Medical expert of the article
New publications
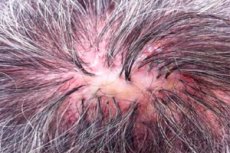
Kanko's decalving folliculitis as a cause of alopecia areata
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Folliculitis decalvans (synonym: sycosiform atrophic folliculitis of the head (folliculitis sycosiformis atrophicans capitis, Hoffmann E. 1931) was first described by Quinquaud (Quinquaud Ch.E. 1889). This very rare dermatosis is a chronic bacterial folliculitis of the scalp, which ends in atrophic alopecia (pseudopelade condition; decalvo (lat.) - to make bald); other areas of the skin can also be affected, especially those covered with bristly and long hair. A similar process on the face, in the area of beard growth, described in the same years, received other names: lupoid sycosis (sycosis lupoides, Brocq L., 1888); cicatricial sycosiform erythema (ulerythema sycosiforme, Unna P., 1889; ovkr (Greek) = ule (Latin) = scar); sycosiform atrophic folliculitis (folliculitis sycosiforme atrophicans barbae, Hoffmann E., 1931).
Thus, different scientists gave different names to the same dermatosis, in which the main, from their point of view, characteristic features were highlighted: chronic folliculitis, similar in course and outcome to discoid lupus erythematosus (atrophy); erythema with sycosiform manifestations and scarring; chronic folliculitis, similar to sycosis, but leading to atrophy. Already in the first descriptions of decalvans folliculitis and lupoid sycosis, common features for both dermatoses were revealed, determining their clinical manifestations: chronic folliculitis, leading without pustulation and ulceration to atrophy and persistent baldness, high resistance to therapy. The differences are in the distribution of chronic folliculitis (folliculitis grouped into small foci - in comparison with the formed large individual foci) and their predominant location (on the scalp or facial skin). Later it turned out that in addition to the facial skin, lupoid sycosis (LS) can also affect the scalp, as well as the skin of the pubic and axillary areas. Only many years later it became finally clear that the lupoid sycosis described by Brok is not an independent nosological form, but duplicates the same disease - decalvans folliculitis is a unique and rare clinical variant.
Causes of folliculitis decalvans
The causative agent is considered to be Staphylococcus aureus, additionally colonization of hair follicles by gram-negative microflora is also possible. However, treatment with broad-spectrum antibiotics gives only a temporary therapeutic effect, strictly limited by the duration of the course. This confirms the dominant role of the macroorganism, changes in its reactivity and a decrease in immune protection.
Pathogenesis
Seborrheic condition, decreased resistance caused by diabetes mellitus, chronic nephritis, dysproteinemia, and other factors leading to suppression of the immune system may predispose to this dermatosis. Cases of spontaneous healing of decalvans folliculitis (DF) after removal of carious teeth complicated by periodontitis have been described. Colonization of hair follicles by bacteria is most likely only a pathogenetic link. The reason why chronic folliculitis ends with skin atrophy and persistent baldness remains unclear. In patients with decalvans folliculitis, or lupoid sycosis, modern research methods always manage to detect specific and significant disorders in the function of the immune system, internal organs, and other body systems.
Symptoms of Kenco's folliculitis decalvans
Folliculitis decalvans usually occurs isolated on the scalp, mainly in the temporal and parietal areas, the frontal area lesions are located on the border of hair growth and resemble ophiasis. In some cases, the axillary and pubic areas are also affected. Eruptions of inflammatory follicular nodules, less often pustules, usually do not cause subjective sensations and are therefore often visible. The size of the rash elements varies from a pinhead to a lentil. In the center, papular and pustular elements are penetrated by unchanged or broken hair, and a small crown of hyperemia is visible in their circumference. Folliculitis is characterized by extremely slow development; they exist for a long time without noticeable dynamics and often do not end with the formation of a pustule. Individual follicular pustules appear only after a long evolution of follicular papules ("secondary pustule" according to Mashkilleyson L.N., 1931). In the center of small grouped foci, a gentle cicatricial atrophy with persistent baldness gradually forms. When several adjacent foci merge, larger foci of cicatricial alopecia are formed, within which individual hairs are sometimes preserved. In the border zone, new follicular nodules and pustules, scales, crusts continue to appear, causing slow peripheral growth. Thus, decalvans folliculitis leads to the formation of foci of atrophic baldness of different sizes and shapes (pseudopelade condition). The course of the dermatosis is chronic, lasting for many years and even decades. At times, the number of new folliculitis appearing in the circumference of foci of atrophic baldness is reduced to a minimum. Decalvans folliculitis of the scalp can be combined with foci of lupoid sycosis (LS) on the skin of the face or other localizations.
