Medical expert of the article
New publications
Facial demodecosis
Last reviewed: 05.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
The demodectic mite is a microscopic living organism that lives in the perifollicular zone and the sebaceous gland area on the body of almost the entire population of the Earth. Another issue is that with proper care of your body and organism, a person may never encounter this problem. But when certain negative factors converge, the mite becomes active, and the consequences of its activity begin to be observed visually. Mostly, in most cases, specialists diagnose demodicosis of the face. This disease is, in fact, both a medical and cosmetic problem.
Causes of facial demodicosis
The catalyst for the problem under consideration can be several different factors, therefore, in order to prevent the occurrence of the disease or to help a speedy recovery, it is necessary to know the causes of facial demodicosis, and having analyzed your lifestyle, try to eliminate possible sources of its provocation. Even if the infection has passed, and the doctor has prescribed a course of treatment, then following the recommendations with parallel relief of the original source, if this is of course possible, will allow you to quickly stop the problem and save yourself from subsequent relapses.
Doctors consider the following to be risk factors for the development of the disease:
- Decreased immune status of the patient. With high immunity, the parasite is unable to overcome the basement membrane.
- Diseases affecting the digestive organs and endocrine system of the patient.
- Staying in a closed, dusty and gas-polluted room for a long time: working in a paint shop, galvanizing, construction work, and so on.
- Increased use of decorative cosmetics in everyday or professional life. Such negative consequences can especially occur when using a low-quality cosmetic product, or if the cosmetics contain various bioadditives (hormonal substances) that are intolerable to the skin, as well as in the case when beauty products are expired.
- Old age of the patient.
- Stressful situations.
- Various phobias.
- Diseases affecting the human nervous system: neuroses, psychoses, excessive emotional exhaustion.
- An incorrect, unbalanced diet can also provoke the parasite to act:
- "Love" for fatty foods.
- An abundance of hot spices.
- Strongly or weakly carbonated drinks.
- Various marinades.
- Addiction to fast food products.
- Poor diet of vegetables and fruits.
- Excessive passion for sweets.
- Disruptions in the functioning of the sebaceous glands.
- Dermatological diseases.
- Unfavorable living conditions.
- The presence of bad habits: nicotine, drugs, alcohol.
- Not enough time spent outdoors.
- Pathological liver lesions.
- Biological disturbance of sebum components.
- Increased addiction to baths, saunas, and sun exposure.
- Love of tanning and spending long periods of time in the open sun.
- Taking hormonal medications.
- Scratching and trauma to the epidermis.
- There are known cases when the diagnosis is established, but the source of the pathology is not explained by any of the reasons given earlier.
The effectiveness of eliminating the disease will largely depend on determining the primary source. If you eliminate only the consequences of the pathology, the disease will return again and again. According to research, the risk group for this disease includes the weak half of humanity aged 30 to 50 years.
The male population of the planet is much less susceptible to the disease in question. Doctors explain this phenomenon simply: when shaving, along with the hair, a micron layer of the skin is scraped off, where the insect mainly lives.
Demodecosis is a superficial pathology that does not penetrate deep into the body. But its course and consequences significantly change a person's appearance, making their skin, and therefore their entire appearance, unattractive.
 [ 4 ]
[ 4 ]
Demodecosis of the facial skin
Human life is multifaceted and a situation may occur that awakens this insect. The tick begins to penetrate deeper into the skin layers, causing an inflammatory reaction of the epidermis. It is the inflammatory process, with many local foci, that doctors call demodicosis of the facial skin. This disease brings discomfort to its owner. In this case, a person receives both physical and emotional suffering.
This insect has a fairly high survival threshold, managing not to lose its physiological characteristics in vegetable oil, glycerin, cosmetic ointments and creams.
But the primary surge of parasite activity is not as dangerous as the secondary infection of the skin, as well as the consequences of disruption of the structure of the epidermis: the formation of colloidal scars and “pits”.
