Medical expert of the article
New publications
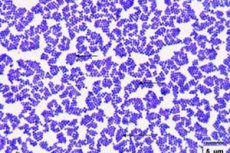
Staphylococcus aureus in an infant.
Last reviewed: 05.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Staphylococci are widespread in the environment and can be represented by both opportunistic and pathogenic microorganisms. The most pathogenic is Staphylococcus aureus, which can cause the development of purulent inflammatory processes in various organs and tissues. Staphylococcus aureus is especially dangerous in infants - primarily due to inadequate child immune protection. What do you need to know about this bacterium, and what steps should be taken if the baby has positive test results?
Epidemiology
According to statistics, every third child has Staphylococcus aureus on their skin or mucous membranes. As a rule, this is a carrier of an infection, which, however, can later enter the body and provoke the development of various pathologies - from furunculosis to pneumonia and even sepsis. [ 1 ]
Most often, the bacteria is found in children in their first year of life. Then, with age, the degree of seeding gradually decreases. The pathogen is seeded mainly from the mucous membrane of the nasal cavity and tonsils, but other localizations also occur. [ 2 ]
Staphylococcus aureus causes more than 60% of existing staphylococcal infections. Saprophytic and epidermal staphylococci are found somewhat less frequently. [ 3 ]
Causes of staphylococcus aureus in a newborn.
Staphylococcus aureus can easily live in the body of any person – but only in small quantities. Active reproduction of bacteria begins against the background of a sharp weakening of the immune defense, or with other stress factors. [ 4 ]
Infants are most susceptible to active growth and infection development. Small children do not yet have the necessary antibodies, and their immunity is weak and inadequate.
Staphylococcus aureus in infants can appear:
- when infected by one's own mother - for example, during childbirth or breastfeeding;
- from medical workers in the maternity hospital, hospital, clinic;
- through direct contact with a sick person (carrier);
- upon contact with objects infected with Staphylococcus aureus (toys, dishes, etc.)
Risk factors
Those at risk typically include:
- children born prematurely;
- babies who have been on artificial feeding since birth;
- weak, underweight infants;
- children with congenital defects and diseases;
- infants who have been treated with antibiotics, hormonal drugs, or children diagnosed with intestinal dysbacteriosis;
- children living in unfavorable sanitary conditions, with inadequate hygiene standards, and with poor nutrition.
Pathogenesis
Staphylococcus aureus is one of the most pathogenic types of such bacteria. However, the presence of this microbe in healthy human microflora is not excluded.
Staphylococcus aureus received such an unusual name due to its ability to form a specific pigment substance, which, when examined microscopically, has a characteristic orange-yellow hue. This bacterium is resistant to medications, can “survive” boiling, exposure to ultraviolet light, and prolonged drying. Strong saline solutions and hydrogen peroxide do not affect it, so the bacterium lives and reproduces well in almost any conditions. [ 5 ]
Staphylococcus aureus has pronounced enzymatic activity and secretes:
- lipase, which breaks down fats, allowing bacteria to easily overcome the skin barrier and enter the bloodstream;
- coagulase, which helps create protection for bacteria from immune cells;
- penicillinase, which provides bacteria with resistance to penicillin drugs.
In addition, Staphylococcus aureus excretes endo- and exotoxic substances that cause severe intoxication. This microbe exhibits strong resistance to medications, is prone to frequent mutation, so it is quite difficult to get rid of it.
One of the most unfavorable mutations of the microbe is considered to be methicillin-resistant staphylococcus: it occurs mainly as a hospital-acquired infection.
How is Staphylococcus aureus transmitted to infants?
A child can become infected with Staphylococcus aureus anywhere – at home, on the street, from his own mother, and also from certain foods or water.
Since the bacterium is very resistant, it is often found in hospitals and clinics: if all existing sanitary standards are observed, the microbe is capable of mutating to such an extent that it becomes resistant to almost any processing solution. [ 6 ]
There are several known ways in which Staphylococcus aureus can get into a baby's body:
- contact household method – involves the transmission of infection through objects contaminated with bacteria (toys, linen, towels, dishes, etc.);
- airborne transmission – involves the transmission of bacteria through the air with coughing, sneezing, etc.;
- feco-oral route – involves the spread of germs through unwashed hands, the mother’s breast (during breastfeeding);
- vertical method – involves the transfer of infection to the baby from its mother during pregnancy or during childbirth (during passage through the birth canal).