Lupoid sycosis mainly affects middle-aged and elderly men. The usual localization of one or two foci of LS are the lateral surfaces of the hairy cheeks, temples, less often - the chin and upper lip (Milman I.S., 1929). The lesion is most often unilateral and is located in the area of hair growth in the temporal region or on the cheek above the horizontal and ascending branches of the lower jaw. A lesion of LS can occur in isolation as a large single lesion and on the scalp. Initially, against the background of hyperemia, grouped inflammatory follicular nodules and pustules appear in the same area, as well as small follicularly located light yellow crusts and grayish scales, which are easily removed by scraping. These elements merge and form a clearly defined round or oval inflammatory plaque with a diameter of 2-3 cm or more, wine-red in color (as in erysipeloid) with a flat painless infiltrate at the base. Gradually, in its central part, the skin turns pale, thins, becomes smooth, devoid of hair and slightly sunken: a characteristic feature of the formed focus of lupoid sycosis develops - central atrophy. Within its limits, new rashes no longer appear and single hairs or tufts of hair growing from one or several follicles may still remain. The peripheral zone of the focus, about 1 cm wide, is slightly elevated, more saturated with red color and moderately infiltrated. Numerous follicular papules with rare follicular pustules are located in it, some of which are perceived as bubbles. In the center of these elements there are still preserved hairs, some of which are broken off, as well as a significant number of easily removable follicularly located crusts and scales. The lesion slowly increases in size due to the appearance of new folliculitis and individual follicular pustules in the peripheral zone. Sometimes the growth of the lesion prevails in one of its foci, which changes the round outlines. When diascopying the edge of the lesion, the "apple jelly" symptom is not determined. LS proceeds chronically for many months and years. Clinical manifestations of lupoid sycosis of the scalp are smoother. In the formed lesion, a smooth, hairless atrophic zone dominates. In the peripheral hour, the elevated ridge is absent, there are only individual, long-standing folliculitis and pustules surrounded by a narrow rim of hyperemia, as well as isolated small scales and crusts. Thus, on the scalp, the manifestations of lupoid sycosis and decalvans folliculitis are practically indistinguishable. The general condition of patients is not disturbed, subjective sensations are usually absent, complaints are limited to a cosmetic defect.
Histopathology
In the epidermis there is a small focal hyperkeratosis, frayed horny masses, pronounced acanthosis. The cells of the spinous layer are sharply changed, especially in the lower rows, where there are signs of pronounced vacuolar dystrophy. The openings of the hair follicles are significantly expanded, filled with horny masses. In the dermis there is a dense perivascular and perifollicular lymphohistiocytic infiltrate, less common plasma mast cells and neutrophils. In some cases, the infiltrate almost entirely consists of plasma cells. In the final atrophic stage, the pathomorphological picture differs little from the changes characteristic of the pseudopelade state in the late stage.
Diagnosis of Kenco's decalvans folliculitis
On the scalp, manifestations of decalvans folliculitis or lupoid sycosis are differentiated primarily from those diseases that manifest as chronic folliculitis and follicular pustules and lead to a pseudopelade state. Therefore, when atrophy of DF (or LS) has not formed in the central part of the lesion, it is differentiated from mycosis of the scalp, including the scutular form of favus, vulgar sycosis, and later - with necrotic acne, folliculitis and perifolliculitis abscessing and undermining the head of Hoffmann, histiocytosis from Langerhans cells and erosive pustular dermatosis. Since follicular papules and tubercles on the scalp can resemble chronic folliculitis and pustules. It is also differentiated from follicular lichen planus, lupus erythematosus, lupus tuberculosis, lupoid leishmaniasis and tubercular syphilid. Histological examination of typical rash elements (folliculitis, pustules, etc.) from the active peripheral zone of the lesion provides significant assistance in establishing the final diagnosis.