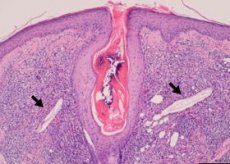
The causative agent of this disease in humans is the mite Demodex folliculorum, which was identified and described by doctors back in 1842. Modern medicine knows 65 types of this insect, but only three of them are capable of affecting human skin, causing the corresponding diseases.
Their "favorite" place of deployment is mainly the nose and chin of the human face. At the same time, it most often parasitizes near the sebaceous glands and hair follicles, but is quite capable of settling on eyelashes and eyebrows.
The parasite's size parameters are quite modest (0.4 mm), it is almost impossible to see it with the naked eye. The parasite's body is covered with small scales, with the help of which it attaches itself to the human body. The tick feeds on sebum, which is produced by glands, as well as hormonal substances of the human body.
As the researchers have established, ticks cannot stand daylight, so they become active closer to dusk, which causes the patient many unpleasant hours, as the itching intensifies.
The tick's life span is short, only a few weeks, but during this short period the female parasite manages to give birth several times, producing several dozen new parasites. And so reproduction occurs in geometric progression. Against the background of "young individuals", old ticks die. Dissolution occurs in the hair follicle, which provokes the development of the inflammatory process.
Symptoms of facial demodicosis
The progression of the pathology begins to manifest itself in unpleasant cosmetic defects. Symptoms of facial demodicosis include:
- Acne and red, inflamed pimples.
- Small ulcers and pustules may appear, gradually increasing in size.
- Intensive work of the sebaceous glands, areas affected by the pathological process become more shiny and oily.
- The skin of the face takes on a painful grayish-earthy or purple-red hue.
- Itching appears, which gradually increases in intensity.
- The texture of the epidermis becomes bumpy.
- The eyelids are swelling.
- The nose may become slightly puffy and swollen, changing color to an unnatural burgundy, or even red-blue.
- There is a contraction and inhibition of facial expressions.
- If the localization of the lesion affects the scalp, and adequate measures are not taken in a timely manner, hair and eyelashes begin to fall out.
- Hyperemic spots appear.
- Visual expansion of the pores of the epidermis is observed.
- A coating can be seen on the tips of the eyelids.
- Eyes become more tired by the end of the day.
- The peak of insect activity is recorded in the spring-autumn period of the year. It is at this time that a surge in relapses is also observed.
- The progression of inflammation can provoke the development of concomitant pathologies, such as conjunctivitis (inflammation of the conjunctiva) or blepharitis (often chronic bilateral inflammation of the eyelids).
In order to take the necessary measures in such a situation, you should first make sure that the diagnosis is correct by consulting a qualified specialist who will confirm or refute it, as well as give the necessary recommendations for eliminating the problem. After all, the symptoms of the lesion in question are quite similar to other dermatological diseases, such as trivial acne or rosacea.
Diagnosis of facial demodicosis
It may sound strange, but an ophthalmologist (oculist) conducts examination and diagnosis of the disease. But it would not be a mistake to consult a dermatologist. Diagnosis of facial demodicosis is quite simple and can be carried out even in the presence of the patient. The diagnosis method does not require additional complex medical equipment.
If the doctor suspects the patient has the disease in question, one or more cilia are taken for examination. As noted above, the insect's parameters do not allow it to be distinguished with the naked eye, but a standard laboratory microscope is sufficient.
A "live" eyelash that has just been removed is suitable for the study. It is placed between slides and fixed on the laboratory table of the magnifying device. For a high-quality study, a solution of 10-20% alkali, or glycerin, kerosene, gasoline is applied to the slide with the eyelash, after which it is covered with a second slide.
After this, the eyelash is examined under a microscope for the presence of pathogenic insects.
Consultations with other specialized specialists are also practiced: surgeon, endocrinologist, neuropathologist.
