Medical expert of the article
New publications
Staphylococcus aureus in infants
Last reviewed: 19.07.2022

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Staphylococci are widely distributed in the environment and can be represented by both opportunistic and pathogenic microorganisms. The most pathogenic is Staphylococcus aureus, which can cause the development of purulent inflammatory processes in various organs and tissues. Staphylococcus aureus is especially dangerous in infants, primarily because of inadequate children's immune defenses. What do you need to know about this bacterium, and what steps should you take if your baby has a positive test result?
Epidemiology
According to statistics, in every third child, Staphylococcus aureus can be found on the skin or mucous membranes. As a rule, we are talking about the carriage of an infection, which, nevertheless, can later enter the body and provoke the development of various pathologies - from furunculosis to pneumonia and even sepsis.[1]
Most often, the bacterium is found in children of the first year of life. Further, with age, the degree of sowing gradually decreases. The causative agent is sown mainly from the mucous membrane of the nasal cavity and tonsils, but other localizations also occur.[2]
Staphylococcus aureus causes more than 60% of existing staphylococcal infectious diseases. Saprophytic and epidermal staphylococcus aureus are found somewhat less frequently.[3]
Causes of the staphylococcus aureus in a newborn
Staphylococcus aureus may well live in the body of any person - but only in small quantities. Active reproduction of bacteria begins against the background of a sharp weakening of the immune defense, or with other stress factors.[4]
Infants are most susceptible to active growth and infection. In young children, the production of the necessary antibodies has not yet been established, and the immune system is weak and inferior.
Staphylococcus aureus in infants may appear:
- when infected from one's own mother - for example, during childbirth or while breastfeeding;
- from medical workers in the maternity hospital, hospital, clinic;
- in direct contact with a sick person (carrier);
- upon contact with objects affected by Staphylococcus aureus (toys, dishes, etc.)
Risk factors
The risk group usually includes:
- children born prematurely;
- babies who have been on artificial nutrition since birth;
- weak babies suffering from lack of weight;
- children with congenital defects and diseases;
- infants who were treated with antibiotics, hormonal drugs, or children with diagnosed intestinal dysbacteriosis;
- babies living in unfavorable sanitary conditions, with insufficient observance of hygiene standards, against the background of malnutrition.
Pathogenesis
Staphylococcus aureus is one of the most pathogenic varieties of such bacteria. This does not exclude the presence of this microbe in a healthy human microflora.
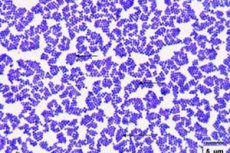
Staphylococcus aureus received such an unusual name because of its ability to form a specific pigment substance, which, under microscopic examination, has a characteristic orange-yellow hue. This bacterium is resistant to medicines, can "survive" boiling, exposure to ultraviolet radiation, prolonged drying. It is not affected by strong saline solutions and hydrogen peroxide, so the bacterium lives and reproduces perfectly in almost any conditions.[5]
Staphylococcus aureus has a pronounced enzymatic activity and secretes:
- lipase, which destroys fats, which allows bacteria to easily overcome the skin barrier and enter the bloodstream;
- coagulase, which contributes to the creation of protection of bacteria from immune cells;
- penicillinase, which makes bacteria resistant to penicillin drugs.
In addition, Staphylococcus aureus excretes endo and exotoxic substances that cause severe intoxication. This microbe exhibits powerful drug resistance, is prone to frequent mutation, so it is quite difficult to get rid of it.
One of the most unfavorable mutations of the microbe is methicillin-resistant staphylococcus aureus: it occurs mainly as a nosocomial infection.
How is Staphylococcus aureus transmitted to babies?
A child can become infected with Staphylococcus aureus anywhere - at home, on the street, from his own mother, as well as from some food or water.
Since the bacterium is very resistant, it is often found in hospitals and clinics: if all existing sanitation standards are observed, the microbe is able to mutate to such an extent that it becomes resistant to almost any processing solutions.[6]
There are several ways to get Staphylococcus aureus to the baby:
- contact household method - consists in the transmission of infection through objects contaminated with bacteria (toys, linen, towels, dishes, etc.);
- drop-air method - involves the transmission of bacteria through the air with coughing, sneezing, etc.;
- fecal-oral method - consists in the spread of germs through unwashed hands, mother's breasts (during breastfeeding);
- vertical method - involves the transfer of infection to the baby from his mother during pregnancy or during childbirth (when passing through the birth canal).
