New publications
Researchers discover how B cells detect cancer in the body
Last reviewed: 02.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Scientists have discovered key features of immune B cells that make them successful in fighting tumours, including cases where cancer has spread to other parts of the body.
In the journal Nature Immunology, the researchers describe the development of a computational tool to identify these cancer-fighting immune cells, which could lead to better personalized immunotherapies. Currently, most immunotherapies only work for a minority of patients, and researchers are working hard to expand the group of patients who could benefit from them.
Scientists from the Department of Biochemistry at the University of Oxford, the Institute of Cancer Research London and the University of Cambridge took biopsies from breast cancer patients and used a technique called B-cell receptor sequencing to identify genetic variations in B cells.
B cells, like the more commonly known T cells, are part of the immune system, helping the body fight infections and cancer. They produce proteins called antibodies that stick to harmful substances like viruses and cancer and recruit other parts of the immune system to destroy them. When a receptor on a B cell recognizes and binds to a cancer cell, the B cell undergoes changes and becomes even more effective at targeting those cancer cells.
Associate Professor Rachel Bashford-Rogers, lead author of the study and Associate Professor in the Department of Biochemistry at the University of Oxford, said: "Using a combination of different genetic techniques, we showed that both B cell and T cell immune responses evolve in tandem with changes occurring at individual tumour sites in the body. However, some B cell responses were seen across many or all tumour sites, suggesting that they are seeking out cancer cells in different locations."
"Here we have identified a common and predictable pattern of immune surveillance of cells across multiple tumor sites and developed a tool to accurately identify these cells. We show that this also applies to other diseases, including autoimmune conditions, and so this work lays the foundation for prioritizing specific antibodies for the treatment of cancer and other diseases."
The researchers found that some unique B cells that changed their genetic sequence after recognizing and targeting cancer cells were present at multiple metastatic tumor sites where the cancer had spread. This means that after recognizing cancer in one area of the body, B cells migrate to hunt cancer in different parts of the body. B cells found in only one tumor site were less likely to change their sequence and did not perform effective cancer surveillance.
The team also found that the B cells present throughout the patients' treatment were the ones that recognized the cancer and changed their genetic sequence, becoming more effective at recognizing cancer.
The researchers used this information to develop a computational tool that predicts which B cells are most likely to successfully detect and target cancer cells.
They believe that their predictive tool could be used to identify the most successful anti-cancer B cells in a patient and artificially engineer the antibodies those B cells naturally produce. This could be used as a personalized immunotherapy that boosts the patient's immune system.
Dr Stephen-John Sammut, first author of the study and head of the Cancer Dynamics Group at the Institute of Cancer Research in London and consultant oncologist at the Royal Marsden Hospital NHS Foundation Trust, said: "When cancer spreads to other parts of the body it is often much more difficult to treat. Our study has shown that the immune response to cancer is not limited to where the tumour initially appears - if an immune B cell successfully detects cancer in one part of the body, it will seek out similar cancer cells in other parts of the body."
"There are currently very few immunotherapies that can be used to treat breast cancer. The computational tool we have developed will allow us to isolate and identify the B cells that have recognised the cancer cells, as well as the antibodies they produce. This will allow us to develop anti-cancer antibodies similar to those produced by B cells, which could then be used as a personalised treatment to boost the immune response against advanced breast cancer."
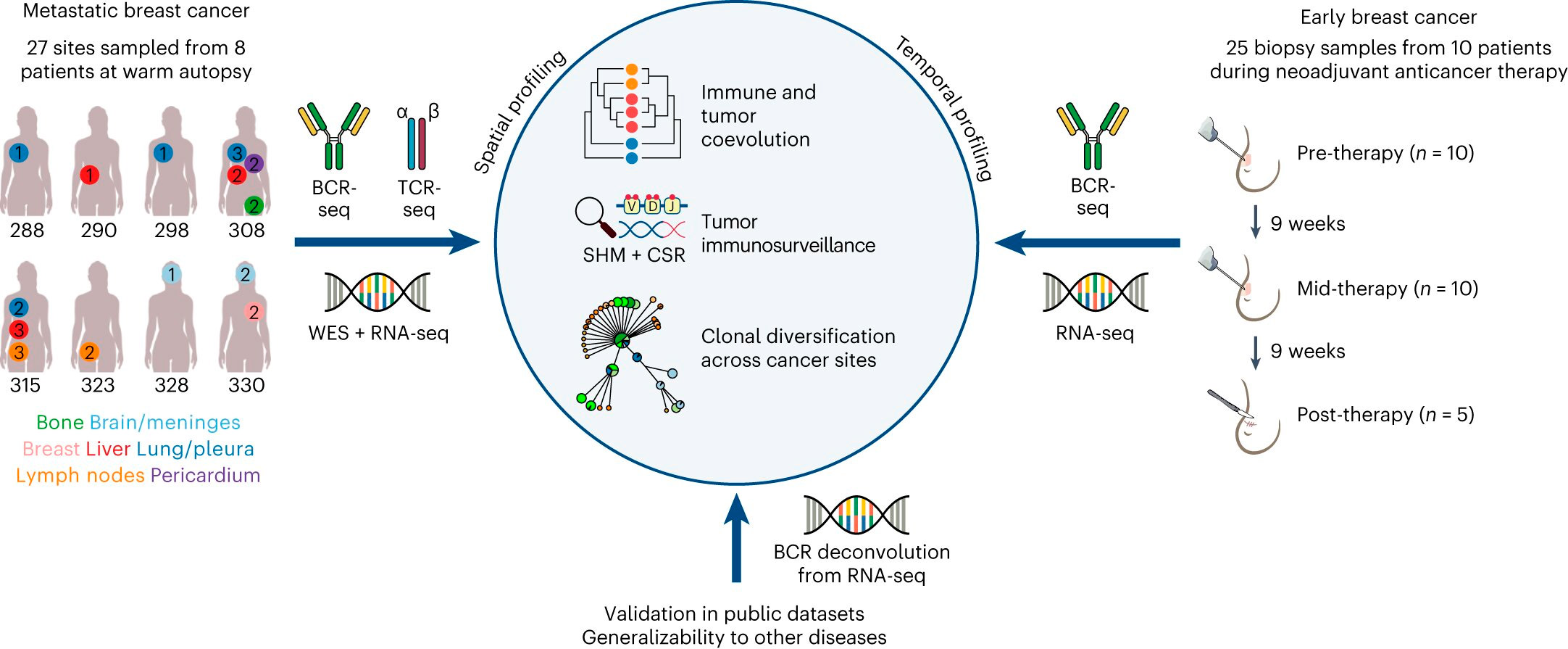
Description of breast cancer cohorts and overview of study design. Source: Nature Immunology (2024). DOI: 10.1038/s41590-024-01821-0
Professor Christian Helin, director general of the Institute of Cancer Research in London, added: "Immunotherapies have changed the outlook for many different types of cancer, but unfortunately they still only work for a minority of patients. We need to better understand how the immune system protects the body from cancer and most research so far has focused on the role of T cells - CAR T cell therapy is the best-known treatment to emerge from this research."
"This study provides exciting insights into the role of B cells during cancer growth and spread, and I look forward to seeing this tool used to focus efforts on developing personalized cancer immunotherapies that can work for many more people than most existing immunotherapies."
