New publications
Study reveals linked biological pathways causing skin inflammation in psoriasis
Last reviewed: 02.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.

A new study has identified a biological pathway — a set of linked reactions in the body — that leads to the inflammation seen in the skin condition psoriasis. The study's authors say the findings could lead to better treatments for all inflammatory skin conditions, including atopic and allergic dermatitis, as well as a type of boil called hidradenitis suppurativa.
Inflammation is the body's natural response to irritation and infection, but if left unchecked it can lead to the reddish, scaly, itchy lesions characteristic of these skin conditions.
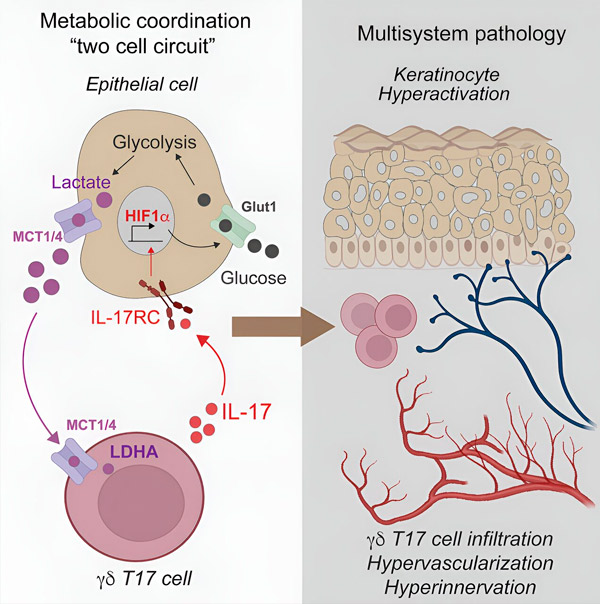
Lead researchers at NYU Langone Health have discovered that the interleukin-17 (IL-17) pathway, whose activity is blocked by existing anti-inflammatory drugs, activates a protein called hypoxia-inducible factor 1-alpha (HIF-1-alpha) in psoriasis. The researchers say IL-17 has long been known to be active in inflammation, but the role of HIF-1-alpha has been unclear until now.
The team also found that HIF-1alpha allows inflammatory skin cells to more actively break down sugar for energy, keeping them metabolized and producing a byproduct called lactate. When inflammatory T cells consume lactate, it triggers the production of IL-17, increasing inflammation.
The results showed that in skin samples from people with psoriasis, measures of gene activity around IL-17 and HIF-1alpha were similar, suggesting that the two factors were linked. Experiments in mice that had been induced to develop psoriasis showed that subsequent treatment with an experimental drug that blocks the action of HIF-1alpha, called BAY-87-2243, resolved the inflammatory skin lesions.
Additionally, skin samples from 10 patients successfully treated with the anti-inflammatory drug etanercept showed decreased activity of both IL-17 and HIF-1alpha, indicating that blocking IL-17 also blocks HIF-1alpha.
"Our findings indicate that HIF-1alpha activation is a key driver of the metabolic dysfunction seen in psoriasis, and that its action is triggered by IL-17, another key inflammatory signaling molecule," said lead study author Shruti Naik, PhD, an associate professor in the NYU Grossman School of Medicine, Department of Pathology and Medicine, and the Ronald O. Perelman Department of Dermatology.
Additional experiments were performed on skin samples from five psoriasis patients whose healthy and inflamed skin were treated separately with either BAY-87-2243 or an existing topical drug combination (calcipotriene and betamethasone dipropionate).
The researchers then compared differences in inflammatory gene activity as a measure of impact and found that the HIF-1alpha inhibitor had a greater impact than existing topical treatments. Specifically, skin samples that responded to HIF-1alpha therapy had 2,698 genes that were differentially expressed, while samples treated with standard therapy had 147 genes that were differentially expressed.
Genetic analysis of skin samples from another 24 psoriasis patients treated with the IL-17A-blocking drug secukinumab showed only a decrease, not an increase, in the activity of HIF-1alpha-related genes, compared with the activity of HIF-1alpha genes in nine healthy patients without psoriasis. The researchers believe this indicates that blocking HIF-1alpha action depends on blocking IL-17.
Additional experiments in mice showed that blocking sugar (glucose) uptake in the skin slowed the growth of psoriatic disease by limiting glucose metabolism, or glycolysis. The number of inflammatory T cells and IL-17 levels were reduced. Levels of lactate, a major byproduct of glycolysis, were also found to be reduced in psoriatic skin cell cultures after exposure to the glycolysis-inhibiting drug 2-DG.
Directly targeting lactate production in psoriatic mice using a skin cream containing lactate dehydrogenase, which breaks down lactate, also slowed disease progression in the skin, with a reduction in inflammatory gamma delta T cells and decreased IL-17 activity. Gamma delta T cells have been shown to take up lactate and use it to produce IL-17.
"Our findings suggest that blocking the action of HIF-1alpha or its glycolytic metabolic support may be an effective therapy for curbing inflammation," added Naik, who is also associate director of the Judith and Stuart Colton Center for Autoimmunity at NYU Langone.
"Evidence of decreased HIF-1alpha action, or suppression, could also serve as a biomarker, or molecular signature, that other anti-inflammatory therapies are working," said Dr. Jose W. Sher, co-author of the study and an assistant professor of medicine at NYU Grossman School of Medicine.
Sher, who is also director of the Psoriatic Arthritis Center and the Judith and Stuart Colton Center for Autoimmunity at NYU Langone, says the team plans to develop experimental drugs that can block the action of HIF-1alpha and lactate in the skin "to end the vicious cycle of IL-17-driven inflammation in skin diseases. Our study significantly expands the possibilities for therapeutic options."
Naik emphasizes that while many available psoriasis therapies, including steroids and immunosuppressive drugs, reduce inflammation and symptoms, they do not cure the disease. She said more experiments are needed to clarify which experimental drug works best at inhibiting HIF-1alpha before clinical trials can begin. Naik and co-lead study co-authors Ipsita Subudhi and Piotr Konieczny have filed a patent application (U.S. application number 63/540,794) for a therapy for inflammatory skin diseases based on their work on inhibiting HIF-1alpha.
It is estimated that more than 8 million Americans and 125 million people worldwide suffer from psoriatic disease. The condition affects both men and women equally.
The results are published in the journal Immunity.
