New publications
B cells can be modified to prevent symptoms of multiple sclerosis
Last reviewed: 02.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
B cells can control myeloid cell responses through the release of certain cytokines (small proteins that control the growth and activity of immune cells), challenging the previously held belief that only T cells coordinate immune responses.
In people with multiple sclerosis (MS), abnormally active respiration in B cells stimulates pro-inflammatory responses in myeloid cells and T cells, causing them to attack the protective sheath (myelin) that covers nerve fibers, causing nerve damage and MS symptoms.
A new class of drugs called Bruton tyrosine kinase (BTK) inhibitors may reverse this abnormal B-cell breathing and stop the signals that lead to MS flare-ups. The study, led by the Perelman School of Medicine at the University of Pennsylvania, was published in the journal Science Immunology.
"Experts previously believed that T cells are the primary orchestrators of responses from other types of immune cells, and that MS is primarily caused by overly activated T cells," said Dr. Amit Bar-Or, professor of neurology and director of the Center for Neuroinflammation and Neurotherapeutics at the University of Pennsylvania.
"This study highlights that it really matters how different cell types interact, and that myeloid-modulating B cells play a much more active role in the immune system than we thought."
A healthy immune system constantly responds to stimuli by activating or suppressing immune responses, in part by releasing various cytokines that tell other types of cells how to respond. Typically, every immune response triggers a counter-reaction, and this constant "push and pull" helps maintain the proper balance between immune responses.
In this way, the human immune system can, on the one hand, respond to infection, but also ensure that the response does not become overactive and cause harm to the body, as can happen in autoimmune diseases such as MS.
In this study, the researchers used both human samples and mouse models of MS to show that not only do cytokine signals between B cells and T cells go awry in MS, but that B cells from MS patients produce an abnormal cytokine profile that causes myeloid cells to generate an inflammatory response.
They found that all of these actions could be traced to metabolic dysregulation in a process in B cells called oxidative phosphorylation, a type of mitochondrial respiration. The researchers found that normal B cells can break down oxygen and release chemical energy signals that trigger a further reaction in the B cells themselves, and then also in the myeloid cells, telling them to mount a pro- or anti-inflammatory response.
However, when this B cell metabolism is overactive, as it is in MS, the signals lead to abnormal myeloid and T cell responses that are associated with flare-ups of MS symptoms.
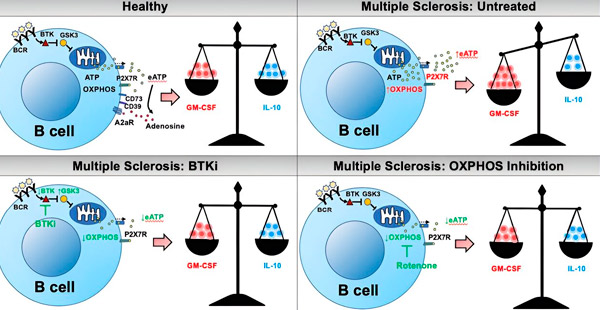
Metabolic regulation of cytokine production by B cells: implications for the pathogenesis and therapy of MS. Source: Science Immunology (2024). DOI: 10.1126/sciimmunol.adk0865
"An exciting approach for new treatments for MS may be to partially suppress respiration in B cells, which could stop the cascade of interactions between immune cells that drives inflammation and MS activity," Bar-Or said.
The authors previously showed that a new class of drugs called BTK inhibitors do just that. These agents slow down overactive B-cell respiration and "calm" the B cells of MS patients so that they don't secrete the same abnormal cytokine profile that triggers abnormal pro-inflammatory responses from myeloid cells and T cells.
Existing MS treatments, such as anti-CD20 therapies, deplete B cells. However, because B cells are destroyed, the patient’s immune system may be compromised, making it difficult to respond to infections or vaccinations. In contrast, BTK inhibitors do not deplete B cells, but correct a metabolic abnormality, making B cells less likely to trigger pro-inflammatory responses in other cells.