Another possible transmission option is considered to be the use of mother's milk by the baby, if the mother is sick with infectious mastitis.
Symptoms of the staphylococcus aureus in a newborn
Staphylococcus aureus in the active stage usually reveals itself with the following symptoms:
- the baby has a very high temperature;
- there are bright signs of rhinitis;
- the child is lethargic, capricious, refuses to eat, cries;
- possible bouts of nausea and vomiting;
- cough appears;
- eyes swell and redden, lacrimation is possible;
- the chair becomes unstable (periods of constipation and diarrhea alternate);
- the baby loses weight (primarily due to loss of appetite);
- the balance of intestinal microflora is disturbed);
- the skin is covered with a rash and other pathological elements - these can be acne, pustules, itchy nodules, areas of peeling.
The incubation period for the activation of Staphylococcus aureus can range from 3 hours to 4-5 days. In this case, it is possible to accurately determine the pathogen only after sowing.
Norm of Staphylococcus aureus in infants
Staphylococcus aureus can be found on the skin and mucous membranes of the baby, as well as in the intestines, nasal cavity, and tonsils. With any suspicion of an infection, an analysis is performed on the baby, which will accurately indicate whether there is a pathology or not.
Determination of the presence and abundance of Staphylococcus aureus may be necessary in order to assess the need for treatment: if the number of bacteria is within acceptable limits, and there are no clinical symptoms, then no treatment is carried out. For example, Staphylococcus aureus in the intestinal cavity can be found in almost all cases, and this is not a reason for therapy. However, if the number of bacteria is exceeded, then measures must be taken, otherwise unpleasant pathological signs will follow in the form of infectious colitis, colic and other digestive disorders.
The presence of Staphylococcus aureus does not always indicate an infectious lesion, since we can talk about asymptomatic carriage. Sowing a smear from the nasal cavity and pharyngeal mucosa with the determination of the number of microbes up to 10 3 is considered a common non-pathological carriage. Exceeding this indicator can cause the development of infectious and inflammatory diseases. In children older than 1 year, the norm is slightly higher - up to 10 4 .
Only the presence of Staphylococcus aureus cannot be a reason for prescribing drug therapy.
The number of staphylococcus should be determined before the start of treatment and after its completion. In the future, it is required to control the number of bacteria for a couple of months after the therapeutic course.[7]
Staphylococcus aureus in infants in feces
An analysis of feces for a baby can be prescribed already in the hospital if there is a suspicion of Staphylococcus aureus. Fecal masses are examined at least twice - for example, with an interval of one or two days. The material for analysis is provided to the laboratory as early as possible - preferably immediately after a bowel movement, but no later than 3 hours after it. Such timing directly affects the correctness of the results.
The maximum allowable rate of Staphylococcus aureus in feces can be 10 3 10 4.
Even if the indicator of the number of bacteria is within the normal range, the doctor will advise you to observe its dynamics, since further rapid reproduction of the infection is not excluded, which will require an urgent start of treatment. If the number of Staphylococcus aureus changes insignificantly, then we can talk about the normal state of health of the baby.
The manifestation of Staphylococcus aureus on the skin in newborns
Staphylococcus aureus is able to manifest itself in any organ and on any tissue of the human body. And this is the special danger of bacteria.
Skin manifestations in children can be different, depending on the form of staphylococcal lesions:
- Staphylococcal folliculitis is manifested by an inflammatory process in the tops of the hair follicles: the skin around the follicle turns red, an abscess or pustule forms, which, after opening, exposes a crust or sore. Quite extensive areas can be affected - mainly in the face or head.
- Staphylococcal hidradenitis is an inflammation of the sweat glands that can be found almost anywhere on the body. There are pustules (pimples), areas of swelling.
- Furuncles are usually painful and may affect the face, back, and neck. More complex elements are carbuncles: the affected skin areas become cyanotic, specific purulent funnels form, and the temperature may rise.
Even if these pathological signs are detected, the treatment of the baby is not carried out until the results of the tests are obtained: it is imperative to make sure that the violation of the skin is not caused by other adverse factors.