Another possible transmission option is considered to be the consumption of mother's milk by the baby if the mother suffers from infectious mastitis.
Symptoms of staphylococcus aureus in a newborn.
Staphylococcus aureus in the active stage usually reveals itself with the following symptoms:
- the baby's temperature rises sharply;
- clear signs of rhinitis appear;
- the child is lethargic, capricious, refuses to eat, cries;
- attacks of nausea and vomiting are possible;
- a cough appears;
- the eyes swell and become red, possibly with tearing;
- the stool becomes unstable (periods of constipation and diarrhea alternate);
- the baby loses weight (primarily due to loss of appetite);
- the balance of intestinal microflora is disturbed);
- the skin becomes covered with a rash and other pathological elements – these can be pimples, pustules, itchy nodules, peeling areas.
The incubation period for activation of Staphylococcus aureus can range from 3 hours to 4-5 days. In this case, the pathogen can only be accurately identified after sowing.
The norm of golden staphylococcus in infants
Staphylococcus aureus can be found on the skin and mucous membranes of an infant, as well as in the intestines, nasal cavity, and tonsils. If there is any suspicion of infection, the infant undergoes an analysis that will accurately indicate whether there is a pathology or not.
Determining the presence and quantity of Staphylococcus aureus may be necessary to assess the need for treatment: if the number of bacteria is within acceptable limits and there are no clinical symptoms, then treatment is not carried out. For example, Staphylococcus aureus can be detected in the intestinal cavity in almost all cases, and this is not a reason for therapy. However, if the number of bacteria is exceeded, then measures must be taken, otherwise unpleasant pathological signs will follow in the form of infectious colitis, colic and other digestive disorders.
The presence of Staphylococcus aureus does not always indicate an infectious lesion, as it may be an asymptomatic carrier. A smear from the nasal cavity and pharyngeal mucosa with a determination of the number of microbes up to 10 3 is considered a normal non-pathological carrier. Exceeding this indicator can cause the development of infectious and inflammatory diseases. In children over 1 year old, the norm is slightly higher - up to 10 4.
The mere presence of Staphylococcus aureus cannot be a reason for prescribing drug therapy.
The number of staphylococci should be determined before the start of treatment and after its completion. Subsequently, it is necessary to control the number of bacteria for a couple of months after the therapeutic course. [ 7 ]
Staphylococcus aureus in infant feces
A stool test may be prescribed for the baby already in the maternity hospital if there is a suspicion of Staphylococcus aureus. The stool is examined at least twice - for example, with an interval of one or two days. The material for analysis is provided to the laboratory as soon as possible - preferably immediately after bowel movement, but no later than 3 hours after it. Such timeframes directly affect the accuracy of the results.
The maximum permissible level of Staphylococcus aureus in feces can be 10 3 10 4.
Even if the number of bacteria is within the normal range, the doctor will advise monitoring its dynamics, since further rapid proliferation of the infection is possible, which will require urgent treatment. If the number of golden staphylococci changes insignificantly, then we can talk about the normal health of the baby.
Manifestation of Staphylococcus aureus on the skin of newborns
Staphylococcus aureus is capable of manifesting itself in any organ and on any tissue of the human body. And this is what makes the bacteria especially dangerous.
Skin manifestations in children may vary depending on the form of staphylococcal infection:
- Staphylococcal folliculitis is manifested by an inflammatory process at the tips of hair follicles: the skin around the follicle turns red, a pustule or abscess forms, which after opening reveals a crust or ulcer. Quite large areas can be affected - mainly in the face or head area.
- Staphylococcal hidradenitis is an inflammation of the sweat glands that can be found on almost any part of the body. Pustules (pimples) and areas of swelling are observed.
- Furuncles are usually painful and can affect the face, back, and neck. Carbuncles are more complex: the affected skin areas become bluish, specific purulent funnels form, and the temperature may rise.
Even if the above pathological signs are detected, the infant is not treated until the test results are received: it is imperative to ensure that the skin disorder is not caused by other unfavorable factors.
