Medical expert of the article
New publications
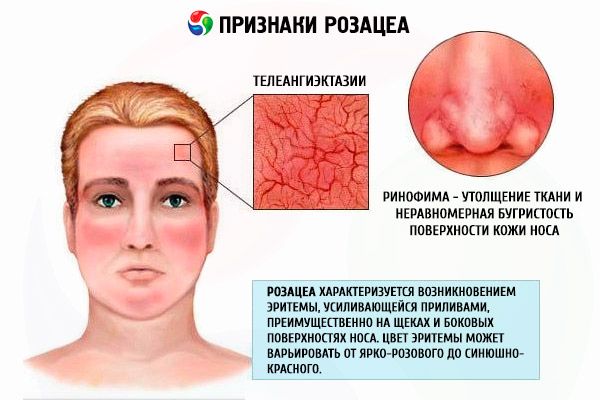
Rosacea
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Rosacea is one of the most common skin diseases that a practicing dermatologist has to deal with. The history of studying rosacea is long and convoluted. The main symptoms of the disease have been known since ancient times and have practically not been subject to pathomorphosis, but there is still no generally accepted definition of this disease.
Abroad, the accepted clinical definition of rosacea is a disease manifested by persistent erythema of the central part of the face, especially protruding surfaces, with dilated skin vessels clearly visible against its background, often accompanied by the appearance of papular and papulopustular rashes, as well as the possible development of cone-shaped deformities of the protruding parts of the face.
 [ 1 ]
[ 1 ]
Causes rosacea
Rosacea is most often defined as an angioneurosis of the predominantly venous link of the vascular plexus of the dermis, based on the most widely accepted hypothesis of the pathogenesis of the disease.
The disease most often develops in females, in the second to fourth decade of life, who have a genetically determined predisposition to transient reddening of the skin of the face, less often the neck and the so-called décolleté area.
Since the pathological changes in the skin of patients with rosacea are localized mainly on the face, the cosmetic significance of the disease and the occurrence of secondary psychosomatic problems of patients with rosacea have led to very active participation of society in the study of this disease. As a result, national societies for the study of rosacea have been formed in developed countries, representing very influential commissions of professionals who monitor periodicals on the problem and provide, among other things, financial support for research in this area. Being a kind of information centers, these societies regularly publish modern generalized views of experts on issues of classification, pathogenesis and treatment methods. Often these views do not correspond to historically established ones.
Pathogenesis
The pathogenesis of rosacea remains unclear. There are many theories, but none of them claims to be the leading one, since it has not been fully proven. Some of these theories are based on the results of systematic studies on the relationship between the development of rosacea and various initiating factors and disorders, others - on the results of individual observations.
The main etiopathogenetic mechanisms are considered to be vasodilation of the vascular plexus of the dermis due to the implementation of the congenital feature of the hypothalamic-pituitary vasomotor activity, as one of the mechanisms of thermoregulation of the brain under conditions of increased temperature (as a result of the action of physical or psychoemotional factors), and the associated blood flow in the carotid artery basin.
The effect of ultraviolet radiation, which, according to many researchers, leads to the early development of telangiectasias, has not been fully explained, and its role in the pathogenesis of rosacea continues to be debated. The combination of paretically dilated vessels and prolonged UFO leads to dystrophic changes in the intercellular matrix of the dermis and partial disorganization of fibrous structures of connective tissue due to the accumulation of metabolites and proinflammatory mediators. This mechanism is considered one of the main ones in the development of hypertrophic rosacea.
Colonization of the digestive system by one of the subpopulations of Helicobacter pylori, which produces cytotoxic substances that stimulate the release of vasoactive substances such as histamine, leukotrienes, prostaglandins, tumor necrosis factor and some other cytokines, is considered one of the main causes of the development of erythematotelangiectatic rosacea.

Excessive consumption of alcohol, spicy food and spices is currently considered only a factor that increases the manifestations of the disease, but has no etiological significance. Just as the role of Demodex folliculorurn, which is a typical commensal, is currently recognized as a factor in the exacerbation of the skin process mainly in the papular-pustular type of rosacea.
