New publications
Medication and group therapy improve control in heroin addiction
Last reviewed: 02.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.

Consistent with their previous research, researchers from the Icahn School of Medicine at Mount Sinai Medical Center showed that people with heroin use disorder showed reduced activity in the anterior and dorsolateral prefrontal cortex (PFC) when performing an impulse inhibition task compared to healthy individuals.
Importantly, 15 weeks of medication-assisted treatment, including adjunctive group therapy, improved impaired anterior and dorsolateral PFC function during an impulse suppression task in a group of participants with heroin use disorder. This suggests a time-dependent recovery of impulse control and PFC function in individuals with heroin use disorder following this intervention.
The study was published in the journal Nature Mental Health.
Opioid overdose deaths (including heroin) continue to rise rapidly among adults. Impulse control—the ability to inhibit unwanted behaviors such as drug use despite significant negative consequences and the desire to quit—is impaired in people with drug addiction, with functional deactivations in the prefrontal cortex, the brain region responsible for self-control processes.
This study recruited 26 inpatients with heroin use disorder undergoing medication-assisted treatment and 24 demographically matched healthy participants for a longitudinal study using functional MRI (fMRI). Participants completed two fMRI sessions 15 weeks apart for inpatients with heroin use disorder and a matched time interval for healthy participants.
During fMRI, participants performed a stop-signal task, a well-validated tool to assess brain function during impulse control. During the task, participants responded to arrow stimuli and withheld their response when the arrow periodically turned red (a stop signal). In addition to increased activity in PFC regions after 15 weeks of inpatient treatment, increased activity correlated with improved performance on the stop-signal task in people with heroin use disorder.
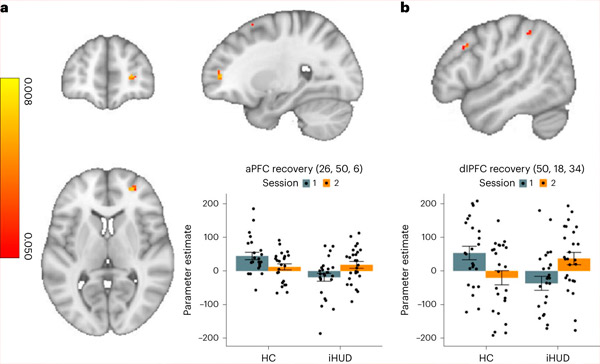
Brain activity responsible for impulse control increases from baseline to follow-up in the iHUD group compared to the HC group. a,b, Activity in the right aPFC (a) and right dlPFC (b) during successful and unsuccessful stops showed a significant increase from baseline to follow-up in the iHUD group compared to the HC group. Source: Nature Mental Health (2024). DOI: 10.1038/s44220-024-00230-4
"Overall, our results identify anterior and dorsolateral PFC regions as potentially amenable to targeted interventions that can accelerate their recovery during impulse control, which may have practical implications for informing future treatments," said Ahmet O. Ceceli, PhD, a senior postdoctoral fellow and lead author of the paper.
"More research is needed to determine whether there is a specific aspect of inpatient treatment that significantly contributes to improvement and to examine other specific factors. For example, our research team plans to test whether the recovery effects we observed in this study are due to the mindfulness-based intervention that was part of an additional group therapy intervention," says Rita Z. Goldstein, PhD, professor of psychiatry and neuroscience at the Icahn School of Medicine at Mount Sinai and senior author of the paper.
