New publications
Turning a tumor's "shield" into a weapon against the tumor itself
Last reviewed: 02.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
According to Peter Insio Wang, tumor cells are “cunning.” They have sinister ways of evading the human immune responses that fight against these cancerous invaders. Tumor cells express programmed death-ligand 1 (PD-L1) molecules, which act as a protective shield that suppresses our immune cells, creating an obstacle to targeted cancer immunotherapies.
Wang, the Alfred E. Mann Chair in Biomedical Engineering and holder of the Dwight C. and Hildagard E. Baum Chair in Biomedical Engineering, leads a laboratory dedicated to pioneering research into engineered immunotherapies that harness the human immune system to create a future arsenal in the fight against cancer.
Researchers in Wang's lab have developed a new approach that turns a tumor cell's insidious defense mechanisms against itself, turning these "shield" molecules into targets for Wang's lab-engineered chimeric antigen receptor (CAR) T cells programmed to attack cancer.
The work, conducted by Wang's lab postdoctoral fellow Lingshan Zhu, along with Wang, research scientist Longwei Liu and their co-authors, was published in the journal ACS Nano.
CAR T-cell therapy is a revolutionary cancer treatment in which T cells, a type of white blood cell, are removed from a patient and given a unique chimeric antigen receptor (CAR). The CAR binds to antigens associated with cancer cells, directing the T cells to kill the cancer cells.
The latest work from Wang's lab is a designed monobody for CAR T cells, which the team calls PDbody, that binds to the PD-L1 protein on a cancer cell, allowing the CAR to recognize the tumor cell and block its defenses.
"Think of CAR as a real car. You have an engine and gas. But you also have a brake. Essentially, the engine and gas push CAR T to move forward and kill the tumor. But PD-L1 acts as a brake that stops it," Wang said.
In this work, Zhu, Liu, Wang and team engineered T cells to block this inhibitory "brake" mechanism and make the PD-L1 molecule a target for destruction.
"This chimeric PDbody-CAR molecule can make our CAR T cells attack, recognize and kill the tumor. At the same time, it will block and prevent the tumor cell from stopping the CAR T cell's attack. In this way, our CAR T cells will be more powerful," Wang said.
CAR T-cell therapy is most effective against "wet" cancers such as leukemia. The challenge for researchers has been to develop advanced CAR T cells that can differentiate between cancer and healthy cells.
Wang's lab is exploring ways to target the technology to tumors so that CAR T cells are activated at the tumor site without affecting healthy tissue.
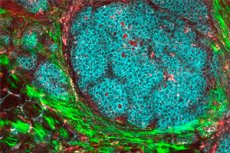
In this work, the team focused on a highly invasive form of breast cancer that expresses the protein PD-L1. However, PD-L1 is also expressed by other types of cells. So the researchers looked at the unique tumor microenvironment – the cells and matrices immediately surrounding the tumor – to ensure that their designed PDbody would bind more specifically to cancer cells.
"We know that the pH in the tumor microenvironment is relatively low - it's a little acidic," Zhu said. "So we wanted our PDbody to have better binding ability in an acidic microenvironment, which would help our PDbody distinguish tumor cells from other surrounding cells."
To improve the precision of treatment, the team used a genetic "gate" system called SynNotch, which ensures that CAR T cells with PDbody attack only cancer cells expressing a different protein known as CD19, reducing the risk of damaging healthy cells.
"Simply put, T cells will only be activated at the tumor site thanks to this SynNotch gate system," Zhu said. "Not only is the pH more acidic, but the tumor cell surface will determine whether the T cell will be activated, giving us two levels of control."
Zhu noted that the team used a mouse model, and the results showed that the SynNotch gating system directs CAR T cells with PDbody to activate only at the tumor site, killing tumor cells while remaining safe for other parts of the animal.
An evolution-inspired process to create PDbody
The team used computational methods and took inspiration from the process of evolution to create their specialized PDbodies. Directed evolution is a process used in biomedical engineering to mimic the process of natural selection in a laboratory setting.
The researchers created a directed evolution platform with a giant library of iterations of their designed protein to discover which version might be most effective.
"We needed to create something that would recognize PD-L1 on the surface of the tumor," Wang said.
"Using directed evolution, we selected a large number of different monobody mutations to select which one would bind to PD-L1. The selected version has these features that can not only recognize tumor PD-L1, but also block the brake mechanism that it has, and then direct the CAR T cell to the surface of the tumor to attack and kill the tumor cells."
"Imagine if you wanted to find a very specific fish in the ocean – that would be really difficult," Liu said. "But now with the directed evolution platform we've developed, we have a way to fish out these specific proteins with the right function."
The research team is now exploring how to optimize the proteins to create even more precise and effective CAR T cells before moving into clinical applications. This also includes integrating the proteins with Wang’s lab’s breakthrough focused ultrasound applications to remotely control CAR T cells so that they are activated only at tumor sites.
"We now have all these genetic tools to manipulate, control and program these immune cells to have so much power and function," Wang said. "We hope to create new ways to direct their function for particularly challenging solid tumor treatments."
