New publications
Immune T cells find allies in astrocytes: new targets for Parkinson's therapy
Last reviewed: 09.08.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
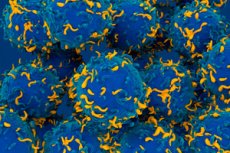
For the first time, scientists have conducted a comprehensive spatial analysis of immune and glial cells in the substantia nigra of brains from people who died from Parkinson's disease (PD) and found a close association between clonally expanded CD8⁺ T cells and pro-inflammatory astrocytes with high levels of the CD44 marker. The work by the Columbia University team was published on August 4, 2025, in Nature Communications.
Why is this important?
In Parkinson's disease, pathological aggregates of α-synoclein accumulate in the substantia nigra and dopaminergic neurons die. The role of immune responses and glia in the progression of the disease is increasingly discussed, but until now there was no clear idea of where exactly and which cells are involved in this inflammatory gathering.
How was the study conducted?
- snRNA-seq (single-molecule nuclear sequencing) provided gene expression profiles in thousands of individual cell nuclei from the substantia nigra.
- Spatial transcriptomics allowed us to superimpose these profiles onto the position of cells in the tissue itself, preserving the architecture of the brain.
- TCR-seq (T-cell receptor sequencing) identified T-lymphocyte clones and their antigen specificity.
Main findings
- Clonal expansion of CD8⁺ T cells. In foci of neurodegeneration, T lymphocytes exhibit limited TCR diversity, indicating their specific response - they are likely directed against α-synoclein peptides.
- Spatial co-localization with CD44⁺ astrocytes. In the same areas where T cells accumulated, the number of astrocytes with high expression of the CD44 receptor increased many times. These glial cells are known as “A1 astrocytes” with a pro-inflammatory profile.
- Functional validation of CD44. In cultured human astrocytes, CRISPR/Cas9 knockdown of CD44 resulted in decreased levels of proinflammatory cytokines and reactive markers, supporting a role for CD44 in supporting neuroinflammation.
Therapeutic perspectives
- Targeting CD44: CD44 blockers or antibodies may attenuate the proinflammatory response of astrocytes and thereby break the “vicious cycle” between T cell infiltration and glial inflammation.
- Immunotherapeutic approaches: Understanding specific T-cell clones may provide the opportunity to develop vaccines or cell-based therapies aimed at rewiring the immune response in the brain.
Conclusion
This study opens a new avenue for Parkinson’s disease therapy by showing that the adaptive immune system and reactive glia do not act in isolation but form pathogenic “units” right at the site of neuronal death. Targeted intervention in these interactions promises to slow the progression of neurodegeneration and alleviate symptoms of the disease.
