New publications
Lithium Deficiency and the Onset of Alzheimer's Disease: What Was Found and Why It Matters
Last reviewed: 09.08.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
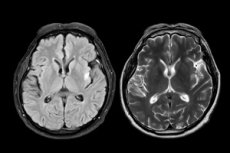
In the brains of mice, a lack of their own lithium (not the lithium in pills, but the stuff that circulates in tiny amounts in the body) accelerates key hallmarks of Alzheimer’s disease—more amyloid and phospho-tau, inflamed microglia and astrocytes, loss of synapses, axons, and myelin, plus memory loss. Replacing this “endo-lithium” with small doses of a special form called lithium orotate prevents and even partially reverses these changes in Alzheimer’s models and in aging, healthy mice. Mechanistically, part of the effect occurs through suppression of the kinase GSK3β, long implicated in the pathogenesis of the disease. The study is published in the journal Nature.
What exactly did the scientists do?
- The mice were depleted of lithium in their diet so that their cortical lithium levels dropped by ~50%. This resulted in accelerated “Alzheimer-like” processes in the animals: amyloid plaques, phospho-tau, neuroinflammation, loss of synapses/myelin, and a decline in cognitive performance. Some of these effects were associated with GSK3β activation.
- They conducted single-nucleus RNA-seq (essentially, they “scanned” gene activity by brain cell types) and saw that with lithium deficiency, transcriptomic shifts in many cell populations overlap with shifts in Alzheimer's.
- They tried lithium orotate (LiO), an organic lithium salt that is less likely to adhere to amyloid than standard lithium carbonate (LiC). At low doses that kept lithium levels in the “natural” range, LiO prevented and/or reversed pathology and memory loss in Alzheimer’s mice and reduced age-related inflammation in normal mice.
Why exactly "orostat"?
There is an old idea: lithium helps with neurodegeneration (it is also a psychiatric drug). In practice, clinical lithium carbonate often runs into two problems:
- Toxicity at pharmacological doses (kidneys, thyroid).
- In brains with amyloid, lithium from carbonate appears to be trapped in plaques and less able to reach the rest of the tissue.
The authors showed physicochemical differences: organic salts (including LiO) have lower conductivity/ionization and bind less to Aβ-oligomers, so they are less likely to “get stuck” in plaques → more lithium is available in unaffected tissue. In microprobe mapping in mice, LiO gave a lower “plaque/non-plaque” ratio and a higher lithium level in healthy fractions of the hippocampus compared to LiC.
What exactly improved in the mice?
- Less amyloid and phospho-tau, more postsynaptic protein PSD-95.
- Better myelin and more oligodendrocytes in the corpus callosum.
- Less activated microglia and astrocytes (Iba1, GFAP), lower levels of proinflammatory cytokines (IL-6, IL-1β).
- Microglia were more active in capturing and utilizing Aβ (both in vivo in old mice and in cell-based assays).
- Memory was restored even when LiO treatment was started at late stages of amyloid pathology (Morris water maze test), without changes in general activity/anxiety.
At the molecular level, LiO decreased GSK3β activity (including the phosphorylated active form) and increased nuclear β-catenin, expected markers of inhibition of the pathway through which lithium may influence tau and plasticity.
How does this relate to people?
- The work shows that lithium homeostasis is no small matter: its disruption may be an early link in the pathogenesis of Alzheimer's (at least in models). Replacement "microdose" therapy with salts that bypass amyloid looks like a promising preventive or therapeutic approach - again: in models.
- Important: this is not about "drinking lithium supplements". Low levels comparable to natural ones worked in mice; safety/efficacy in humans has not been proven. Classic carbonate at therapeutic concentrations is a different dose and risks (kidneys, thyroid), and orotate is a different salt, and its kinetics/safety during long-term use in the elderly population have not been clinically studied.
Limitations and what's next
- This is a mouse study + mouse nuclear sequencing; similar findings need to be confirmed in humans.
- The authors carefully selected the doses and regimens. They cannot be transferred "as is" to the clinic: phase I–III, strict safety monitoring (electrolytes, kidneys, thyroid), and biomarkers of lithium distribution in the brain are needed.
- Interesting questions for the future:
- Is it possible to monitor "brain lithium" non-invasively?
- Does the approach already work for mild cognitive impairment?
- Does it help with other "amyloid" conditions or with post-traumatic microglial changes?
- Are there genetic/metabolic factors that influence lithium homeostasis?
Conclusion
The work gently pushes towards the idea: not only amyloid and tau, but also microscopic shifts in the elemental composition of the brain (lithium!) can significantly change the trajectory of the disease. And if it is possible to restore the “correct” lithium background in a measured and safe manner — especially with salts that do not stick to plaques — this could turn into a new class of Alzheimer’s prevention and therapy. For now, this is a beautiful, proven story on animals — but strong enough to move to people.
