New publications
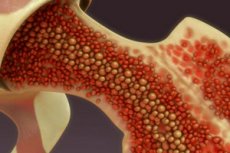
Bone marrow function is dependent on the cardiovascular system
Last reviewed: 02.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
In people suffering from hypertension, atherosclerosis, and also during the post-infarction period, the production of immune cells is activated in the bone marrow.
Immunocytes are formed by stem blood cells that live in the bone marrow. Bone marrow structures react to absolutely all impulses sent to the immune system from various tissues and organs. In this case, hematopoietic cells occupy special places (cells) that have their own microenvironment. The structures that support it also influence the processes of stem cell division, but the activity of these structures themselves is regulated by molecular impulses entering the bone marrow. The nervous system, the state of the intestinal flora, and the functionality of the pancreas also play a role - in particular, in diabetes mellitus, normal immunocytes change the speed of exit from their bone marrow cells and the intensity of entry into the circulatory system.
Scientists from Massachusetts General Hospital have discovered that patients with hypertension, atherosclerosis, andheart attack survivors experience accelerated hematopoiesis – the formation of new blood cells, especially myeloid immune cells. The highest levels are found among leukocytes and neutrophils: they are the first to encounter an infectious agent and initiate the development of an inflammatory response.
Scientists conducted experiments with rodents prone to the pathologies mentioned above: the bone marrow of these animals really began to produce more myeloid immunocytes. In addition, changes were noted in the blood vessels supplying the bone marrow. The number of vessels increased, the vascular walls thickened, and their permeability increased. Due to the increased permeability, more immune cells, previously located in the bone marrow cells, began to enter the blood. As a result, the division of stem cells was activated, and new mature immunocytes appeared.
Experts have traced the entire mechanism of the process. In the post-infarction state, the blood is saturated with vascular endothelial growth factor A, a protein substance that stimulates vascular growth and has a specific receptor that affects cells. Blocking this receptor leads to inhibition of blood vessels in the bone marrow after an infarction. In addition, against the background of atherosclerotic and post-infarction changes in the bloodstream, the content of the signaling immune protein interleukin-6 and versican, a proteoglycan that stimulates hematopoiesis, increases. Today, scientists are studying the origins of these molecular factors that affect bone marrow structures in cardiovascular pathologies.
Time will tell how useful these observations and discoveries will be. Perhaps drugs will be created that block the connection between cardiovascular disease and bone marrow function.
Information is presented on the pages of the NCR publication