 [ 7 ]
[ 7 ]
Facial cleansing for demodicosis
Cosmetic body care is positive in any case. It has its own healing effect and on the process of the fastest recovery of the skin in the considered disorder. Facial cleansing for demodicosis is carried out twice a day. In this case, the procedure should be performed only by a qualified cosmetologist. Self-cleaning or a procedure performed by an amateur can only worsen the clinical picture. An unprofessional person can aggravate the situation by spreading the infection throughout the entire area of the treated area.
The procedure itself is aimed at cleansing the skin, removing the parasite's waste, excess sebum and sweat gland products. This procedure mainly uses PH neutral chemical compounds that do not have soapy properties.
A little less often, but a person with such a pathology can be found on a deep facial peeling. Such cleaning is carried out with special medicinal scrubs, enzymes or special chemicals. The procedure should be carried out only on the basis of a beauty salon.
To moisturize the epidermis layer, cosmetologists use hyaluronic acid or urea-based medications.
When treating the disease, alginate masks are used, which are based on alginic acid, without other additional additives. This procedure should only be carried out within the walls of a beauty salon.
It is also possible to undergo other physiotherapeutic procedures:
- Cryomassage is a procedure using cold.
- Ozone therapy is a modern physiotherapeutic method of treatment, which is carried out through the use of an ozone-oxygen mixture.
- Mesotherapy is a subcutaneous or less deep intradermal injection of active components of medicinal preparations and vitamin complexes.
During the treatment period, it is necessary to refrain from using cosmetics: foundation, powder, eyeshadow, etc. Since this is an excellent breeding ground for the development of the subcutaneous mite. And after the end of the therapy, it will be necessary to get rid of all cosmetics, replacing them with new ones, since old ones contain demodex larvae, which is a source of the return of the disease.
You should not squeeze out inflamed pimples on your own during the treatment, such a desire to quickly get rid of the problem will only prolong the course of therapy. You should not smoke and avoid smoky rooms.
 [ 8 ]
[ 8 ]
Treatment of demodicosis of facial skin
A person who faces this problem faces a dilemma of how to get rid of discomfort, but you should not engage in self-diagnosis and treatment. First, you should make an appointment with an ophthalmologist. Only a specialist can correctly determine the disease, find the source of the pathology and prescribe adequate effective treatment for demodicosis of the facial skin.
One of the points of therapy is drug treatment of the disease.
- The treatment protocol includes drugs that increase the patient’s immune status: Immunal, Thymogen, Viferon, Lokferon, Bronchomunal and others.
The medicine that stimulates the immune process, Immunal, is prescribed by a doctor, both in the form of tablets and solution.
Adult patients are administered 20 drops three times a day, having previously diluted it in a small amount of water. If clinically necessary, the amount of the administered drug can be increased to 40 drops, but after the acuteness of the disease has been relieved, the dosage is reduced to 20 drops and taken with the recommended frequency.
For young patients, the dosage of the drug varies depending on age:
- from one to six years - 5-10 drops three times a day.
- from six to 12 years old - 10-15 drops three times a day.
The duration of treatment is from one week to eight.
This drug is contraindicated if the patient has a history of tuberculosis, multiple sclerosis, leukemia, or allergic reactions to the components of the drug.
- Medicines that normalize the functioning of the gastrointestinal tract are also prescribed: polyphepan, bimeral, hilak forte, laktonorm, degistal forte, trimedat and others.
The probiotic Hilak Forte is administered to the patient with food or before meals. Before taking the drug, dilute it with a sufficient amount of liquid (except milk).
The medicine is taken three times a day in the following dosage:
- - Adult patients and adolescents over 12 years old - 40-60 drops. - Children from two to 12 years old - 20-40 drops of the drug. - Babies from birth to two years old - 15-30 drops.
If the condition has stabilized somewhat, the dosage should be halved. Contraindication to the use of the drug is individual intolerance to the components of Hilak Forte.
- Antiparasitic drugs: tinidazole, bacimex, trichosept, metronidazole, metroxan, trichopolum, metroseptol and others.