Differential diagnostics with mycosis of the scalp. The reason for mycological examination is the presence of flaking, altered hair, yellow crusty scales, follicular pustules, inflammatory follicular nodules and knots, purulent-bloody crusts with hair fragments and foci of cicatricial alopecia of varying sizes on the scalp. In the presence of these manifestations, especially in children and elderly patients, it is advisable to exclude mycosis of the scalp. When examining other areas of the skin, pay attention to the condition of the nail plates of the hands and feet. It is necessary to conduct a fluorescent study of hair, microscopic and cultural study of altered hair, skin and nail scales, crusts, purulent discharge. The fastest and most informative is a microscopic examination of the altered hair (broken at the skin level, having the appearance of "black dots", and at a height of 3-5 mm, with a cap at the base, gray, dull, deformed in the form of "spots", "exclamation marks"). Detection of fungal elements, clarification of the characteristics of the hair lesion by it allow the doctor to diagnose mycosis of the scalp and get an idea of the genus of the pathogen and the probable epidemiology of the disease.
Lupoid sycosis (LS, or DF) differs from vulgar sycosis by the dominance of long-term folliculitis, only a small part of which ends with the formation of follicular pustules, the presence of 1 or 2 (with DF - more) clearly defined foci with slow peripheral growth and the existence of 2 zones in them (except for foci on the scalp): a central, wide zone of cicatricial atrophy, and a peripheral - narrow, serpiginizing in the form of a red ridge, where new folliculitis is formed. The characteristic localization of LS is also different - the temporal region and the lateral surface of the cheek, the scalp and much less often - the chin and upper lip, which are favorite for vulgar sycosis. It is also necessary to take into account the greater resistance of DS (or DF) to treatment, compared to vulgar sycosis, as well as the differences in the pathomorphological picture. The active peripheral zone of the scalp in DF (or DS), which is important for clinical and histological diagnostics, is weakly expressed and is represented only by individual folliculitis and follicular pustules. In this way, decalvans folliculitis, or lupoid sycosis, differs from many other dermatoses of the scalp, leading to a pseudopelade state.
Decalvans folliculitis (or lupoid sycosis) of the scalp should be differentiated from necrotic acne (NA), or necrotic folliculitis of this localization. With a common primary eruption element (folliculitis) and chronic course of these rare dermatoses, they differ in the localization and distribution of folliculitis, as well as in the rate and features of their evolution. For DF, or LS, in contrast to necrotic acne, long-existing follicular papules with a diameter of 2-5 mm are characteristic, which slowly transform into single pustules without central necrosis and dirty-brown necrotic crusts. In DF or LS, chronic folliculitis is grouped, grows peripherally and merges without pustulization, central necrosis and itching, leading to the formation of smooth foci of atrophic alopecia (pseudopelade condition). In NU, for example, the favorite localization is the skin of the forehead along the border of hair growth (an area several centimeters wide outside and inside the hairline), temporal areas, the back of the neck, rarely the rash can spread to the ears, nose, central areas of the chest and back. In necrotic acne, folliculitis occurs in older people usually against the background of seborrheic status, is accompanied by itching and quickly transforms into papulopustular, then into papulonecrotic elements. They are always isolated, delimited from each other, do not grow peripherally and therefore do not merge into larger foci. In NU, purple-red follicular papules and papulopustules 2-4 mm in diameter quickly become necrotic in the center and are covered with dirty-brown necrotic crusts. They are tightly attached, persist for a long time, therefore they dominate in clinical manifestations and are most characteristic of necrotic acne, or necrotic folliculitis. After the crusts come off, isolated stamped, smallpox-like scars remain on the skin, which resemble scars after papulonecrotic tuberculosis or grouped tubercular syphilid. On the scalp, scars after NU are barely noticeable and do not lead to the formation of quickly detectable foci of cicatricial atrophy. Histological changes in these dermatoses also differ. A peculiarity of the histological picture in necrotic acne is the location of a granulocytic abscess with necrosis of the epithelium of the funnel of the hair follicle inside the follicle. The perifollicular infiltrate consists of neutrophils, lymphocytes and mast cells; there are vascular thromboses in the peripheral inflammatory zone.
