimal conditions for the development of the inflammatory process.
Many women, especially at the planning stage of conception, are interested in the question: is it possible at all to make pregnancy with ureaplasmosis? The answer to this question is unambiguous: in itself, the presence in the body of Ureaplasma urealyticum does not have any effect on a woman's ability to become pregnant.
However, the inflammatory process (ureaplasmosis) that has arisen because of this pathogen can lead to a number of complications, which in the future can interfere with the reproductive function. Adhesive disease, obstruction of the fallopian tubes, inflammatory diseases of the uterus and appendages - these are some of the consequences of infection.
Symptoms of ureaplasma in pregnancy
Usually, from the moment the ureaplasmosis pathogen enters the body before the appearance of the first visible symptoms of the disease, it takes about 30 days. This time is called a latent, or latent, period. During this period, the presence of Ureaplasma urealyticum in the body does not appear, and after the completion of the incubation process, the disease can develop in two scenarios:
- the course of the disease may be subtle, with a mild symptomatology that the patient can easily ignore;
- the onset of the disease can be acute, with marked characteristic symptoms of ureaplasmosis requiring immediate treatment.
Both variants of ureaplasmosis can be represented by the following manifestations:
- the appearance of mucous secretions of incomprehensible etiology;
- a feeling of discomfort in the vagina, reminiscent of the symptoms of thrush;
- burning in the urethra, frequent urination, pain and pain when urinating, turbidity of urine;
- lower abdominal pain;
- signs of inflammation of the mucous membranes of the respiratory tract, edema of the nasopharynx, larynx, symptoms of acute respiratory infection, purulent sore throat.
Perhaps the appearance of sexual discomfort - pain and discomfort during sexual intercourse.
In the absence of the necessary treatment for infection, the process of inflammation expands, there are more serious complications, such as inflammation of the bladder, uterus and appendages. Symptoms of ureaplasmosis in pregnancy may be signs of pyelonephritis.
Is it dangerous in pregnancy ureaplasma?
Many future mothers are wondering: Is pregnancy ureaplasma dangerous?
It should be noted that the bacteria themselves Ureaplasma urealyticum can live on mucous completely healthy people and not bring them any discomfort. Usually, women do not even guess about the presence of pathogenic flora in their organism, while it does not concern the delivery of tests and bacteriological cultures.
Ureaplasmas begin to pose a danger in pregnancy only when their number becomes higher than normal, or when the immune forces of the body fall, as a result of various inflammations, stressful situations, hypothermia, hormonal imbalance.
There are always laboratory tests, in particular, on the presence of ureaplasma, when planning pregnancy. It is always better to know about possible risk factors in advance, in time to prevent consequences. It is more expedient to destroy the pathogen before the onset of pregnancy, without endangering the future child, and even the pregnancy itself as a whole.
How does ureaplasma affect pregnancy? If ureaplasmosis is found already in a pregnant woman, it can affect the mental and physical usefulness of the fetus, lead to serious intra-uterine developmental defects. Even the loss of pregnancy itself is possible - Ureaplasma urealyticum in the early stages, when the placenta is not yet formed, represents a real threat of miscarriage or a stagnant pregnancy.
In other periods of gestation, in connection with the pathological impact of ureaplasma on the future child's emerging organism, there is a risk of spontaneous termination of pregnancy or premature birth.
Even a normally well-bred, healthy child has a huge risk of contracting Ureaplasma urealyticum from the mother while passing the birth canal. Bacteria get on the mucous membranes of the newborn, provoking in the future diseases of the nasopharynx, respiratory tract, inflammation of the genital organs, meningitis.
Therefore, in planning recommended mandatory examination of the future mother, in order to avoid the consequences of ureaplasmosis in pregnancy.
Diagnosis of ureaplasma in pregnancy
The primary diagnosis of ureaplasma during pregnancy is based on data from subjective and objective research. Complaints of patients corresponding to the clinical symptoms of the disease are taken into account. Also important are the objective signs of ureaplasmosis: the presence and nature of secretions, their accumulation in the posterior vaginal fornix, hyperemia or pallor of the mucous membranes.
