Key protein identified in preventing bone loss in osteoporosis
Last reviewed: 14.06.2024

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
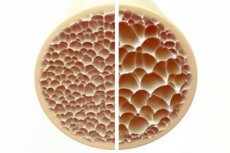
Osteoporosis, a condition characterized by porous and brittle bones, poses a significant threat to skeletal health. Bones, being the main structural support of the human body, provide vital support. When bone mass decreases, it not only impairs this support, but also impairs overall function, leading to decreased quality of life.
As the incidence of osteoporosis increases in the aging population, the strain on health care resources for long-term care increases. Therefore, it is necessary to understand the mechanisms contributing to the development of osteoporosis and develop effective targeted treatments to minimize its long-term impact.
Osteoblasts and osteoclasts are two types of cells that play a key role in the maintenance and remodeling of bone tissue. While osteoblasts are bone-forming cells and are responsible for the synthesis and deposition of new bone tissue, osteoclasts are bone-degrading cells involved in the decomposition and removal of old or damaged bone tissue.
An increase in the proportion of osteoclasts leads to bone loss in conditions such as osteoporosis, rheumatoid arthritis (inflammation of the joints) and bone metastases (cancer that has spread to the bones). Osteoclasts arise from the differentiation of macrophages or monocytes, which are types of immune cells.
Inhibiting osteoclast differentiation may thus serve as a therapeutic strategy to prevent bone loss. However, the precise molecular mechanisms that regulate the complex process of bone remodeling remain unclear.
In a new study, Professor Tadayoshi Hayata, Mr. Takuto Konno and Ms. Hitomi Murachi from Tokyo University of Science, together with colleagues, delved deeper into the molecular regulation of osteoclast differentiation. Stimulation by receptor nuclear factor kappa B activator ligand (RANKL) induces differentiation of macrophages into osteoclasts.
In addition, bone morphogenetic protein (BMP) and transforming growth factor (TGF)-β signaling pathways have been implicated in the regulation of RANKL-mediated osteoclast differentiation. In the current study, the researchers sought to examine the role of Ctdnep1, a phosphatase (an enzyme that removes phosphate groups) that is reported to suppress the BMP and TGF-β signaling pathways.
The study was published in the journal Biochemical and Biophysical Research Communications.
Professor Hayata states: "RANKL acts as an 'accelerator' for osteoclast differentiation. Driving a car requires not only an accelerator, but also brakes. Here we found that Ctdnep1 acts as a 'brake' in osteoclast differentiation."
The researchers first examined the expression of Ctdnep1 in macrophages from mice treated with RANKL and control cells without treatment. They noted that Ctdnep1 expression did not change in response to RANKL stimulation. However, it was localized in the cytoplasm in granular form in macrophages and differentiated into osteoclasts, different from its normal perinuclear localization in other cell types, suggesting its cytoplasmic function in osteoclast differentiation.
In addition, Ctdnep1 knockout (downregulation of the gene) resulted in an increase in the number of osteoclasts positive for tartrate-resistant acid phosphatase (TRAP), where TRAP is a marker of differentiated osteoclasts.
Ctdnep1 knockout resulted in increased expression of key differentiation markers, including "Nfatc1," a master transcription factor induced by RANKL for osteoclast differentiation. These results support an “inhibitory function” of Ctdnep1, whereby it negatively regulates osteoclast differentiation. Moreover, knockout of Ctdnep1 also resulted in increased calcium phosphate absorption, suggesting an inhibitory role for Ctdnep1 in bone resorption.
Finally, although Ctdnep1 knockout did not alter the BMP and TGF-β signaling pathways, Ctdnep1-deficient cells showed increased levels of phosphorylated (activated) proteins that are products of the RANKL signaling pathway. These results suggest that the suppressive effect of Ctdnep1 on osteoclast differentiation may not be mediated through the BMP and TGF-β signaling pathways, but through negative regulation of the RANKL signaling pathway and Nfatc1 protein levels.
Overall, these results provide new insights into the osteoclast differentiation process and identify potential therapeutic targets that can be used to develop treatments aimed at reducing bone loss due to osteoclast overactivity. In addition to diseases characterized by bone loss, Ctdnep1 has also been identified as a causative factor in medulloblastoma, a childhood brain tumor. The authors are optimistic that their research can be extended to other human diseases beyond bone metabolism.
Professor Hayata concludes: "Our results suggest that Ctdnep1 is required to prevent excessive osteoclastogenesis. These results may further expand knowledge of how the phosphorylation-dephosphorylation network controls osteoclast differentiation and may provide new therapeutic strategies for the treatment of bone diseases associated with excessive osteoclast activity."