Metronidazole is taken orally immediately with or after food. The tablet is not chewed. Adult patients and adolescents who have already reached the age of 12 are prescribed the drug in a dosage of 0.25 - 0.5 g three times a day for seven to ten days. Children from two to 12 - 7.5 mg per kilogram of the small patient's weight, divided into three daily doses.
The maximum daily dose for adults is 4 g.
Factors that do not allow taking this medicine include increased individual sensitivity to the components of the medicine, as well as if the patient's medical history includes leukopenia, a tendency to epilepsy, severe liver failure, nitroimidazole, the first trimester of pregnancy, lactation, age under 2 years.
- Antiseptic ointments for demodicosis: ichthyol, yellow mercury, sulfur.
The ointment is used only externally in a thin layer. The lubricated area is covered with gauze. The procedure is repeated two to three times throughout the day.
A contraindication to the use of this ointment is individual intolerance to the components of the drug.
- Antiparasitic drug permethrin, aversect.
The ointment is applied to the affected area two to three times a day. The duration of treatment is up to five weeks.
- Cream-gel "Dexodem Phyto" - therapy for demodicosis of the eyelids.
Before applying the drug, the skin of the face should first be washed well, after which the drug should be applied in a thin layer. During the treatment, it is necessary to use only disposable towels to prevent re-infection. The procedure is carried out twice a day (morning and evening). The only thing to clarify is that the duration of treatment is at least one and a half months.
Sequence of procedure:
- We apply a cotton or gauze swab soaked in any alcohol tincture to the tightly closed eyelid. The procedure is repeated after a quarter of an hour. This method allows for more effective removal of the parasite's waste products. The procedure should be carried out carefully so that the liquid does not get into the eyes.
- Only after such treatment can the medicinal cream-gel be applied. The eyes are again tightly closed and the medicine is applied with a cotton swab.
- In case of deep damage to the epidermis, a dermatologist or dermatocosmetologist can prescribe a special essential oil, which is ordered and prepared in specialized pharmacies. Even short-term use of the medicine is enough to get rid of the mite.
Other methods used in the treatment of facial demodicosis are:
- Electrophoresis is a physiotherapeutic treatment method, the essence of which is the introduction of a medicinal substance into the body using a weak electric current. Shows good therapeutic results.
- Microdermabrasion is a mechanical peeling or micro-grinding of the skin, which involves removing the upper microlayer of the skin, in which the demodectic mite mainly settles.
- The laser coagulation technique is similar to the previous one, only the grinding is done using a laser.
- The attending physician's attention must be drawn to adjusting the diet and introducing a corrective diet.
Face masks for demodicosis
There are numerous folk remedies, the use of which allows you to get rid of the problem in question, using face masks for demodicosis.
- The parasite in question does not tolerate an acidic environment, which blocks its access to nutrition. Therefore, almost all fruit and berry masks that have natural acid are effective in combating this insect. It should only be taken into account that if the patient's skin is oily, then no additional additives are required, and if it is dry, then it is necessary to add egg yolk to the fruit pulp to prevent severe drying of the skin.
- To soothe skin irritation, you can use compresses made from gauze soaked in decoctions of medicinal herbs: sage, chamomile, succession, oak bark, calendula and others.
- You can use a mask made from two parts sour apple and one part horseradish. Grind the ingredients and apply to cleansed skin. Leave it on for about 15 minutes. If it stings too much, you can remove it earlier than expected. After the cleansing procedure, wipe your face with whey and apply a disinfectant on top - Lassar paste.
But home masks should not be the only way to treat the disease; you should definitely consult a dermatologist who will prescribe the main treatment.
- Clay masks are also used to treat the disease. Take one tablespoon of medicinal blue clay and dilute it with a small amount of clean water until it becomes a paste. You can also add a teaspoon of 5% natural apple cider vinegar. Mix everything thoroughly.
The substance is applied in a thin layer to the face, without touching the lips and eyes. Keep the mask on for 15-20 minutes, then wash off with warm water. During the procedure, the clay on the face will dry out, so it is advisable not to talk or use facial expressions during this period.