It should be noted that the norm of the content of Ureaplasma urealyticum in pregnancy is less than 10 to 4 degrees of microbial elements in 1 g or 1 ml of excreta. Higher concentrations mean the possibility of developing the disease.
The fence of the test material for diagnosis of ureaplasma during pregnancy can be made in several ways:
- scraping from the surface of the vagina, cervix, and immersing it in a specific diagnostic environment;
- flushing with an isotonic solution of sodium chloride from the surface of the vagina or urethra;
- A smear on Ureaplasma urealyticum with the subsequent bacterial culture.
Analyzes for a ureaplasma will help to reveal one of two kinds of activators of the given infection:
Ureaplasma parvum is the most pathogenic form of ureaplasma. It is a more active bacterium, easily cleaves urea with ammonia release. As a consequence - a protracted inflammatory process and increased formation of salts of uric acid in the ureters and kidneys. Ureaplasma Parvum does not have its own cell membrane, therefore it forms a dense symbiosis with epithelial cells, eventually destroying them. The enzymatic activity of this pathogen makes it possible to exert a destructive effect on the proteins of the epithelium, destroying the antibodies of the mucous membrane and thereby drastically lowering the local immunity. This type of infection is more aggressive and rarely involves peaceful carriage, often reborn into a bright inflammatory process.
Ureaplasma urealitikum - less aggressive bacterium, prone to permanent habitation on the mucosa of a healthy person. The possibility of developing an inflammatory process caused by this type of infection appears only when the general immunity of the body falls. But at the same time, the most harmless ureaplasma ureaplasma in pregnancy is more dangerous: it is the only kind of ureaplasma that penetrates the placental barrier and represents a real threat to the future child.
Sometimes both varieties of ureaplasma exist together in one territory. In such cases, the laboratory uses the term Ureaplasma species.
Among the additional types of diagnostics, the use of venous blood for the presence of antibodies to ureaplasma, as well as immunofluorescence analysis to determine the pathogen antigens.
Who to contact?
Treatment of ureaplasma in pregnancy
Treatment of ureaplasma during pregnancy is mainly performed on an outpatient basis. The causative agent of this disease has the property of rapidly adapting to various types of antibiotics. Therefore, they are usually prescribed, gradually moving from lighter drugs to potent ones. To determine the necessary spectrum of action of drugs, an analysis is made for the sensitivity of pathogenic flora to antibiotics.
In pregnancy, not all antimicrobials can be used, so only the safest for the future mother and fetus are selected for treatment.
To completely get rid of infection, simultaneous treatment of both spouses is especially important. In addition, during the period of therapy, it is better to refuse sexual intercourse in general, or use a condom, otherwise the mutual process of infection will stretch the period of treatment to infinity.
Of the antimicrobial agents, macrolide antibiotics (erythromycin, oleandomycin phosphate), lincosamides (lincomycin, clindamycin) are most often used. Especially effective treatment of ureaplasma with rovamycin, it is taken by 3 million IU 2-3 times a day.
As ancillary drugs used drugs for the treatment of protozoal infections, antifungal agents (nystatin, levorin).
The course of antibiotic therapy lasts 10-14 days.
Additionally, preparations can be prescribed to support immunity (biologically active peptides, interferons), complex groups of vitamins. Local installations of medicines, physiotherapy are conducted.
Quite often when an infection is used vaginal suppository - geneferon, terzhinan, neo-pentotrans.
Diet during the treatment of Ureaplasma urealyticum implies a complete refusal of spicy, smoked, salty foods, alcoholic beverages and sweets. We welcome the use of sour-milk products, vegetables and fruits.
In the future it is recommended to strictly adhere to the rules of personal hygiene, to avoid casual sexual relations.
With any suspicious symptoms it is better to consult a specialist, and then the pregnancy will be easy, and the future baby will be healthy. It is also necessary to understand that ureaplasma during pregnancy is not a sentence, it can be disposed of, following the prescriptions and advice of a doctor.
More information of the treatment


 [
[