Low oxygen levels and sleep apnea linked to epilepsy in older adults
Last reviewed: 14.06.2024

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.

Sleep apnea and low oxygen levels during sleep are associated with epilepsy that first occurs after age 60, known as late-onset epilepsy, according to a new study published in the journal Sleep.
The association was independent of other known risk factors for late-onset epilepsy and sleep apnea, such as hypertension and stroke. These findings may help better understand the relationship between sleep disorders and late-onset epilepsy, as well as identify potential targets for treatment.
"A growing body of evidence suggests that late-onset epilepsy may indicate the presence of vascular disease or neurodegenerative disease, even potentially as a preclinical marker of neurodegenerative disease," said Rebecca Gottesman, MD, chief of the stroke branch at the NIH's National Institute of Neurological Disorders and Stroke (NINDS) and an author of the study.
"Compared to other age groups, older adults have the highest rate of new cases of epilepsy — up to half of which have no clear cause. Sleep apnea is common among people with epilepsy, but the association is poorly understood."
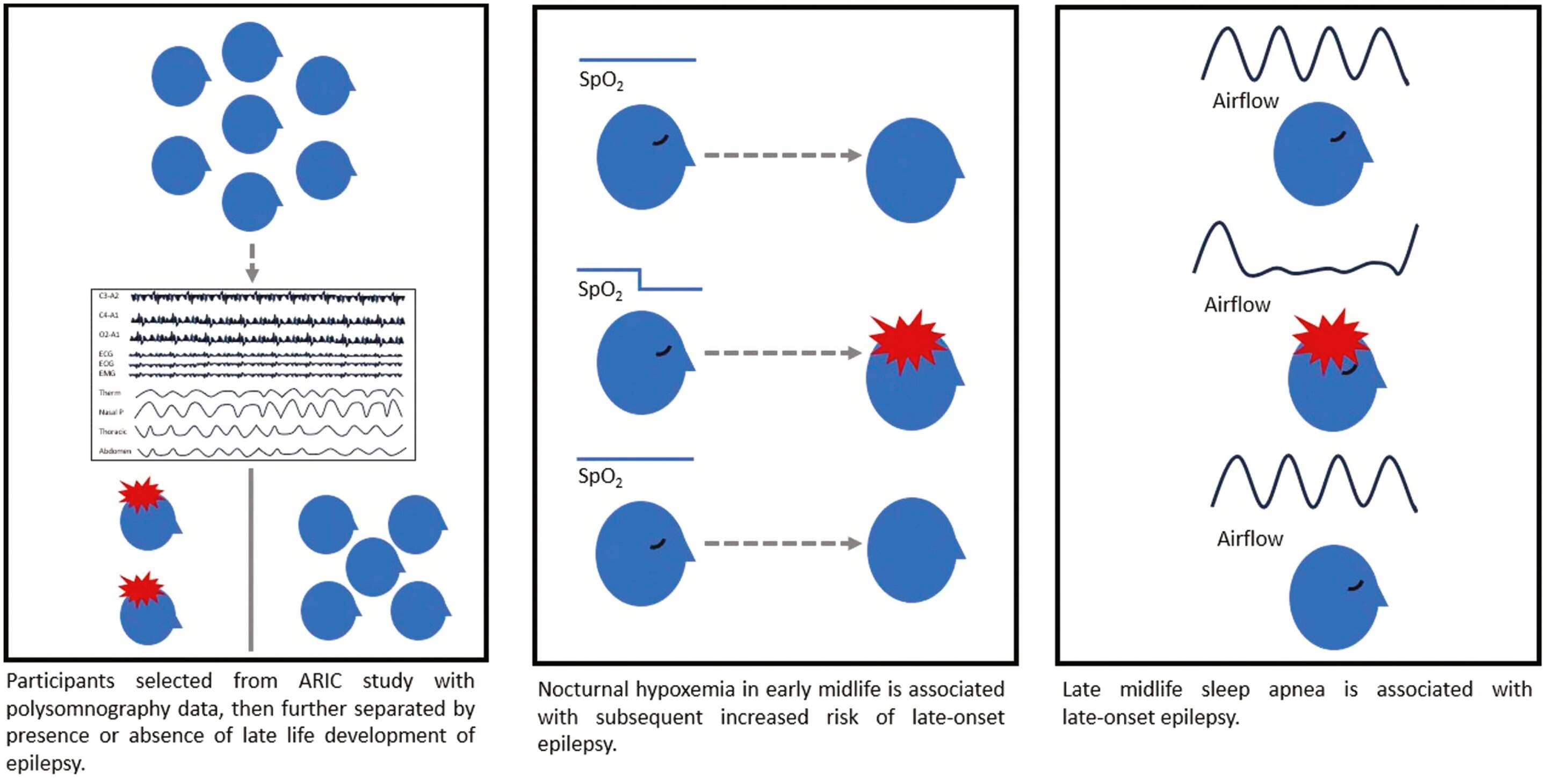
Researchers led by Christopher Carosella, MD, assistant professor of neurology at Johns Hopkins University in Baltimore, identified cases of late-onset epilepsy using Medicare data and analyzed sleep data from more than 1,300 participants in the Sleep-Disordered Breathing and Cardiovascular Disease Study.
They found that people whose oxygen saturation during sleep fell below 80%, a condition known as nocturnal hypoxia, were three times more likely to develop late-onset epilepsy than those who did not have similarly low oxygen levels. In addition, participants who self-reported sleep apnea later in life were twice as likely to develop late-onset epilepsy as those who did not have the sleep disorder.
The degree of sleep hypoxia was associated with late-onset epilepsy independent of other underlying medical problems and demographic factors. The authors note that the study found no association between the apnea-hypopnea index, a traditional measure of sleep apnea severity.
Sleep apnea is known to be a risk factor for poor brain health in other ways, including stroke and dementia, but the link to epilepsy has not been previously described. The link to hypoxia suggests that repeated chronic exposure to low oxygen levels overnight may lead to changes in the brain that ultimately lead to risk of epilepsy.
The study cannot determine whether treating or preventing sleep apnea can reduce the risk of epilepsy, but it does indicate that it may be an important potential target for reducing the risk of late-onset epilepsy.
"Discovering a reversible cause for the development of any type of idiopathic epilepsy is a cherished goal for epilepsy researchers or clinicians," said Dr. Carosella. "We hope that this study can be a small first step in this direction, as well as a stimulus for the assessment and treatment of sleep disorders in patients with epilepsy."
Because sleep apnea can have an impact on cardiovascular and brain health, the results could also eventually help identify people at risk for some of these other conditions, providing a potential opportunity for treatment and prevention. p>
Future research is needed to evaluate whether treating sleep apnea in patients at risk for late-onset epilepsy can help prevent the onset of the disease.
