New publications
Without pills and immune suppression: the world's first β-cell transplant for diabetes
Last reviewed: 09.08.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
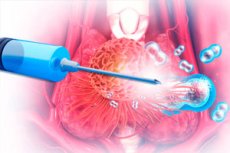
In a unique case, a 42-year-old man with a 37-year history of severe type 1 diabetes received a transplant of genetically modified islet β-cells from a donor without taking a single drop of immunosuppressants. Researchers from Sweden and Norway used CRISPR–Cas12b to remove key HLA I and II markers and then boosted expression of “non-self” CD47 so that the cells would “fuse” with the recipient’s tissues and avoid both adaptive and innate rejection. The study is published in NEJM.
How was it arranged?
Isolation and editing
- Donor islet cells were "crushed" into single β-cells.
- CRISPR–Cas12b “knocked out” the B2M and CIITA genes (the basis of HLA-I and HLA-II).
- Lentiviral transduction inserted the CD47 gene into the cells, blocking attacks by macrophages and NK cells.
- The final UP421 product contained ~86% HLA I–negative, 100% HLA II–negative, and nearly 50% CD47-enhanced cells.
Transplantation
- 79.6 million edited β-cells were injected intramuscularly into the forearm muscle - 17 small "bead" injections along the fibers.
- The patient did not receive steroids, anti-CD3, or cyclosporine.
Immunity control
- Conventional (non-edited) islet cells and double knockouts elicited potent T cell and innate responses: peak activity at days 7–21, a clear IgM→IgG switch, and cytotoxicity in a PBMC+serum cocktail.
- Hypoimmune (HIP) cells survived 12 weeks without evidence of rejection, antibodies or cytotoxicity.
Restoration of pancreatic function
- At 0 week, C-peptide was absent, but 4–12 weeks after transplantation, the patient developed a glucose-dependent increase in C-peptide with food intake.
- At the same time, EHD decreased by 42%, and the daily dose of exogenous insulin was adjusted upward to prevent “hyperspikes” to protect the new transplant.
- PET-MRI confirmed the survival and vascularization of the "islands" in the muscle.
Safety and side effects
Over 12 weeks, only 4 adverse events were recorded (mild thrombophlebitis and hand paresthesia), none of which were serious or related to the genetically modified cells.
Significance of the study
- The world's first person to receive a hypoimmune allogeneic islet transplant without immunosuppression.
- CRISPR–Cas12b + CD47 overexpression has been shown to protect against T cells, NK cells, macrophages and antibodies.
- Clinical feasibility has been confirmed: stable and physiological secretion of insulin from transplanted cells.
“This is a proof of concept that genetically modified ‘invisible’ β-cells can save patients from lifelong pills and immunosuppressants,” comments Dr. Johan Schön.
Next steps
By increasing the cell dose to a level that provides complete insulin independence and prolonging the observation, a series of such transplants could offer a real chance of a “cure” for millions of people with type 1 diabetes in the future.