Instead of vinegar, you can add a teaspoon of hydrogen peroxide or three to five drops of iodine to the clay. The procedure is carried out in the same way as described above.
Yellow clay works in a similar way.
- You can try using another composition: take equal proportions of olive oil and crushed garlic. Apply the "medicine" to the damaged areas. It is better to carry out the procedure lying down. Cover with cling film on top. Leave for 25 to 40 minutes and rinse with warm water. Apply a moisturizer on top. If it is difficult to carry out the procedure yourself, you should ask for help.
An ointment prepared on the basis of a small amount of Vaseline and a couple of crushed Trichopolum tablets shows high efficiency. This composition is carefully applied to the affected eyelids (the lower and upper eyelids are treated). The ointment is collected on a stick and applied to the skin. It is necessary to ensure that the composition does not get into the eyes.
- Laundry soap (tar soap is best) can also be used as a base for a medicinal mask. Grate it and mix it in a small amount of water. Additional substances can be: a teaspoon of apple cider vinegar, vegetable oil or hydrogen peroxide, three to four drops of iodine. The solution is applied only to the affected areas when the patient is lying down. A polyethylene film is placed on top of the “medicine”. After the procedure, the composition is washed off with warm water.
- A napkin soaked in tomato juice can serve as a compress. Such procedures are carried out up to twenty times a day, 15 minutes each.
- Aloe juice diluted 1:1 with water is also effective. Soak gauze in the liquid and apply to the face for a quarter of an hour. The mask should be done daily. The course of treatment is 25 procedures.
Nutrition for facial demodicosis
Nutrition plays an important role in therapy for facial demodicosis. A properly composed regimen of introducing healthy foods can significantly reduce the parasite's ability to reproduce and continue its life.
After diagnosing the disease, the patient should exclude from his diet:
- Smoked and fatty foods.
- Sweets and any foods with a high glucose content.
- Hot spices.
- Minimize salt intake.
- It is necessary to ensure that as little glucose as possible, which is food for the parasite, ends up on the patient’s table.
These products can irritate the mucous membrane of the digestive organs, which only activates the inflammatory process.
The basis of the menu should consist of the following food products:
- A variety of vegetables. Fiber will help cleanse the gastrointestinal tract of food debris.
- Fruits that have a sour taste.
- Fermented milk products: kefir, ayran, cottage cheese, curdled milk, fermented baked milk, yogurt.
- Cereals: whole grain bread and various porridges: millet, buckwheat, pearl barley, oatmeal.
- It is necessary to increase the amount of liquid you drink per day: juices, milk, teas, compotes, mineral water.
This diet helps cleanse the body of toxins and harmful substances, which makes it possible to stimulate the patient's immune system, forcing his body to strengthen the resistance to the invasion. Such nutrition brings an imbalance to the vital activity of the demodectic insect. Without receiving sufficient nutrition, the subcutaneous mite dies, which leads to a speedy recovery.
Diet for facial demodicosis
Diet for facial demodicosis plays not the last, but perhaps even one of the leading roles in the therapeutic treatment of the disease in question. Doctors have long established that improper nutrition, the predominance of certain foods in the diet, are one of the factors that can become a catalyst in the process of awakening and rapid reproduction of the subcutaneous mite.
Those people who have already had to deal with the pathology in question are well aware of the value of the diet and the restrictions it imposes on the patient's diet. Dietary nutrition makes it possible to improve digestion and cleanse the body, which invariably affects the growth of defenses and the body's ability to fight invasive lesions.
During treatment, you should avoid eating the following foods:
- Smoked and fried dishes.
- Those that contain large amounts of sugar and salt.
- Chocolate.
- Sour cream, hard cheeses, rennet cheeses.
- Products that contain large amounts of animal fats.
- Low and high alcoholic drinks.
- Brewer's and confectioner's yeast.
- Soy sauce.
- Citrus fruits: pomelo, tangerines, oranges, grapefruit, sweeties, lemons and other similar fruits are strong allergens.