Staphylococcus aureus in a baby's nose
Staphylococcus aureus is often isolated from the nasal cavity, but its presence does not always indicate the presence of the disease. Only when the permissible indicators are exceeded do the first signs of infection appear:
- whitish or greenish-yellow discharge;
- increased temperature, fever;
- signs of general intoxication;
- general malaise, headaches, nausea, loss of appetite.
In the future, Staphylococcus aureus can become an impetus for the development of such pathologies as sinusitis, frontal sinusitis. The pathological condition is aggravated by frequent and uncontrolled use of nasal vasoconstrictors, self-medication with antibacterial agents, incomplete or improperly conducted course of antibiotic therapy.
Complications and consequences
Staphylococcus aureus in infants can provoke a generalized pathological process, since the microbe can spread unhindered, affecting many tissues and organs. At the same time, there is a danger even with an initial small manifestation of the disease on the skin: in the absence of treatment, infantile phlegmon develops within a short time, which is a purulent-inflammatory reaction in adipose tissue, with the further formation of a necrotic process. [ 8 ]
In cases where the infectious carrier is the child's mother, Staphylococcus aureus can easily penetrate into the child's intestinal cavity (this happens during breastfeeding). Such a mechanism causes serious disruptions in the digestive tract. As a result, the growth and development of the baby is disrupted.
In addition, Staphylococcus aureus can penetrate from the tissues into the bloodstream, with the further development of an extensive pathological process: we are talking about septic complications that threaten the life of the infant. [ 9 ]
Diagnostics of staphylococcus aureus in a newborn.
Diagnostic measures for the detection of Staphylococcus aureus primarily include the use of serological tests, namely:
- The generally accepted coagulase test with a test tube, the test duration is from four to 24 hours;
- latex agglutination reaction, using latex particles coupled with antibodies to staphylococcus (meaning A-protein, adhesion factor and a number of surface antigens).
In addition, the following tests may be useful in diagnostics:
- general clinical studies of blood and urine (in case of staphylococcal infection, the blood shows an increased content of leukocytes and neutrophils, an accelerated ESR, and protein, leukocytes and staphylococci are found in the urine);
- biological seeding on an appropriate nutrient medium.
Sowing is necessary to identify the infectious agent and determine its sensitivity to antibiotic therapy. Fecal sowing is possible no later than 3 hours after defecation. A smear from the oral cavity and nasopharynx is taken before eating and taking any medications.
In case of skin lesions, it is important to take a smear from the affected areas after mechanical cleaning and treatment of the wound surface with antiseptic preparations.
Instrumental diagnostics involves the use of the following procedures:
- The agglutination reaction is carried out to determine the dynamics of the pathology and assess the effectiveness of the selected therapy. The study is repeated at least twice with an interval of 1-1.5 weeks. If the antibody titers in the blood increase and exceed 1:100, this indicates that the infection is progressing.
- Phage typing of plasma-coagulating Staphylococcus aureus helps to determine the degree of sensitivity of microorganisms to viral phages for the further selection of therapeutic measures.
Differential diagnostics in the laboratory are carried out with streptococcal infection.
Treatment of staphylococcus aureus in a newborn.
If the amount of Staphylococcus aureus in the infant's body exceeds the permissible levels, then the pathology should be treated under the supervision of a doctor, following all his instructions. Additionally, parents can take the following measures:
- bathe the child in herbal decoctions (decoctions and infusions of chamomile, sage, calendula are suitable);
- give your baby complex preparations such as Baby Calm or Plantex, which facilitate digestive processes, improve bowel function, and stimulate enzyme secretion;
- play with your child more often, stimulating his physical activity;
- do light gymnastics and abdominal massage.
The mother who is breastfeeding should monitor her own hygiene and also review her diet. It is advisable to exclude rice, peas and beans, cabbage, grapes and blueberries from the menu. Such recommendations are especially relevant if Staphylococcus aureus is found in the stool of an infant.
The basic directions in the treatment of the baby should be strengthening the body's defense reaction and stabilizing metabolic processes. It is very important that lactation is not interrupted, since breast milk is the main factor in healthy child immunity.
If a baby shows symptoms of an inflammatory process, changes in stool, or an elevated temperature, then in the vast majority of cases the doctor will prescribe antibiotic therapy.
