Hypogalactia
Last reviewed: 07.06.2024

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.

Homo sapiens belongs to the class of mammals, and when a child is born, it switches from intrauterine hematotrophy to lactotrophy - feeding on mother's milk (from Latin lactis - milk). Hypogalactia is simply a lack of milk (from Greek gala - milk) in a nursing mother, i.e. A decrease in lactation or secretion of breast milk in daily volumes that do not fully meet the nutritional needs of her child.
This term, as well as the term "oligogalactia" (from Greek oligos - few and gala - milk) is used only after the mother's milk "comes in", which usually occurs about 30-40 hours after the birth of a full-term baby. The milk supply may start later than usual (during the first 72 hours after delivery), but thereafter it is produced in sufficient quantities, and in such cases delayed lactogenesis (observed in one third of breastfeeding women) is defined. [1]
Epidemiology
According to some reports, primary lactational insufficiency occurs in nearly 5% of women despite adequate number of feedings and proper feeding technique.
And the lack of milk 2-3 weeks after the birth of the child complains of at least 15% of healthy mothers who gave birth to their firstborn, and in 80-85% of cases hypogalactia is secondary.
Causes of the hypogalactia
Specialists have identified key causes of hypolactia as:
- Complicated postpartum period;
- Hypoplasia of the mammary glands (lack of glandular tissue that produces milk, although the size of the breasts may be significant);
- Diffuse breast changes and other forms of mastitis;
- Retention of placental fragments in the uterus after delivery;
- Congenital or drug-induced hypoprolactinemia - a deficiency of the hormone prolactin, which ensures milk production;
- Labor complicated by massive hemorrhage with the development of sheehan syndrome - postpartum pituitary insufficiency and decreased prolactin production;
- Insufficient levels of a key hormone in breastfeeding - oxytocin;
- Suppression of the milk ejection reflex - the milk ejection reflex - by negative emotions, pain, stress.
Hypogalactia can also be associated with problems of lacto- or galactopoiesis - autocrine maintenance of already established lactation. And here, the most important role is played by the excretion of milk from the breast (the degree of its emptying), that is, suckling it by the baby. A decrease in the amount of milk at this stage may be the result:
- Not feeding the child often enough (not on demand, but "on schedule") or incorrect feeding technique;
- Inability of the baby to suckle effectively, particularly if the baby is premature or low birth weight;
- Neglecting to decant residual milk, for more information see breast milk decanting: why and how is it done?
- Congestion in the breasts - lactostasis, leading to lactation mastitis.
Risk factors
Risk factors for inadequate breast milk secretion include:
- The age of the breastfeeding mother is 36-40 years or older;
- Benign tumors of the uterus and ovaries;
- Gestosis (late toxicosis) during pregnancy;
- Cesarean delivery;
- Insufficient and/or improper nutrition of the breastfeeding mother;
- Obstruction of the ducts of the mammary glands;
- Complicating a newborn's good breast grasp retracted nipples;
- Stress, depression after childbirth (to which almost 20% of women in labor are affected), neurotic disorders;
- Surgery or trauma to the breast (with possible disruption of the milk ducts);
- Prolonged use of corticosteroids, diuretics, adrenomimetics, hormonal contraceptives, hormone replacement therapy with gestagens;
- Diabetes;
- Obesity;
- Psychosocial factors;
- Bad habits.
And the risk of prolactin deficiency is increased in: ovarian dysfunction, hypothyroidism, problems with the adrenal glands and hypothalamic-pituitary system, and certain autoimmune diseases.
Pathogenesis
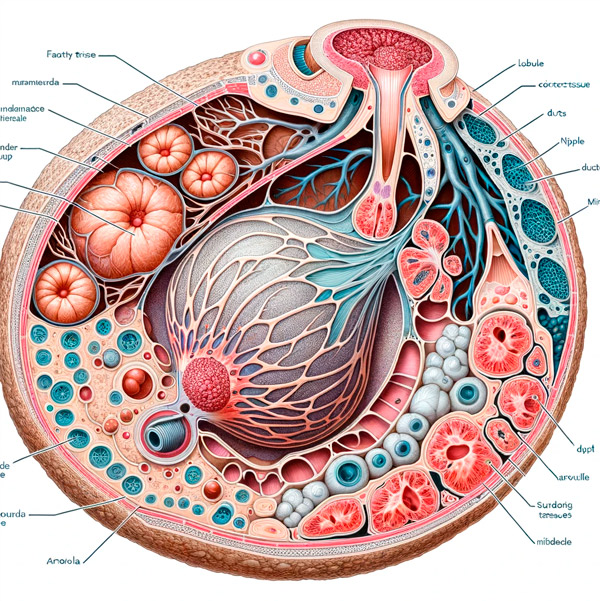
Both biochemically and physiologically, adequate breastfeeding depends on lactation, a complex process of breast milk production.
In some cases, the pathogenesis of its insufficient production is due to decreased secretion of the corresponding hormones of the hypothalamic-pituitary system: prolactin and oxytocin. Prolactin biosynthesis occurs in specialized lactotrophic cells of the anterior lobe of the pituitary gland under the influence of high estrogen levels, and during pregnancy the number of these cells and the pituitary gland itself increases.
