New publications
How do abnormal neutrophils help lung cancer spread?
Last reviewed: 02.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Lung cancer remains a leading global health problem, causing the largest number of cancer-related deaths worldwide. Central to its development is the tumour microenvironment, which includes complex interactions with immune cells such as neutrophils. Neutrophils were initially considered beneficial due to their anti-tumour activity in early stages of cancer, but it is now understood that they play a dual role, potentially promoting cancer metastasis under the influence of the tumour environment.
A groundbreaking study from Xuzhou Medical University, detailed in the journal Cancer Biology & Medicine, reveals a new mechanism by which neutrophils accelerate lung cancer progression. This study highlights a key function of neutrophils — typically the first responders to inflammation — as they adopt pro-tumor roles in the cancer microenvironment, significantly influencing the dynamics of cancer metastasis.
The study examines the roles of the PARP-1/Alox5/MMP9 axis in regulating lung cancer-associated neutrophil activation and thereby promoting lung cancer progression. Activated by lung cancer cells, neutrophils interact with PARP-1, which then collaborates with another protein, ALOX5. This interaction is important because it enhances the production of MMP-9, an enzyme vital for breaking down tissue structures and promoting cancer invasion and metastasis.
Using techniques such as immunohistochemistry, the study examines neutrophil infiltration into lung cancer tissue and uses in vitro assays to analyze their effects on lung cancer cell behavior. Downregulation of gene expression and pharmacological inhibition of PARP-1 further elucidate its role in this process.
Confirmed in mouse models, these results show that blocking PARP-1 can significantly reduce tumor growth, illuminating the complex relationship between the immune system and cancer while highlighting that synergistic PARP-1 inhibition may be beneficial for the treatment of lung cancer.
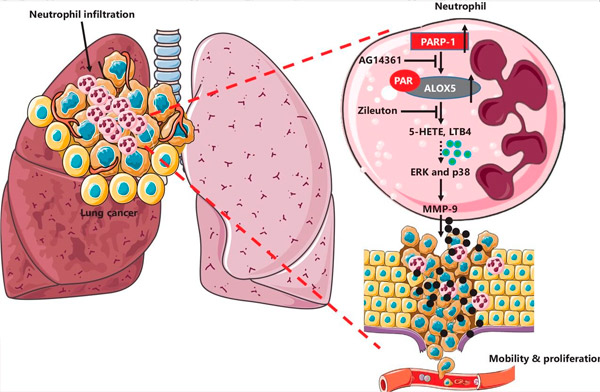
Schematic of the neutrophil-mediated PARP-1-ALOX5 mechanism mediated by MMP-9 in lung cancer. Infiltrated neutrophils are increased in cancer lung tissues and negatively correlate with patient prognosis. Following neutrophil exposure of lung cancer cells, PARP-1 interacts with ALOX5 and enhances protein stabilization via ALOX5 PARillation. Increased ALOX5 metabolites promote MMP-9 production via activation of the ERK and p38 MAPK pathways. Blocking PARP-1 with AG14361 or ALOX5 with Zileuton reduces MMP-9 production and attenuates neutrophil-induced lung cancer progression. Source: Cancer Biology & Medicine (2024). DOI: 10.20892/j.issn.2095-3941.2023.0248
Dr Junnian Zheng, lead author of the study, commented: “This study not only improves our understanding of the biological interactions between lung cancer cells and neutrophils, but also paves the way for new targeted therapies that can interrupt these interactions and potentially improve outcomes for patients.”
These findings have significant implications, suggesting that targeting the PARP-1-ALOX5-MMP-9 pathway may be a promising approach to suppressing neutrophil protumor activity in lung cancer. This strategy may lead to innovative therapies that slow lung cancer progression and enhance the efficacy of current treatments.