Initial manifestations of folliculitis and perifolliculitis abscessing and undermining Hoffmann (FPAP) of the scalp may resemble decalvans folliculitis (DF, or lupoid sycosis). However, with formed clinical manifestations, these dermatoses have little similarity, which is limited only to chronic inflammation of the hair follicle and a long persistent course, leading to cicatricial alopecia. The depth of the lesion, inflammatory changes in the area of the hair follicle, the main rash element and its evolution are different. With DF (or LS), superficial chronic folliculitis of the scalp is grouped and merges into foci without pustulization, without the formation of subcutaneous abscessing nodes and without the formation of fistulous openings with purulent-bloody discharge and crusts. In the central, largest area of the lesion, a smooth, shiny, thin atrophic scar (pseudopelade condition) is formed. In the marginal zone of the lesion, follicular papules with single pustules and a rim of hyperemia in their circumference, as well as easily detached scales and crusts dominate. In FPAP, in contrast to DF (or LS), the dominant rash element is deep nodes with a diameter of 0.5 to 1.5 cm, which merge, abscess and perforate tissues. They arise as a result of the evolution of deep abscessing and undermining folliculitis and perifolliculitis. When nodes abscess, numerous subcutaneous fistulous tracts are formed, which seem to undermine the skin and open on the surface with numerous openings. When pressing on the infiltrated area with a bumpy surface, purulent and bloody discharge is released simultaneously from several fistulous openings spaced apart from each other, which is considered characteristic of this rare dermatosis. It is noteworthy that the deeply (to the tendon helmet) penetrating lesion is not accompanied by pronounced hyperemia of the scalp and remains slightly painful. FPAP occurs only in men aged 20-30 years with pronounced seborrheic status. In some cases, this dermatosis is combined with spherical and inverse acne. After scarring of individual FPAP foci, not only atrophic baldness remains, but also hypertrophic, uneven scars, especially in the occipital region.
In some cases, Langerhans cell histiocytosis of the scalp is clinically very similar to the manifestations of devaluing folliculitis, or lupoid sycosis, of this localization. These diseases are chronic, steadily progressing and leading to a pseudopelade state, within which the characteristic manifestations of the previous dermatosis are not preserved. In some patients, the lesion of the scalp by histiocytosis is isolated, but more often it is a fragment of systemic changes caused by the proliferation of Langerhans cells in the skin and visible mucous membranes or the proliferation of macrophages in other tissues (in bones, the central nervous system, in the liver, intraorbitally, etc.). In these cases, in addition to the common manifestations of histiocytosis on the skin (they may also resemble manifestations of other dermatoses: Darier's disease, decalvans folliculitis, necrotic acne, etc.), there are other characteristic manifestations of this very rare disease. Thus, the most common are lung lesions, foci of destruction in the bones (especially the skull), damage to the posterior pituitary gland (which manifests itself as symptoms of diabetes insipidus), exophthalmos caused by retrobulbar infiltration of fatty tissue, damage to the oral mucosa (infiltration and swelling of the gums, ulcers, loosening and loss of teeth). In some cases, the clinical manifestations of DF and histiocytosis of the scalp are very similar.
With great similarity of clinical manifestations of these dermatoses on the scalp, it is possible to distinguish individual symptoms that are not characteristic of DF. The most significant difference is the presence of papulopustular and pustular elements in the active zone of scalp skin histiocytosis that are not associated with hair follicles, as well as individual superficial erosions and ulcers of an elongated shape that are revealed after the crusts have come off. These slightly painful superficial defects have an elongated shape (up to 0.5 cm in width and up to 1 cm in length), an uneven surface and protrude slightly above the skin level. The evolution of these elements leads to the development of skin atrophy areas of different sizes and shapes, located in the circumference of a continuous atrophic lesion of baldness, sometimes in the form of lace, which causes: significant thinning of hair in this zone. Perhaps, in some patients with DF, who were diagnosed without histological confirmation.