Staphylococcus aureus in a baby's nose
Staphylococcus aureus is often sown precisely from the nasal cavity, but its presence does not always indicate the presence of the disease. Only against the background of exceeding the permissible indicators do the first signs of infection appear:
- whitish or greenish-yellow discharge;
- fever, fever;
- signs of general intoxication;
- violation of the general condition, headaches, nausea, loss of appetite.
In the future, Staphylococcus aureus can become an impetus for the development of pathologies such as sinusitis, frontal sinusitis. The pathological condition is aggravated against the background of frequent and uncontrolled use of nasal vasoconstrictor drugs, self-treatment with antibacterial agents, incomplete or incorrectly conducted course of antibiotic therapy.
Complications and consequences
Staphylococcus aureus in infants can provoke a generalized pathological process, since the microbe can spread freely, affecting many tissues and organs. At the same time, there is a danger even with an initial small manifestation of the disease on the skin: if left untreated, children's phlegmon develops for a short time, which is a purulent-inflammatory reaction in adipose tissue, with the further formation of a necrotic process.[8]
In cases where the infectious carrier is the mother of the child, Staphylococcus aureus can easily enter the cavity of the child's intestines (this occurs during breastfeeding). This mechanism causes serious disturbances in the digestive tract. As a result, the growth and development of the baby is disturbed.
In addition, Staphylococcus aureus from tissues can penetrate into the bloodstream, with the further development of an extensive pathological process: we are talking about septic complications that threaten the life of an infant.[9]
Diagnostics of the staphylococcus aureus in a newborn
Diagnostic measures for the detection of Staphylococcus aureus primarily include the use of serological tests, namely:
- conventional coagulase test with a test tube, the duration of the test is from four to 24 hours;
- latex agglutination reaction using latex particles coupled with anti-staphylococcus antibodies (meaning A-protein, clumping factor and a number of surface antigens).
In addition, the following tests may be useful in diagnosis:
- general clinical studies of blood and urinary fluid (with a staphylococcal infection, an increased content of leukocytes and neutrophils, an accelerated ESR are determined in the blood, and protein, leukocytes and staphylococci are found in the urine);
- biological inoculation on an appropriate nutrient medium.
Culture is necessary to identify the infectious agent and determine its sensitivity to antibiotic therapy. Sowing of fecal masses is possible no later than 3 hours after a bowel movement. A swab from the oral cavity and nasopharynx is taken before meals and the use of any medications.
In case of damage to the skin, it is important to take a smear from the affected areas, after mechanical cleaning and treatment of the wound surface with antiseptic preparations.
Instrumental diagnostics involves the use of such procedures:
- The agglutination reaction is carried out to determine the dynamics of the pathology and evaluate the effectiveness of the chosen therapy. The study is repeated at least twice with an interval of 1-1.5 weeks. If antibody titers in the blood rise and exceed 1:100, then this indicates that the infection is progressing.
- Phage typing of plasmacoagulating Staphylococcus aureus helps to determine the degree of sensitivity of microorganisms to viral phages, for further selection of therapeutic measures.
Differential diagnosis in the laboratory is carried out with streptococcal infection.
Treatment of the staphylococcus aureus in a newborn
If the amount of Staphylococcus aureus in the body of the baby exceeds the permissible values, then the pathology should be treated under the supervision of a doctor, following all his instructions. Additionally, parents can take the following steps:
- bathe the child in herbal decoctions (decoctions and infusions of chamomile, sage, calendula are suitable);
- give the baby complex preparations such as Baby Calm or Plantex, which facilitate digestive processes, improve bowel function, and stimulate enzyme secretion;
- play with the child more often, stimulating his motor activity;
- do light exercises and massage the abdomen.
The mother herself, who is breastfeeding, should monitor her own hygiene, as well as review her diet. It is advisable to exclude rice, peas with beans, cabbage, grapes and blueberries from the menu. Such recommendations are especially relevant if Staphylococcus aureus is found in the stool of an infant.
The basic directions in the treatment of the baby should be the strengthening of the protective reaction of the body and the stabilization of metabolic processes. It is very important that lactation is not interrupted, since breast milk is the main factor in healthy children's immunity.
If the baby has symptoms of an inflammatory process, stool changes are observed, the temperature rises, then the doctor in the vast majority of cases will prescribe antibiotic therapy.