Symptoms rosacea
The clinical picture of erythematotelangiectatic rosacea is characterized by the appearance of erythema, initially transient, increasing with flushes, and then becoming persistent, mainly on the cheeks and lateral surfaces of the nose. The color of the erythema can vary from bright pink to bluish-red, depending on the duration of the disease. Against the background of such erythema, patients develop telangiectasias of various diameters, scanty or moderate peeling and swelling of the skin. Most patients complain of a burning and tingling sensation in the area of erythema.
The manifestations of the disease are aggravated by exposure to low and high temperatures, alcohol, spicy food and psycho-emotional stress. Patients with this type of rosacea are characterized by increased sensitivity of the skin to external preparations and UV radiation. Even indifferent creams and sunscreens can cause an increase in inflammatory manifestations. Most patients suffering from this type of rosacea do not have a history of acne vulgaris.
Forms
The classification of rosacea is still a subject of debate. Historically, it is believed that the disease is characterized by a staged course. However, the classification of the expert committee of the American National Rosacea Society from 2002 indicates the existence of 4 main types of rosacea (erythematous-telangiectatic type, papulopustular type, phymatous and ocular types, corresponding to the hypertrophic stage and ophthalrosacea in the domestic classification). It also questions the transformation of one type into another, with the exception of cases of rhinophyma development in patients with the papulopustular type of rosacea.
Papulopustular rosacea is characterized by a similar clinical picture, but with this type of rosacea there are not as many complaints about sensations from the erythema as with the erythematotelangiectatic type. Patients are mainly concerned about papular rashes. They are characterized by a bright red color and perifollicular location. Individual papules can be crowned with a small round pustule, but such papulopustular elements are few. Peeling is usually absent. Formation of persistent edema at the site of widespread erythema is possible, which is more common in men.
Phymatous, or hypertrophic, type of rosacea is characterized by significant tissue thickening and uneven bumpiness of the skin surface. The occurrence of such changes on the skin of the nose is called rhinophyma, metaphyma - if the skin of the forehead is affected; gnathophyma is a pineal change in the chin, otophyma - of the auricles (it can also be unilateral); much less often, the process affects the eyelids - blepharophyma. There are 4 histopathological variants of pineal formations: glandular, fibrous, fibroangiomatous and actinic.
The ocular type, or ophthalrosacea, is clinically predominantly represented by a combination of blepharitis and conjunctivitis. Recurrent chalazion and meibomitis often accompany the clinical picture. Conjunctival telangiectasias are often encountered. Patients' complaints are nonspecific, burning, itching, photophobia, and a foreign body sensation are often noted. Ophthalrosacea may be complicated by keratitis, scleritis, and iritis, but in practice such changes are rare. In rare cases, the development of eye symptoms precedes skin symptoms.
There are special forms of the disease: lupoid, steroid, conglobate, fulminant, gram-negative rosacea, rosacea with solid persistent edema (Morbigan's disease), etc.
In particular, lupoid rosacea (rosacea lupoides, granulomatous rosacea, Lewandowsky tuberculoid) is characterized by the formation of a granuloma like foreign bodies. A yellowish-brownish color of papules is noticeable during diascopy. A decisive role in diagnostics is played by histological examination of the characteristic element.
 [ 10 ]
[ 10 ]
Diagnostics rosacea
The diagnosis, according to the American Committee for the Study of Rosacea, is based on anamnestic data, indicating, first of all, the existence of persistent erythema of the central part of the face for at least 3 months. Complaints of burning and tingling in the area of such erythema, dry skin and the appearance of telangiectasias, the appearance of papules against the background of stagnant erythema, hypertrophy of the protruding parts of the face and the detection of eye damage allow us to determine the type of rosacea.
What do need to examine?
How to examine?
Differential diagnosis
In terms of differential diagnosis, it is necessary to first exclude true polycythemia, connective tissue diseases, carcinoid and mastocytosis. In addition, it is necessary to differentiate rosacea from periorificial or steroid dermatitis and contact dermatitis, including photodermatitis. Laboratory diagnostics are mainly carried out by excluding other diseases, since there are still no specific tests for verifying rosacea.
Who to contact?