In addition to decalvans folliculitis (DF), discoid lupus erythematosus also leads to the condition of pseudopelade. In the active stage, dermatoses differ in different types of primary rash element. In DF, the primary rash element is a small follicular inflammatory papule (2-5 mm in diameter), the evolution of which does not always end with the formation of a follicular pustule. In the center, these elements are penetrated by a hair (sometimes broken off), and in the circumference there is a narrow crown of hyperemia. Scraping the rash does not cause severe pain, and grayish scales and light yellow follicular crusts are easily separated from the affected surface. In the central part of the lesion, superficial atrophy of the skin with hair loss occurs without the formation of new rashes within it. DF is characterized by a long, chronic course regardless of the time of year and the absence of exacerbations after insolation. The lesion is often isolated, without foci in other locations. In typical cases of discoid lupus erythematosus, the primary rash element is an inflammatory spot that transforms into a plaque with hyperkeratosis, leading to atrophy. On its surface, there are firmly attached hyperkeratotic scales with unevenly located horny plugs. Scraping the lesions is painful, the scales are separated from the surface with difficulty. Along the periphery of the growing lesions, there is a hyperemic rim, and in the center, skin atrophy with telangiectasias and hair loss develops relatively quickly. Relapses of the dermatosis often occur on old atrophic areas of the skin. In addition to the scalp, lupus erythematosus lesions usually occur on the auricles, bridge of the nose, malar part of the cheeks, etc. With these dermatoses, histological changes in the lesions also differ significantly.
Folliculitis decalvans (or lupoid sycosis) differs from follicular decalvans lichen ruber by the appearance of the primary eruption element, which can be noticed only in the active stage of the disease. At the edges of the lesion of atrophic alopecia in DF there are small follicular inflammatory papules with a long evolution, leading to single follicular pustules. The defeat of the scalp by these dermatoses is usually isolated, rarely lupoid sycosis (or DF) can also affect the temporal region and lateral surface of the cheeks. In follicular decalvans lichen ruber, the primary eruption element is a small, follicular, conical papule with a horny spine in the center, leading to atrophic alopecia. The detection of lesions characteristic of lichen planus on other skin areas (including the axillary and pubic areas), on the oral mucosa and nails facilitates the preliminary diagnosis. It is important to confirm it by histological examination of the affected skin; pathomorphological changes in these dermatoses were described earlier.
The focus of decalvans folliculitis (DF, or luposus sycosis-LS) differs from luposus tuberculosis of the skin (serpiginizing form) by the primary element of the rash. Lupous tuberculosis (LT), which rarely affects the scalp, is characterized by flat, merging tubercles, yellowish-red in color, soft consistency with a positive "apple jelly" symptom during diascopy. The tubercles are not associated with hair follicles, and there are no pustules. With DF (or LS), in the border zone of the focus around follicular papules and single pustules, hyperemia is more pronounced in the form of a narrow border, and in the central zone there is smooth, superficial atrophy of the skin with baldness without new active rashes. In LT, which is often localized on the face, fresh tubercles (relapses on the scar) appear against the background of skin atrophy, and ulceration is also possible, which does not happen with DF (or LS). Dermatoses have different histological pictures. DF is characterized by intrafollicular microabscesses and perifollicular, mainly lymphohistiocytic infiltrates in the dermis. In LT, the tuberculous granuloma is located in the dermis and consists of clusters of epithelioid cells with foci of necrobiosis, several giant cells located among the epithelioid cells, and a shaft of lymphoid cells in the circumference.