Medications
A few decades ago, the main antibiotics that were prescribed for Staphylococcus aureus were penicillin preparations. They cured purulent processes, stopped the development of septic complications. But Staphylococcus aureus eventually developed resistance to penicillins and "learned" to quickly destroy and neutralize the antibiotic.
Despite this, some penicillin preparations - mostly belonging to the latest generations - are still used to suppress staphylococcal infections. These drugs include, for example, Oxacillin, Amoxicillin, etc. Antibiotics of the cephalosporin group are no less effective - for example, we are talking about Cefazolin, Cefuroxime.
With a more complex course of pathology, the following is prescribed:
- Vancomycin for newborns is prescribed at the rate of 15 mg / kg of body weight per day, and for infants from one month old, 10 mg / kg of body weight is administered twice a day. During therapy, mandatory monitoring of the concentration of the drug in the blood serum is required. Intramuscular injections of Vancomycin are very painful, therefore, drip intravenous administration of the drug is preferable.
- Clindamycin is not recommended for use in children under six years of age, but may be prescribed if indicated by the doctor if such an appointment is necessary. The dosage is calculated individually. Possible side effects are digestive disorders, impaired immunity.
- Co-trimoxazone is used to treat children from 3 months of age. The dosage for infants up to six months is determined at the rate of ¼ tablet twice a day. After six months, the child can be given half a tablet twice a day, at the same time. The duration of treatment is up to one week. Side effects: allergies, digestive disorders.
- Doxycycline and Minocycline are not recommended for small children, but correction is possible at the discretion of the doctor.
Which of the medicines to choose, the doctor decides. He also, if necessary, makes adjustments to the standard therapeutic regimen.
Immediately before the start of treatment, it is recommended to pass an analysis that determines the sensitivity of bacteria to antibiotic therapy.
Enterofuril with Staphylococcus aureus in infants
Enterofuril is an effective and relatively safe antibacterial drug, so it is actively used for Staphylococcus aureus in infants and older children. The tool has the necessary therapeutic effect, thanks to the active component nifuroxidase - a bactericidal substance with a wide spectrum of activity, which disrupts the production of the dehydrogenase enzyme and prevents the growth of bacteria.
Enterofuril acts strictly selectively, so the vast majority of beneficial microflora does not suffer. In addition, resistance to the drug is practically not developed, systemic action does not occur.[10]
The drug is indicated for the treatment of staphylococcal infections in children from the age of one month. Enterofuril is usually well tolerated, and side effects are extremely rare and are manifested only by an allergic response to the administration of the drug.
Treatment of Staphylococcus aureus in infants with a bacteriophage
Staphylococcal sepsis, enterocolitis in infants and newborns often require the administration of a bacteriophage in the form of high enemas (via a catheter or gas tube) two to three times a day in an amount of 5-10 ml. If vomiting and regurgitation are absent, then bacteriophage can be administered orally, mixed with breast milk. Sometimes combined treatment is practiced, alternating oral and enema administration of the drug. The average duration of the treatment course is from five to fifteen days.
If relapses of infection are observed, then the course of bacteriophage is repeated.
If it is necessary to treat omphalitis, pustular skin lesions, the bacteriophage is applied by applicator, every day in the morning and evening: a gauze napkin is treated with a bacteriophage and applied to the affected area.
Prevention
Preventive measures against Staphylococcus aureus are simple, few of them, but they are all very important for ensuring the health of a small child. And they are as follows:
- hygiene, both mother and baby;
- support and strengthening of the immune defense of the baby;
- limiting the communication of strangers with a small child, avoiding visiting public places;
- ensuring the full and competent nutrition of the mother, the establishment of breastfeeding of the baby;
- providing care for the baby, with hygiene not only of the hands, but also of the mother's breasts, clothes, bed linen, toys, dishes, any items in the house.
Staphylococcus aureus is considered a rather unfavorable microorganism, therefore, in no case should you try to get rid of the bacterium on your own. At the first symptoms of an infectious pathology, the help of a medical specialist must be followed.
Forecast
Further prognosis depends on the complexity of the infection and on the timeliness and effectiveness of the prescribed therapy. Of particular danger is Staphylococcus aureus in infants, since it can provoke septic complications, infectious-toxic shock, coma, and even death of the patient. With an uncomplicated infection, the prognosis can be considered favorable, but a generalized lesion - for example, with the development of sepsis - ends in death in about half of the cases.