Treatment rosacea
Today, the problem of treatment is much better developed than the pathogenesis and etiology of rosacea. Therapeutic tactics largely depend on the clinical type of the disease. However, the success of rosacea treatment is based on the joint efforts of the doctor and the patient to determine the provoking factors, which are strictly individual. Most often, these include meteorological factors: exposure to solar radiation, high and low temperatures, wind and associated abrasive effects; alimentary: consumption of hot and carbonated drinks, alcohol, spicy foods and excess food; neuroendocrine: emotional effects, climacteric syndrome and other endocrinopathies accompanied by increased blood circulation in the carotid artery pool; iatrogenic, including both systemic drugs that cause facial erythema (for example, nicotinic acid preparations, amiodarone), and external drugs, including cosmetics and detergents that have an irritating effect (waterproof cosmetics and toners, the removal of which requires the use of solvents, as well as detergents containing soap). Elimination or reduction of the effect of these factors significantly affects the course of the disease and reduces the costs of drug therapy.
The basis of treatment is adequate daily skin care. First of all, it includes sunscreens. They should be selected taking into account the increased sensitivity of the skin of patients with rosacea. The least irritating effect is possessed by indifferent preparations (titanium dioxide, zinc oxide), which block ultraviolet irradiation of the skin due to their physical properties. Preparations containing chemical ultraviolet filters, which can be recommended to patients with rosacea, should not contain sodium lauryl sulfate, menthol and camphor and, on the contrary, should contain silicones (dimethicone, cyclomethicone), which significantly reduce the irritating effect of sunscreens and ensure their water resistance and low comedogenicity.
The basis of the recommendations for daily skin care is the regular use of light-consistency, green-colored, fattening preparations for daily use. It is advisable to apply them in a thin layer 2 times a day and as a base for make-up, which is preferably presented in the form of powder or shaken mixture. It is necessary to remember that the restoration of barrier functions is a very important component of the therapy of rosacea, which is characterized by increased sensitivity of the skin.
Currently, topical treatment is considered preferable for all types of rosacea, with the exception of hypertrophic rosacea, for which surgical treatment and systemic synthetic retinoids are most effective. Numerous comparative studies conducted in independent centers in accordance with the principles of evidence-based medicine have demonstrated the absence of statistically reliable data on the superior efficacy of systemic treatment. For example, it has been shown that the efficacy of systemic tetracycline antibiotics does not depend on the dose and frequency of administration of the drug, and is apparently not associated with their antimicrobial action. The same applies to systemic use of metronidazole, although it can serve as an alternative to tetracycline antibiotics in cases where the latter are contraindicated. Assumptions about the effectiveness of metronidazole against Demodex spp., which survive in conditions of high concentrations of metronidazole, have proven unfounded. These drugs, however, continue to be widely used, but their use is not approved by such organizations as the Federal Drug and Food Administration (FDA) in the USA. For lupoid rosacea, systemic tetracyclines are prescribed; there are indications of the effectiveness of phthivazid.
The most effective is considered to be the combined use of external preparations of azelaic acid with external preparations of metronidazole or clindamycin. There are numerous publications on the effectiveness of tacrolimus or pimecrolimus. Sulfur-containing preparations and benzoyl peroxide remain relevant, although a possible irritating side effect of these drugs is noted. At the initial manifestations of the phymatous type of rosacea, monotherapy with isotretinoin in normal doses turned out to be the most effective. Whereas in the treatment of formed rhinophyma one cannot do without plastic surgery methods, which are often combined with various thermal effects. In this regard, modern photo- and laser therapy deserves special attention. Sources of incoherent intense light radiation (IPL), diode, KTR, alexandrite and, the most modern, long-pulse neodymium lasers on yttrium aluminum garnet (Nd; YAG lasers) are used. Laser treatment appears to be more effective and less expensive both in relation to telangiectasias (selective photothermolysis) and in relation to collagen reorganization due to thermal stimulation of fibroblasts, although the use of IPL sources is often better tolerated. In the treatment of hypertrophic rosacea, laser dermabrasion has recently taken one of the leading positions due to its safety.
Microcurrent therapy is widely used as a physiotherapeutic treatment. Its effectiveness is mainly associated with the redistribution of fluid in facial tissues and the restoration of lymphatic drainage. It is also noted that microcurrents effectively promote the restoration of the damaged skin barrier and prevent the dissociation of saprophytic microflora.
More information of the treatment

