Small molecule shows promise for myelin sheath repair
Last reviewed: 14.06.2024

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
When treated with a new protein function inhibitor called ESI1, mice mimicking symptoms of multiple sclerosis (MS) and laboratory-grown human brain cells demonstrated the ability to repair vital myelin sheaths, which protect healthy axonal function.
This breakthrough, published in the journal Cell appears to overcome challenges that have long hampered previous attempts to reverse a form of nerve damage that robs people with MS of motor control and cognitive function gradually declines in many people as they age.
"There are currently no effective therapies to repair myelin damage in devastating demyelinating diseases such as MS," says study corresponding author Q. Richard Lu, Ph.D., a brain research expert at Cincinnati Children's. "These results are significant because they suggest new treatment pathways that potentially change the therapeutic focus from managing symptoms to actively promoting myelin repair and regeneration."
Stimulating healing by removing obstacles
The critical insight that led to the new findings was the observation that damaged areas of the brain in MS still contain the type of cells needed to repair myelin damage, but the disease activates other cell types and signals that work together to suppress the repair function.
These beneficial cells in the brain, called oligodendrocytes, are responsible for producing myelin sheaths, which wrap around the axons of nerve cells, like plastic insulation around a wire. When protective myelin is damaged, whether due to disease or wear and tear with age, nerve signaling is disrupted. Depending on where the damaged nerves lead, these disorders can affect movement, vision, thinking, etc.
Essentially, the research team has found a way to unblock the suppressed repair process, freeing oligodendrocytes (OLs) to do their job.
Identifying the genetic changes and signals involved in the process of suppression of repair and finding a small molecule compound that can reverse the suppression has been a challenging task. The project, which spanned more than five years, included four co-authors and 29 co-authors from Cincinnati Children's, the University of Cincinnati and 14 other institutions, including universities in Australia, China, Germany, India, Singapore and the UK.
The main findings of the team:
Identification of a mechanism that prevents myelin production in MS
Analysis of preserved autopsy tissues revealed that OLs in MS lesions lack an activating histone mark called H3K27ac, while expressing high levels of two other repressive histone marks, H3K27me3 and H3K9me3, associated with suppression of genetic activity.
Finding a compound that can reverse the suppression
The research team examined a library of hundreds of small molecule compounds known to target enzymes that can modify gene expression and influence suppressed OLs. The team determined that the compound ESI1 (Epigenetic Suppression Inhibitor-1) was nearly five times more potent than any other compound examined.
The compound tripled the levels of the desirable histone mark H3K27ac in OLs, while dramatically reducing the levels of two repressive histone marks. In addition, the study revealed a new way in which ESI1 promotes the creation of special membrane-free regulatory nodes, known as “biomolecular condensates,” inside the cell nucleus that control fat and cholesterol levels.
These nodes act as focal points to enhance the production of essential fats and cholesterol needed to create myelin, an important component of nerve fibers.
Demonstration of benefits in mice and lab-grown human tissue
In both aging and MS-mimicking mice, ESI1 treatment stimulated myelin sheath production and improved lost neurological function. Testing included tracking gene activation, measuring microscopic new myelin sheaths surrounding axons, and observing that treated mice performed a water maze faster.
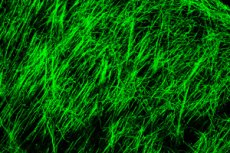
The team then tested the treatment on laboratory-grown human brain cells. The team used a type of brain organoid, myelin organoids, which are greatly simplified compared to a full brain but still produce complex myelinating cells. When the organoids were exposed to ESI1, the treatment lengthened the myelin sheath of the myelinating cells, the study reported.
Consequences and next steps
MS is the best known of several major neurodegenerative diseases. The new findings could inspire a new approach to stopping the degenerative effects of these conditions, Lu says.
Myelin regeneration treatments may also be helpful for people recovering from brain and spinal cord injuries.
But the most far-reaching implication of the study is the possibility of using ESI1 or similar compounds to help slow or even reverse the cognitive loss that often occurs with age. Many studies have shown that loss of myelin plays a role in age-related cognitive loss, Lu says.
However, more research is needed to determine whether clinical trials of ESI1 can be initiated as a potential treatment. For example, the effects of ESI1 may require modification by adjusting the dose and duration of treatment or using “pulsatile therapy” during specific time windows. More research is also needed to determine whether even more effective compounds than ESI1 can be developed.
"This study is just the beginning," Lu says. "Prior to the discovery of ESI1, most scientists believed that failure of remyelination in MS was due to arrested progenitor development. We now show proof of concept that reversal inhibition of activity in OLs present in the damaged brain may allow myelin regeneration."
