Medical expert of the article
New publications
Ureaplasma in pregnancy
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Often women encounter such a concept as ureaplasma during pregnancy.
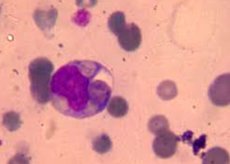
What is ureaplasma (Ureaplasma urealyticum)? It is a small type of gram-negative bacteria that does not have a cell wall and its own carrier of genetic information. Therefore, ureaplasma lives only in symbiosis with other types of microorganisms. It has the ability to generate ATP exclusively by hydrolysis of urea, therefore, mass seeding with ureaplasma occurs mainly in the urogenital tract, less often in the respiratory tract, as well as the upper and lower parts of the digestive tract.
Causes of ureaplasmosis during pregnancy
Dysbiosis of the genital tract is a concept of a violation of the quantitative and qualitative balance of the general microflora present. Some initially neutral microorganisms (in particular, gardnerella) prepare the vaginal flora for possible pathogenization of the process of coexistence of bacteria. As a result, under certain circumstances, the symbiosis of gardnerella and ureaplasma during pregnancy can lead to the proliferation of microbial colonies and the development of inflammation.
Ureaplasma urealyticum have an intermediate structure, something between a virus and a common bacterium. Due to their inherent ureolysis function, the infection occurs primarily in the urogenital area. Therefore, the most common way of infection is considered to be sexual intercourse. Men are also possible carriers of the infection, although it is not as common in them as in women. Other contact methods of infection transmission, such as using a public toilet, visiting a swimming pool or a public bath, are much less likely, and many specialists exclude them altogether.
Therefore, it is generally accepted that infection occurs during unprotected sexual intercourse.
With the onset of pregnancy, when significant hormonal changes in the body are observed, a natural decrease in immunity contributes to a surge in the activity of microorganisms and their transition to a pathogenic state. Previously peacefully coexisting bacteria begin to multiply rapidly, which leads to a disruption of the microbiocenosis of the genitourinary sphere. This creates optimal conditions for the development of the inflammatory process.
Many women, especially at the stage of planning conception, are interested in the question: is it possible to become pregnant with ureaplasmosis? The answer to this question is unambiguous: the presence of Ureaplasma urealyticum in the body itself does not affect a woman's ability to become pregnant.
However, the inflammatory process (ureaplasmosis) caused by this pathogen can lead to a number of complications that can further interfere with reproductive function. Adhesive disease, obstruction of the fallopian tubes, inflammatory diseases of the uterus and appendages are some of the consequences of the infection.
Symptoms of Ureaplasma during Pregnancy
Usually, about 30 days pass from the moment the ureaplasma pathogen enters the body until the first visible symptoms of the disease appear. This time is called the latent, or hidden, period. During this period, the presence of Ureaplasma urealyticum in the body does not manifest itself in any way, and after the incubation process is complete, the disease can develop according to two scenarios:
- the course of the disease may be subtle, with mild symptoms that the patient can easily ignore;
- The onset of the disease can be acute, with pronounced characteristic symptoms of ureaplasmosis, requiring immediate treatment.
Both variants of the course of ureaplasmosis can be represented by the following manifestations:
- the appearance of mucous discharge of unknown etiology;
- a feeling of discomfort in the vagina, reminiscent of the symptoms of thrush;
- burning in the urethra, increased urge to urinate, pain and stinging when urinating, cloudy urine;
- pain in the lower abdomen;
- signs of inflammation of the mucous membranes of the respiratory tract, swelling of the nasopharynx, larynx, symptoms of acute respiratory infection, purulent tonsillitis.
Sexual discomfort may occur – pain and unpleasant sensations during sexual intercourse.
In the absence of necessary treatment of the infection, the inflammation process expands, more serious complications appear, such as inflammation of the bladder, uterus and appendages. Symptoms of ureaplasmosis during pregnancy may be accompanied by signs of pyelonephritis.
Is ureaplasma dangerous during pregnancy?
Many expectant mothers ask themselves: is ureaplasma dangerous during pregnancy?
It should be noted that Ureaplasma urealyticum bacteria themselves can live on the mucous membranes of absolutely healthy people and not cause them any discomfort. Usually women do not even suspect the presence of pathogenic flora in their body until it comes to taking tests and conducting bacteriological cultures.
Ureaplasmas begin to pose a danger during pregnancy only when their number becomes higher than normal, or when the body's immune forces decline, as a result of various inflammations, stressful situations, hypothermia, hormonal imbalance.
Laboratory tests are always carried out, in particular, for the presence of ureaplasma, when planning a pregnancy. It is always better to know about possible risk factors in advance in order to have time to prevent the consequences. It is more expedient to destroy the pathogen before pregnancy, without endangering the future child, and the pregnancy itself in general.
How does ureaplasma affect pregnancy? If ureaplasmosis is detected in a pregnant woman, it can affect the mental and physical fitness of the fetus, leading to serious intrauterine developmental defects. Even the loss of pregnancy itself is possible - Ureaplasma urealyticum in the early stages, when the placenta has not yet formed, poses a real threat of miscarriage or frozen pregnancy.