In addition, during pregnancy, prolactin is synthesized by the cells of the decidual layer of the placenta thanks to placental lactogen, a hormone secreted from the second month of pregnancy, and prolactin is involved in the maturation of the mammary glands until delivery. After birth, prolactin levels remain high only as long as breastfeeding continues. Suckling triggers the mechanism that allows prolactin to be secreted and therefore milk to be produced. If breastfeeding is intermittent, prolactin drops back to baseline within two weeks.
Oxytocin is produced by large neuroendocrine cells in the hypothalamic nuclei and transported to the posterior lobe of the pituitary gland, where it is accumulated and then secreted into the blood. During lactation, oxytocin entering the bloodstream plays an important role: it induces contractions of myoepithelial cells surrounding the alveoli of the mammary gland, which leads to the release of milk from the breast. Stress (increased blood cortisol levels) and medical interventions during labor can reduce the release of oxytocin, negatively affecting the initiation of breastfeeding.
The main in the mechanism of decreased lactation with insufficiently frequent feeding of the child - the lack of the necessary level of stimulation of the nipples to manifest the so-called milk ejection reflex. Its essence is that sucking activates sensory nerve endings in the nipple and its areola, the resulting afferent signals are transmitted to the hypothalamus, which leads to the release of oxytocin in the blood. And this hormone, as noted above, "forces" the muscle cells of the mammary gland to contract and "push" milk from the alveolar lumen into the ducts.
If part of the placenta is retained, there is an increase in the level of the lactation-suppressing hormone progesterone.
Inability of a baby to suckle effectively due to prematurity is associated with incomplete functional maturation and practical absence of the suckling reflex; in a baby born at term, feeding problems may be due to congenital maxillofacial defects (cleft palate) or ankyloglossia - short frenulum.
Symptoms of the hypogalactia
Recognized by pediatricians as reliable signs of hypogalactia include:
- Neonatal weight loss of ˃7-10% of initial birth weight (with adequate feeding, newborns should regain their birth weight in two weeks);
- Insufficient and irregular weight gain of the child - less than 500 g per month or up to 125 g per week (while the weight gain of a full-term infant during the first month is 600 g, and during each month of the first six months of life - up to 800 g);
- Decrease in the number of urination and defecation (at 3-5 days of age the child can urinate up to 5 times and defecate up to 4 times a day, by the age of a week should be 4-6 urination and 3-6 defecation per day);
- Insignificant amount of urine, with the urine being intensely yellow in color, with a pungent odor;
- With infrequent defecation, the consistency of the stool is dense.
In addition to underweight, lethargy and frequent crying, signs of starvation of the child in hypogalactia in the mother consist of pale skin and loss of tissue turgor, an insignificant amount of subcutaneous tissue on the trunk and abdomen (with a decrease in skin folds at the level of the navel), a decrease in the weight-growth ratio (the ratio of body weight in grams to body length in cm), as well as the fatness index (the ratio of the circumference of the shoulder, thigh and shin).
In a breastfeeding mother, symptoms of decreased breast milk secretion include insufficient swelling of the mammary glands (indicating milk "coming up") and no milk in the breast when decanting after a feeding.
Stages
Degrees of hypogalactia are determined as a percentage of the child's daily need: with a lack of milk less than 25% of the need - I degree (mild); from 25 to 50% - II degree (moderate); from 50 to 75% - III degree (medium); over 75% - IV degree (severe).
Forms
A distinction is made between types of hypogalactia such as:
- Early hypogalactia, when insufficient breast milk production is noted from the time of birth during the first decade;
- Late hypogalactia (develops later in life);
- Primary hypogalactia, observed in women with certain diseases, neuroendocrine pathologies or anatomical problems (insufficient amount of glandular tissue in the mammary glands); after previous breast surgeries; in the delay of the placenta fragment or after severe labor with massive bleeding;
- Secondary hypogalactia, the causative factors of which include delayed breastfeeding of the infant after delivery, improper feeding regimen, incomplete emptying of the mammary glands of milk residues, unjustified bottle feeding of infant formula, etc.;
- Transient or transient hypogalactia with delayed onset of lactogenesis may be due to hot weather, colds and other ailments of a nursing woman (with fever), changes in her psycho-emotional state, fatigue, frequent sleep deprivation. It is characteristic of lactating women with obesity, insulin-dependent diabetes and long-term treatment with corticosteroids.
Lactation can decrease as the baby grows, and maintaining the required amount of milk as the baby gets older can be problematic. An infant usually needs about 150 ml/kg per day, and while an infant weighing 3.5 kg needs 525 ml of milk per day, an infant weighing 6-8 kg needs 900-1200 ml.
It should be borne in mind that at 3, 7 and 12 months of lactation there are so-called hunger crises: the baby needs more milk due to its growing mobility and increased nutritional needs during the periods of the most intensive growth.
