New publications
Double Whammy for Cancer: Manganese Hyperactivates Stress Sensor and Kills Tumors
Last reviewed: 09.08.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Scientists from the Institute of Biophysics of the Chinese Academy of Sciences (CAS), the University of Minnesota and the US National Cancer Institute (NCI), led by Professor Wang Likun, published a study in iScience demonstrating that divalent manganese ions (Mn²⁺) can literally “drive cancer cells to self-destruction” by overactivating the ER stress sensor IRE1α and inducing apoptosis via the RIDD and JNK pathways.
Background: UPR and the role of IRE1α
Protein quality control. Misfolded proteins accumulate within the endoplasmic reticulum (ER) of cells, triggering the “ER stress response” (UPR) via three sensors: IRE1α, PERK, and ATF6.
Dual nature of IRE1α.
- Adaptive activation: moderate ER stress induces XBP1 splicing → restoration of homeostasis.
- Terminal response: Under severe or prolonged stress, IRE1α deactivates the XBP1 branch and instead triggers RIDD- (Regulated IRE1α-Dependent Decay) and JNK-mediated cascades → apoptosis.
This duality has long fascinated oncologists, but the prevailing idea has been to suppress IRE1α to weaken the tumor’s adaptive defenses. The new study suggests the opposite approach: hyperactivating IRE1α.
Experimental protocol and key methods
Cell culture:
Breast cancer (MCF-7), hepatocellular carcinoma (HepG2) and normal control cell lines (HEK293).
Addition of MnCl₂ (0–200 µM) for 24–48 h.
Biochemical verification of IRE1α activation:
IRE1α phosphorylation (Western blot) increased dose-dependently at 50–100 µM Mn²⁺.
RNase activity (RIDD): Decay of target mRNAs (Blos1, Sparc) was measured by qPCR.
JNK pathway: levels of p-JNK and its substrates (c-Jun) increased 2-3-fold.
XBP1s Splicing:
RT-PCR testing showed that Mn²⁺ does not increase the level of the XBP1s splice variant, i.e. it specifically overloads the terminal branch of the UPR.
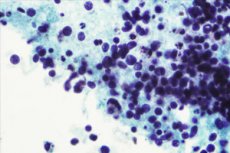
Apoptosis and cell survival:
Flow-cytometry (Annexin V/PI) revealed up to 60% apoptotic cells after 48 h of treatment with 100 µM Mn²⁺;
MTT analysis confirmed a reduction in viability of up to 30% in cancer lines at the same dose, while normal cells retained 80% survival.
Molecular control:
Genetic knockout of IRE1α (CRISPR–Cas9) completely abolished Mn²⁺ cytotoxicity, demonstrating IRE1α dependence.
Administration of small molecule JNK inhibitors (SP600125) reduced apoptosis by approximately 50%, indicating involvement of this branch.
Preclinical in vivo models
Mouse model of breast cancer:
Intratumoral administration of MnCl₂ (1 mM, 20 µL) twice a week for 3 weeks.
Tumor growth: In more than 80% of cases, tumors shrank or stabilized; controls continued to progress.
Toxicity and Safety:
Blood biochemistry (ALT, AST, creatinine) remained within normal limits.
Histology of organs (liver, kidneys, heart) without detected damage.
Expression of apoptotic markers:
Increased activity of caspase-3 and TUNEL-positive cells in tumor sites.
Meaning and Prospects
“We have shown for the first time that selective overactivation of IRE1α with Mn²⁺ reverses the UPR protocol in tumor cells, prioritizing apoptosis,” explains Prof. Wang Likun. “This opens up a new branch of cancer therapy, where instead of suppressing defense pathways, we ‘overload’ them.”
- Contrast agent and oncotherapy? Manganese is already used in MRI contrast agents, which may facilitate rapid translation of therapy.
- Development of Mn²⁺ donors: targeted nanodonors that deliver Mn²⁺ specifically to the tumor, minimizing systemic exposure.
- Combination with immunotherapy: enhanced apoptosis may increase neoantigen production and improve response to checkpoint inhibitors.
The authors emphasize several key points:
A new paradigm for UPR therapy
“We have shown that instead of suppressing the UPR sensor IRE1α, it is possible to achieve an antitumor effect by overactivating it,” says Prof. Wang Likun (CAS). “This opens up a new strategy for cancer therapy based on ‘overloading’ ER stress.”The specificity of the mechanism
“Mn²⁺ selectively stimulates the RIDD and JNK branches of IRE1α without activating the adaptive XBP1s pathway,” notes Dr. Li Chang (NCI). “This ‘biased’ response ensures apoptosis of tumor cells with minimal impact on normal cells.”Prospects for clinical translation
“Since manganese is already used as a contrast agent in MRI, we have every chance to quickly adapt Mn²⁺ donors for the clinic,” comments Prof. Sarah Lee (Minnesota). “The next step is to develop targeted delivery systems to the tumor.”Potential for combination therapy
“Overactivation of IRE1α may enhance neoantigen production and improve the response to immunotherapy,” adds Dr. Tanaka (CAS). “The combination of Mn²⁺ with checkpoint inhibitors promises a synergistic effect.”Safety and Selectivity
“In our preclinical models, Mn²⁺ did not cause damage to normal tissues or increase systemic toxicity,” notes Dr. Martinez (Minn.). “This is critical to moving into clinical trials.”
This study sets a new course for cancer treatment through controlled activation of the cellular stress response and introduces manganese as an antitumor agent capable of overloading cancer cell survival mechanisms.