During other periods of gestation, due to the pathological impact of ureaplasma on the developing organism of the future child, there is a risk of spontaneous termination of pregnancy or premature birth.
Even a normally carried healthy child has a huge risk of becoming infected with Ureaplasma urealyticum from the mother when passing through the birth canal. The bacteria get on the mucous membranes of the newborn, causing diseases of the nasopharynx, respiratory tract, inflammation of the genitals, meningitis in the future.
Therefore, when planning, it is recommended that the expectant mother undergo mandatory examination to avoid the consequences of ureaplasmosis during pregnancy.
Diagnosis of ureaplasma during pregnancy
Primary diagnostics of ureaplasma during pregnancy is based on subjective and objective examination data. Patient complaints corresponding to the clinical symptoms of the disease are taken into account. Objective signs of ureaplasmosis are also important: the presence and nature of discharge, its accumulation in the posterior vaginal fornix, hyperemia or pallor of the mucous membranes.
It should be known that the normal content of Ureaplasma urealyticum during pregnancy is less than 10 to the 4th power of microbial elements in 1 g or 1 ml of secretions. Higher concentrations indicate the possibility of developing the disease.
Collection of the test material for diagnosing ureaplasma during pregnancy can be done in several ways:
- scraping from the surface of the vagina, cervix, and immersing it in a specific diagnostic environment;
- washing with an isotonic sodium chloride solution from the surface of the vagina or urethra;
- smear for Ureaplasma urealyticum followed by bacterial culture.
Ureaplasma tests will help identify one of two types of pathogens of this infection:
Ureaplasma parvum is the most pathogenic type of ureaplasma. It is a more active bacterium, easily breaking down urea with the release of ammonia. As a result - a protracted inflammatory process and increased formation of uric acid salts in the ureters and kidneys. Ureaplasma parvum does not have its own cell membrane, therefore it forms a dense symbiosis with epithelial cells, destroying them over time. The enzymatic activity of this pathogen allows it to have a destructive effect on epithelial proteins, destroying the antibodies of the mucous membrane and thereby dramatically reducing local immunity. This type of infection is more aggressive and rarely involves peaceful carriage, more often degenerating into a bright inflammatory process.
Ureaplasma urealyticum is a less aggressive bacterium, prone to permanent residence on the mucous membrane of a healthy person. The possibility of developing an inflammatory process caused by this type of infection appears only when the general immunity of the body falls. But at the same time, the most harmless ureaplasma urealyticum during pregnancy is more dangerous: this is the only type of ureaplasma that penetrates the placental barrier and poses a real threat to the unborn child.
Sometimes both types of ureaplasma coexist in the same area. In such cases, laboratories use the term Ureaplasma species.
Additional diagnostic methods include testing venous blood for the presence of antibodies to ureaplasma, as well as immunofluorescence analysis to determine the pathogen's antigens.
Who to contact?
Treatment of ureaplasma during pregnancy
Treatment of ureaplasma during pregnancy is carried out mainly on an outpatient basis. The pathogen of this disease has the ability to quickly adapt to various types of antibiotics. Therefore, they are usually prescribed, gradually moving from lighter drugs to potent ones. To determine the required spectrum of action of drugs, an analysis of the sensitivity of pathogenic flora to antibiotics is first carried out.
Not all antimicrobial drugs can be used during pregnancy, so only those that are safest for the body of the expectant mother and fetus are selected for treatment.
For complete elimination of the infection, simultaneous treatment of both spouses is especially important. In addition, during the period of therapy, it is better to abstain from sexual intercourse altogether, or use a condom, otherwise the mutual infection process will extend the treatment period indefinitely.
Of the antimicrobial agents, the most commonly used are macrolide antibiotics (erythromycin, oleandomycin phosphate), lincosamides (lincomycin, clindamycin). Especially effective is the treatment of ureaplasma with rovamycin, it is taken at 3 million IU 2-3 times a day.
As auxiliary means, drugs for the treatment of protozoal infections and antifungal agents (nystatin, levorin) are used.
The course of antibiotic therapy lasts 10-14 days.
Additionally, medications to support immunity (biologically active peptides, interferons), complex groups of vitamins may be prescribed. Local instillations of medications and physiotherapy are performed.
Quite often, vaginal suppositories are used for infections - Genferon, Terzhinan, Neo-Penotran.
The diet during treatment of Ureaplasma urealyticum involves complete rejection of spicy, smoked, salty food, alcoholic beverages and sweets. The consumption of fermented milk products, vegetables and fruits is encouraged.
In the future, it is recommended to strictly adhere to the rules of personal hygiene and avoid casual sexual relations.
In case of any suspicious symptoms, it is better to consult a specialist, and then the pregnancy will be easy, and the future child will be healthy. It is also necessary to understand that ureaplasma during pregnancy is not a death sentence, you can get rid of it by following the doctor's instructions and advice.
More information of the treatment


 [
[