The scalp is almost never affected by leishmaniasis, since the hair protects against mosquito bites. However, infection may occur at the hairline, leading to the development of late ulcerative (anthroponotic) leishmaniasis, acutely necrotizing (zoonotic) leishmaniasis, and even more rarely, chronic lupoid (tuberculous) cutaneous leishmaniasis (LLC). All forms of the disease result in the formation of a scar and persistent baldness within its borders. Manifestations of the lupoid form of cutaneous leishmaniasis may resemble a lesion of decalvans folliculitis (or lupoid sycosis). When differentiating them, it is necessary to determine the type of the primary eruption element, find out from the anamnesis whether the patient previously lived in areas endemic for leishmaniasis, and whether the patient has suffered cutaneous leishmaniasis in the past. Unlike DF (LS), LLK is characterized by small yellowish-brown tubercles that are not associated with hair follicles and appear around a scarring or cicatrized leishmanioma. The tubercles are usually localized on the face and are completely identical in size, color, consistency, and positive "apple jelly" symptom to the clinical manifestations of the flat form of lupus tuberculosis of the skin. Therefore, DF (LS) is otherwise differentiated from lupoid leishmaniasis of the skin in the same way as from lupus tuberculosis. Histological examination reveals a granuloma in the LLK focus, but the small amount of the pathogen in this rare form of the disease complicates diagnosis. Leishmania can be detected in the LLK focus by repeated bacterioscopic examination of thin smears prepared from scrapings of tubercle tissue and stained using the Giemsa-Romanovsky method.
Decalvans folliculitis (or DF) differs from serpiginizing tuberculous syphilid of the scalp (BS) by the primary eruption element and its different evolution. With DF, in the peripheral zone of the lesion there are small (2-5 mm) inflammatory follicular papules and individual follicular pustules, scales, crusts. With tuberculous serpiginizing syphilid, in the peripheral part of the lesion, lentil-sized tubercles are visible, dark red in color, smooth, hemispherical, dense, not associated with hair follicles. Along the edges of the lesion, they are closely grouped and merge, some of them ulcerate, forming round and oval ulcers with ridge-like, steeply breaking edges, a greasy bottom or bloody crusts on the surface. Such manifestations do not occur with DF (or LS), as well as the continuous, uneven, cellular atrophic scar with scalloped outlines and pigmentation along the periphery that remains after syphilid scarring. Pathomorphological changes in the lesions also differ. With tubercular syphilid, in contrast to DF, a granulomatous infiltrate is found in the dermis.
Erosive pustular dermatosis of the scalp is a very rare disease of unknown etiology, recently described in old women. The dermatosis has a long-term chronic relapsing course and also leads to a pseudopelade state. However, the clinical manifestations of EPD and DF differ. Thus, with EPD, flat pustules not associated with hair follicles, erosive-ulcerative skin defects and purulent-bloody crusts appear on the scalp. It should also be taken into account that DF, or LS, affects both women and men after puberty. The pathomorphological picture of these dermatoses is also different. In contrast to intrafollicular microabscesses with perifollicular and perivascular lymphohistiocytic infiltrates in the dermis, characteristic of DF, in EG, nonspecific inflammation in the dermis is accompanied by necrosis of the epidermis and its appendages, acanthosis and subcorneal pustules. Plasma cells predominate in the dermal infiltrate; in the initial phase, there are signs of leukocytoclastic vasculitis. However, direct immunofluorescence is usually negative.
Treatment of patients with decalvans folliculitis
Patients with suspected decalvans folliculitis (or lupoid sycosis) should be examined in detail to verify the diagnosis (including a biopsy of the affected skin) and to determine the specific pathogenesis of decreased resistance (chronic foci of infection, decompensated diabetes mellitus, chronic nephritis, dysproteinemia, etc.). General and external treatment of patients with this dermatosis is fundamentally little different from the treatment of vulgar (staphylococcal) sycosis. Antibiotics are prescribed systemically, taking into account the patient's tolerance and the sensitivity of the bacterial flora. Antiseptic, disinfectant antimicrobial agents are used externally: 0.1% chlorhexidine bigluconate solution, dioxidine solution, 0.01% miramistin solution, Fukortsin solution, as well as 2% mupirocin or 10% mafenide in the form of an ointment, etc. In the active peripheral zone of the lesion, hair is removed from the affected hair follicles. If these agents are insufficiently effective, it is recommended to prescribe combined antibiotics with a glucocorticosteroid in the form of a spray, lotion, or cream. Treatment is prescribed to patients during exacerbations, it is carried out for a long time, in courses, with a change of drugs. Now, X-ray therapy is almost never prescribed to the lesions, which was used earlier with a good, although not always long-term therapeutic effect. Comparison of the patterns-copies of the lesions in dynamics allows timely determination of the progression of the disease and the appointment of rational therapy.