- Vegetables: eggplants, tomatoes, avocado.
- A range of legumes, including pulses.
- Fruits include sweet fruits: bananas, figs, grapes, melon, apricot, red plums, raisins.
- Eliminate highly spicy foods from your diet.
- Avoid eating very hot foods.
- Honey and bee products.
Products that must be present in the patient’s diet:
- It is necessary to increase the amount of consumed vegetables (white potatoes, cabbage, carrots) and sour fruits. These products are rich in plant fiber, which helps to normalize digestion and cleanse the body.
- You should increase the amount of liquid you consume: soups, soft drinks, fresh juices, compotes, juices.
- Whole grain bread.
- Nuts: almonds, peanuts.
- Decaffeinated drinks.
- All kinds of greenery.
- Dairy-free cheeses.
- Cereal porridges: oatmeal, buckwheat, millet, pearl barley, rice.
- Fermented milk products and milk.
The approach to solving the problem that has arisen should be comprehensive and, along with medication, physiotherapy and cosmetic treatment, the patient should receive a complete, but dietary diet, rich in plant fiber, micro- and macroelements, vitamins, so necessary for the body to function normally. It is adherence to all dietary recommendations that allows you to speed up recovery and reduce the risk of re-infection to a minimum. Against the background of such a diet, the general condition of the human body also improves, which is important for maintaining physical and emotional health.
 [ 9 ]
[ 9 ]
More information of the treatment
Prevention of facial demodicosis
In order to avoid suffering with treatment and not to experience a lot of unpleasant minutes in front of the mirror, it is necessary to prevent demodicosis of the face. To reduce the risk of activation of the parasite, you should follow a number of simple recommendations.
- The cosmetics that a woman uses must be of high quality, not expired, and not contain hormonal substances.
- Avoid going to the bathhouse, sauna or solarium. Limit your time under the scorching rays of the summer sun.
- Avoid dusty, gas-polluted areas.
- Grooming and cleaning pets.
- If there was a precedent, get rid of cosmetics and things infested with ticks.
- Monitor the immune status of the body, maintaining it at a high level.
- Lead a healthy lifestyle, eliminating smoking (even passive smoking), alcohol, and drugs.
- Balance your diet.
- After washing, bed linen should be ironed on both sides.
- Wash and clean items regularly, especially if the disease has been diagnosed and the patient is undergoing treatment.
- Periodically disinfect glasses and shaving accessories.
- Do not ignore morning and evening washing.
- If there is a patient with facial demodicosis in the family, limit his close contact with other residents of the apartment. Provide him with individual dishes, bed linen and personal hygiene products.
- Avoid overheating or overcooling of the skin.
- Avoid stressful situations and excessive emotional exhaustion.
- Avoid physical overexertion by alternating heavy loads with rest.
- Carefully monitor your skin, and at the slightest deviation from the norm, consult a dermatologist or ophthalmologist.
By following these recommendations, a person can avoid or significantly reduce the risk of developing the disease.
Prognosis of facial demodicosis
If a person has a fairly high immunity, and his medical history is not burdened with a “bouquet” of serious diseases, then the prognosis for facial demodicosis is favorable; it is enough to sit on a diet for three months.
Depending on the type of skin, remission can be observed from three years to a year, and in some cases even more. After completing the treatment course, every tenth patient experiences relapses. In most cases, the return of the disease is associated with untimely treatment by a specialist, neglect of the disease, incompleteness of treatment therapy, that is, the patient simply did not cure the disease.
Demodecosis of the face is not a lifelong verdict, unless of course you ignore this fact and promptly seek advice and help from a qualified doctor. Self-medication can significantly worsen the situation, only a specialist can make a correct diagnosis and give the necessary recommendations. But a lot also depends on the patient. By leading a healthy lifestyle and adhering to a balanced diet, a person can significantly protect himself from the activation of the demodectic mite. Dietary nutrition will not only prevent the disease or speed up the recovery process, but will also significantly improve the health of the entire body as a whole.