Medicines
Just a few decades ago, the main antibiotics prescribed for Staphylococcus aureus were penicillin-type drugs. They cured purulent processes and stopped the development of septic complications. But Staphylococcus aureus eventually developed resistance to penicillins and “learned” to quickly destroy and neutralize the antibiotic.
Despite this, some penicillin drugs – mainly those belonging to the latest generations – are still used to suppress staphylococcal infections. Such drugs include, for example, Oxacillin, Amoxicillin, etc. No less effective are antibiotics of the cephalosporin group – for example, we are talking about Cefazolin, Cefuroxime.
In case of more complicated course of the pathology the following is prescribed:
- Vancomycin is prescribed to newborns at a rate of 15 mg/kg of weight per day, and to infants from one month of age, 10 mg/kg of weight is administered twice a day. During therapy, mandatory monitoring of the drug concentration in the blood serum is required. Intramuscular injections of Vancomycin are very painful, so intravenous drip administration of the drug is preferable.
- Clindamycin is not recommended for use in children under six years of age, but may be prescribed according to indications if the doctor considers such a prescription necessary. The dosage is calculated individually. Possible side effects are digestive disorders, impaired immunity.
- Co-trimoxazone is used to treat children from 3 months of age. The dosage for infants up to six months is determined at the rate of ¼ tablet twice a day. After six months, the child can be given half a tablet twice a day, at the same time. Duration of treatment is up to one week. Side effects: allergy, digestive disorders.
- Doxycycline and Minocycline are not recommended for use in young children, but adjustments may be made at the discretion of the physician.
The doctor decides which medication to choose. He also makes adjustments to the standard therapeutic regimen if necessary.
Immediately before starting treatment, it is recommended to take a test to determine the sensitivity of the bacteria to antibiotic therapy.
Enterofuril for Staphylococcus aureus in infants
Enterofuril is an effective and relatively safe antibacterial drug, so it is actively used for Staphylococcus aureus in infants and older children. The drug has the necessary therapeutic effect due to the active component nifuroxidase - a bactericidal substance with a wide spectrum of activity, which disrupts the production of the enzyme dehydrogenase and prevents the proliferation of bacteria.
Enterofuril acts strictly selectively, so the overwhelming majority of beneficial microflora is not affected. In addition, resistance to the drug is practically not developed, and there is no systemic effect. [ 10 ]
The drug is indicated for the treatment of staphylococcal infection in children, starting from one month of age. Enterofuril is usually well tolerated, and side effects are extremely rare and manifest themselves only as an allergic response to the administration of the drug.
Treatment of Staphylococcus aureus in infants with bacteriophage
Staphylococcal sepsis, enterocolitis in infants and newborns often require the administration of bacteriophage in the form of high enemas (via a catheter or gas tube) two to three times a day in an amount of 5-10 ml. If vomiting and regurgitation are absent, the bacteriophage can be administered orally, mixing it with breast milk. Sometimes combined treatment is practiced, alternating oral and enema administration of the drug. The average duration of the treatment course is from five to fifteen days.
If relapses of the infection are observed, the bacteriophage course is repeated.
If it is necessary to treat omphalitis, pustular skin lesions, the bacteriophage is applied by applicator, every day in the morning and evening: a gauze napkin is treated with the bacteriophage and applied to the affected area.
Prevention
Preventive measures against Staphylococcus aureus are simple, there are not many of them, but they are all very important for ensuring the health of a small child. And they are as follows:
- maintaining hygiene for both mother and baby;
- support and strengthening of the infant's immune defense;
- limiting communication between strangers and a small child, avoiding visiting public places;
- ensuring the mother's complete and proper nutrition, establishing breastfeeding of the baby;
- providing care for the baby, with hygiene not only of the hands, but also of the mother's breast, clothes, bed linen, toys, dishes, and any objects in the house.
Staphylococcus aureus is considered a rather unfavorable microorganism, so in no case should you try to get rid of the bacteria on your own. At the first symptoms of an infectious pathology, the help of a medical specialist must follow.
Forecast
The further prognosis depends on the complexity of the infectious lesion and the timeliness and effectiveness of the prescribed therapy. Staphylococcus aureus in infants is especially dangerous, as it can provoke septic complications, infectious-toxic shock, coma and even death of the patient. In case of uncomplicated infection, the prognosis can be considered favorable, but generalized damage - for example, with the development of sepsis - ends fatally in about half of the cases.

