New publications
Study reveals differences in brain responses in men and women to low sex drive
Last reviewed: 02.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.

In a recent study published in the journal Scientific Reports, researchers examined the neurofunctional determinants of hypoactive sexual desire disorder (HDSS) in men and women. In simple terms, it’s a condition in which people experience a distressing decrease in sexual desire. The disorder has been studied in women before, but never in men. In this study, the researchers used functional magnetic resonance imaging (fMRI) combined with psychometric questionnaires to assess the neurofunctional responses of men and women to sexual and non-sexual video presentations.
This study found that women with hypoactive sexual desire follow a top-down theory, which posits that hyperactivity in higher cognitive areas of the brain suppresses lower levels of the sexual brain regions. Unlike women, this neurofunctional pattern was not observed in men, highlighting the sexual dimorphism in how male and female brains process sexual stimuli. Although the researchers were unable to elucidate the cognitive mechanisms underlying HDSS in men, this study highlights the need for more research on HDSS in men and suggests that low sexual desire treatments used for women may not produce the desired results in men.
What is HDSS and what do we know about the condition?
The Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Revised (DSM-IV-TR) defines hypoactive sexual desire disorder (HDSS) as "persistent sexual fantasies and desire for sexual activity that cause marked distress or interpersonal difficulty." Popularly referred to as "diminished sexual desire," "hyposexuality," or "inhibited sexual desire," HDSS is a sexual dysfunction whose symptoms include a significant lack of sexual fantasies and arousal, even in sexually active men and women. Given the significant social and interpersonal distress caused by HDSS, the condition is often associated with depression and similar emotional disorders.
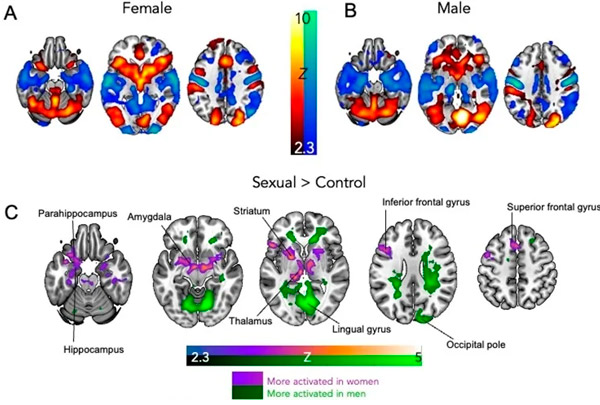
Women with HSDD show greater limbic system activation to sexual videos than men.
(A) Average results for a group of women with HSDD showing brain activation (red/yellow) and deactivation (blue/green) to sex videos compared to controls (exercise).
(B) Average results for a group of men with HSDD showing brain activation and deactivation to sex videos compared to controls (exercise).
(C) Brain regions that are more activated in women (compared to men) to sex videos compared to controls are shown in purple. Brain regions that are more activated in men (compared to women) to sex videos compared to controls are shown in green.
The results are cluster-corrected and the cut-off values are Z = 2.3, P < 0.05, N = 64 (32 women, 32 men).
Study: Women with HSDD show greater limbic system activation to sex videos than men. (A) Mean results for the female HSDD group showing brain activation (red/yellow) and deactivation (blue/green) to sex videos compared to controls (exercise). (B) Mean results for the male HSDD group showing brain activation and deactivation to sex videos compared to controls (exercise). (C) Brain regions that are more activated in females (compared to males) to sex videos compared to controls are shown in purple. Brain regions that are more activated in males (compared to females) to sex videos compared to controls are shown in green. Results are cluster-corrected and thresholded at Z = 2.3, P < 0.05, N = 64 (32 females, 32 males). Study: Women and men with distressing low sexual desire show sex differences in brain processing.
First identified in 1980 (DSM-III) and formally defined in 1987 (DSM-III-R), HDSS is a clinically distinct disorder from conditions such as asexuality and erectile dysfunction. Its causes may include a history of sexual abuse, altered sex hormone levels, or other medical conditions such as cancer, diabetes, and multiple sclerosis. Despite its relatively recent description, HDSS is one of the most common sexual disorders worldwide, estimated to affect 10% of all women and 8% of all men. Given the social stigma associated with the condition, these figures are considered to be severely underestimated, highlighting the need for interventions to combat the impact of neurofunctional disorders on quality of life.
Unfortunately, despite the limited research on HDSS, the available scientific literature on the topic focuses almost exclusively on women, with the only previous study in men using questionable methodologies. This disparity in research is reflected in treatment options, with two medically licensed interventions for American women and none for American men. A significant number of cases of HDSS in men are misdiagnosed as erectile dysfunction, exacerbating the stress and mental health associated with the condition.
In this study, the researchers aimed to use functional magnetic resonance imaging (fMRI) in combination with several psychometric questionnaires to assess the neurofunctional responses of men and women with HDSS to sexual and non-sexual stimuli (in this case video presentations – visual sexual stimuli). The study participants were men and women with clinically confirmed HDSS (ICD-11) recruited through advertisements across London (print and online media). Screening of participants consisted of a telephone interview followed by an in-person medical assessment (blood and questionnaires) to distinguish acquired from generalised HDSS. To avoid confounding with existing clinical conditions, people with a history of psychiatric illness or currently receiving treatment were excluded from the study.
"...participants had to be in a stable, communicative, monogamous relationship for more than 6 months. Participants were excluded if they had a history of unresolved sexual trauma, abuse, or aggression, use of medications (prescription or over-the-counter) or herbal preparations to enhance sexual desire, arousal, or performance, or if they had contraindications for MRI scanning."
The experimental intervention involved the presentation of 20-second silent sexual videos (cases) interspersed with neutral non-sexual exercise videos (controls) over a 12-minute standardized block (rated on a Likert scale). Participants were required to complete the Sexual Desire and Arousal Inventory (SADI) immediately before and after the experimental intervention, which measured 54 descriptors in the categories of evaluative, negative, physiological, and motivational. During the experimental intervention, participants underwent simultaneous fMRI and pulse oximetry.
Data processing included correlations between questionnaire results and fMRI arousal images, matches between activation patterns in men and women (via Dice coefficients) to sexual and non-sexual visual stimuli, and analysis of brain regions of interest (ROIs), especially those corresponding to the neural sexual network (amygdala, hypothalamus, insular cortex, precentral gyrus, striatum, and thalamus).
Following the screening process, 32 men and 32 women with clinically confirmed HDSS remained in the study sample. While men were on average nine years older than their female counterparts, Dice coefficient results suggest that age did not influence the study results. An additional 20 “healthy” men and women were recruited to confirm differences between sexual and non-sexual stimuli and to establish baseline levels of neural activation responses.
"The results are somewhat consistent with previous studies in individuals with normal sexual desire, suggesting that women and men show similar general patterns of activation to visual sexual stimuli. However, notable differences were observed in the activation of limbic brain regions in women and men with HDSS, particularly the hypothalamus, amygdala, and thalamus, which are key structures associated with emotional processing and sexual motivation."
The present study highlights that the neural genital network in females with HDSS shows activation when presented with sexual stimuli; however, these "low-level" neurofunctional centers (limbic regions) are masked by the simultaneous activation of higher cortical regions, supporting the "top-down" hypothesis proposed by Cacioppo. In contrast, no neural genital network activation was observed in males with HDSS, suggesting that visual sexual cues are not effectively transmitted to the emotional centers associated with sexual response. This study is the first to explain the sexual dimorphism between male and female neurofunctional HDSS. It highlights the need for additional research, particularly in males, before effective therapeutic interventions can be developed for this condition.