Physician's tactics for pseudopelade
When examining a patient with pseudopelada, the primary task is to establish the nosological form of the dermatosis that led to focal atrophic alopecia. It is rational to first exclude those diseases that most often lead to the condition of pseudopelada: atrophic forms of lichen planus, discoid or disseminated lupus erythematosus, scleroderma, decalvans folliculitis, atrophic forms of mycosis of the skin, etc. On the way to the diagnosis, the doctor expects difficulties due to a number of objective factors. Thus, in some cases, active manifestations of dermatosis on the skin of the scalp are absent or uninformative. This may be due to the onset of remission of the disease or its latent ("smoldering") course. With predominant damage to the deep layers of the dermis of the scalp, inflammatory changes on the skin surface are barely noticeable. Therefore, the characteristic manifestations of various atrophic dermatoses in this localization are smoothed out, which causes a decrease in their clinical differences. The common and dominant rash is focal atrophy of the skin with baldness. This objectively complicates the diagnosis of the dermatosis that led to the development of pseudopelade, especially in cases where it is limited to the scalp.
To establish a diagnosis, anamnesis data, objective examination of not only the scalp, but also the rest of the skin surface, as well as hair, nails, visible mucous membranes and laboratory examination (primarily mycological and histological) are required. Based on the anamnesis data, the patient's age is established when focal atrophic alopecia was noticed. Thus, the existence of a skin defect on the scalp from birth and the absence of progression in the future allow us to suspect a developmental defect - congenital aplasia of the skin. Some genodermatoses often occur in children and can lead to a pseudopelade condition (for example, congenital and vulgar ichthyosis, congenital bullous dystrophic epidermolysis, incontinentia pigmenti (in girls) or Siemens follicular keratosis (in boys), etc.
When examining the affected scalp, special attention is paid to the area bordering the atrophic baldness focus, as well as to the remaining hair tufts in the pseudopelade area. In the active stage of the disease, a typical primary rash element and secondary rashes can be found in these areas. The doctor must consistently establish the morphology of the primary and secondary rash elements and their characteristics (color, size, shape, connection with the hair follicle, presence of a horny spine in the center, possible hair changes, etc.). In cases where the primary rash element cannot be detected, it is important to examine the secondary rashes (erosions or ulcers, crusts - purulent, bloody, serous or necrotic, etc.), which are a consequence of the evolution of the primary element and therefore indirectly help in its determination. Taking into account the type of primary element of the rash, differential diagnostics are carried out among dermatoses that manifest themselves with the same or similar rashes (see diagnostic algorithms for dermatoses leading to a pseudopelade condition).
After completing an objective examination of the pseudopelade area and forming a preliminary opinion regarding the genesis of the initial dermatosis, the doctor proceeds to a thorough examination of the patient. The entire surface of the skin, the condition of its appendages and visible mucous membranes are examined. If rashes are detected in other localizations (except for the scalp), their morphology and nosology are consistently established. Outside the scalp, atrophic dermatoses retain their characteristic clinical features. This applies equally to pathomorphological changes in the skin. Depending on the clinical manifestations, the necessary laboratory tests are carried out (mycological, bacteriological, histological, immunological, etc.).
In the vast majority of cases, the pseudopelade condition and skin lesions in other localizations are caused by the same dermatosis. Therefore, clarification of the morphology and nosology of rashes on smooth skin (or mucous membrane) practically predetermines the diagnosis of the underlying disease that led to pseudopelade. In each case of progressive pseudopelade, a histological examination of the affected skin is necessary, since it is unrealistic to establish a reliable diagnosis based only on the clinical picture. It is advisable to do a skin biopsy in the area where there are characteristic primary elements of the rash. The conclusion on the pathomorphological structure of the primary rash element is an important and decisive link in verifying the diagnosis.