Complications and consequences
Maternal hypogalactia in children leads to dehydration and protein-energy deficiency - hypotrophy of the newborn - with possible impaired growth and development.
Also, complications and consequences of insufficient consumption of mother's milk can manifest themselves in a decrease in complex immune defense and increased susceptibility to infectious diseases, primarily viral respiratory diseases.
In mothers with oligogalactia, when breastfeeding, the baby tries to suckle more vigorously, which combined with increased feeding time leads to irritation of the nipple skin - with maceration, cracking and inflammation.
Diagnostics of the hypogalactia
As noted by experts, it is not uncommon for women to be convinced that they do not have enough milk due to restless behavior and frequent crying of the infant. And in order to identify hypogalactia, a diagnosis is carried out, which begins with the collection of anamnesis.
The pediatrician examines the child, checks the indicators of his body weight, from the words of the mother records the intensity and nature of urination and defecation.
To verify insufficient lactation, control feedings are carried out: weighing the baby before and after it, checking the correctness of putting to the breast, the baby's grip on the nipple, the intensity of sucking and its duration.
Any changes in her breasts during pregnancy and after delivery are discussed with the mother. Her blood tests for prolactin, estradiol and progesterone levels are also taken.
Instrumental diagnosis is limited to ultrasound of the mammary glands. If a pituitary lesion is suspected, CT and MRI of the brain may be performed. However, in most cases, careful history taking and control measurements are sufficient to confirm the diagnosis.
Differential diagnosis
The differential diagnosis of such conditions as lactostasis, complete absence of breast milk secretion in the mother - agalactia and hypogalactia, delayed onset of lactation, as well as hypogalactia and lactation crisis, that is, a temporary decrease in breast milk production due to postpartum hormonal changes in the mother's body.
It may be necessary to consult other specialists (mammologist, gynecologist, endocrinologist).
Treatment of the hypogalactia
In order to correct the situation with decreased breast milk secretion, it is first of all necessary to adhere to the principles of successful breastfeeding and make adjustments in its technique.
For example, the optimal method is to place the baby on both breasts when they are fully emptied in order to stimulate lactation and also to prevent cracked nipples. Feeding with one breast should not take longer than 15 minutes until it is completely empty, and then - if the baby needs more milk - continue feeding with the other breast. The next feeding should be started from this breast.
Detailed narrative in the materials:
The main methods of treatment of hypogalactia:
The most commonly used medicines are listed in the publication - lactation-enhancing drugs
The task of the mother's body is to support the production of milk with the necessary quality composition for the child, and it is solved by increasing the intake of energy and nutrients from food. Therefore, special attention should be paid to nutrition and diet in hypogalactia, read more:
The average breastfeeding mother produces 850 ml of breast milk per day, and she needs to consume enough food to cover all the components excreted with milk. During lactation, the daily calorie intake should be at least 2200-2500 kcal. Recommended by WHO experts daily norms of vitamins are: vitamin A - 1.2 mg; vitamin C - 100 mg; vitamin D-12.5 mcg; vitamin E - 11 mcg; riboflavin (vitamin B2) - 1.8 mg; pyridoxine (vitamin B6) - 2.5 mg; folic acid (vitamin B9) - 0.5 mg; nicotinic acid in hypogalactia (niacin, nicotinamide, vitamin B3 or PP) - 18-20 mg. Niacin is essential for coenzyme systems that are involved in the synthesis of fatty acids and steroids (including cholesterol). Niacin deficiency is rare because the daily requirement can usually be met through the consumption of meat, grains, and dairy products. If a nursing woman's diet provides adequate amounts of this vitamin, niacin supplementation is not required.
To increase the amount of breast milk, herbs with "lactic" effect (in the form of decoctions) are used, including: fenugreek, fennel, anise, alfalfa, goatgrass (galega), verbena, milk thistle, nettle, oats (grains), red raspberry leaf, watercress (cress). However, the side effects of many herbal remedies should be considered. For example, fenugreek seed can cause hypoglycemia, increased BP and diarrhea; galega - decreased BP and blood sugar levels; milk thistle - allergic reactions and intestinal upset.
According to experts, supplemental formula or donor milk should be given only when medically necessary (when all attempts to increase breast milk secretion have failed) and indications for supplementation include the above signs of starvation in the infant, as well as when low lactation is due to factors such as insufficient glandular tissue in the mammary glands, etc.
Read more in the publications:
Prevention
In accordance with WHO recommendations, prevention of breastfeeding disorders involves observation of a pregnant woman by an obstetrician-gynecologist to prevent complications of pregnancy and childbirth and timely treatment of associated diseases.
While carrying a child, expectant mothers (especially if the firstborn is expected in the family) should undergo prenatal breastfeeding education, including training of parents in methods of prevention of hypogalactia, one of which is a free feeding schedule: the time of feeding the infant should depend on its nutritional needs, including at night.
Forecast
Early putting the baby to the breast, ensuring round-the-clock cohabitation of mother and child, establishing a feeding regime on demand, as well as adequate medical care in case of decreased secretion of breast milk provide a favorable prognosis for most forms of secondary hypogalactia.

