Scientists have discovered a new immunosuppressive mechanism in brain cancer
Last reviewed: 14.06.2024

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Associate Professor Filippo Veglia, Ph.D., and his team at the Wistar Institute have discovered a key mechanism by which glioblastoma—a serious and often fatal brain cancer—suppresses the immune system system so that the tumor can grow without encountering resistance from the body's defense mechanisms.
Their discovery was published in the article "Glucose-driven histone lactylation promotes the immunosuppressive activity of monocyte-derived macrophages in glioblastoma" in Immunity.
“Our research shows that the mechanisms of cancer self-preservation, if sufficiently understood, can be used against the disease very effectively,” said Dr. Veglia.
"I look forward to future research into the mechanisms of metabolic immunosuppression in glioblastoma and hope that we continue to learn more about how to better understand and combat this cancer."
Until now, little has been studied about how monocyte-derived macrophages and microglia create an immunosuppressive tumor microenvironment in glioblastoma.
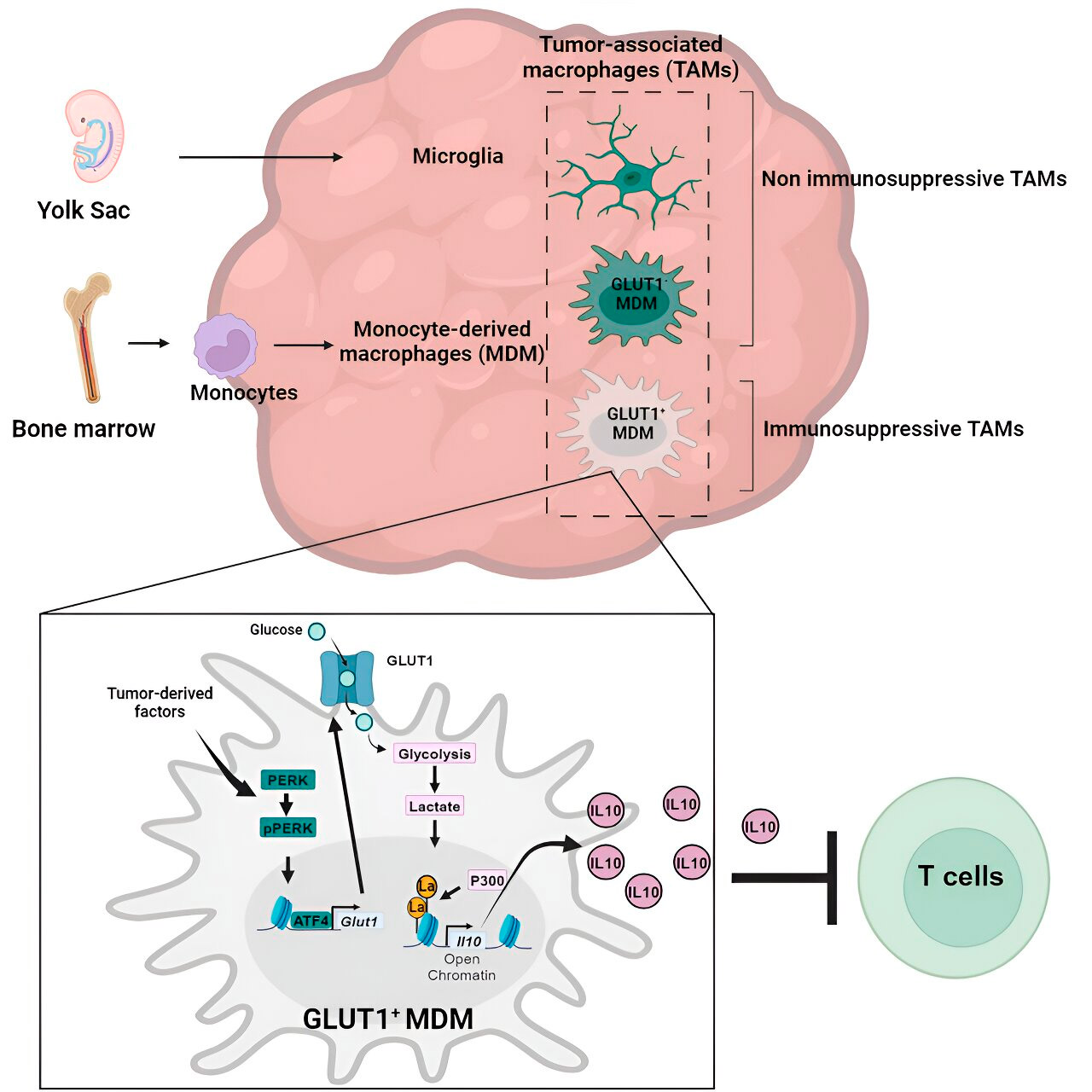
Weglia's laboratory investigated the cellular mechanisms of immunosuppression in glioblastoma and found that as glioblastoma progresses, monocyte-derived macrophages begin to outnumber microglia, indicating that the predominance of monocyte-derived macrophages in the tumor microenvironment is beneficial for the cancer in terms of evading the immune response.
Indeed, monocyte-derived macrophages, but not microglia, blocked the activity of T cells (immune cells that destroy tumor cells) in preclinical models and in patients. The team confirmed this by evaluating preclinical glioblastoma models with artificially reduced numbers of monocyte-derived macrophages.
As expected, models with fewer malignant macrophages in the tumor microenvironment showed improved results compared to standard glioblastoma models.
Glioblastoma accounts for just over half of all malignant tumors that arise in the brain, and the prognosis for patients diagnosed with this disease is extremely poor: only 25% of patients survive the first year after diagnosis. Glioblastoma is dangerous not only because of its location in the brain, but also because of the immunosuppressive tumor microenvironment, which makes glioblastoma resistant to promising immunotherapies.
By programming certain immune cells, such as macrophages (monocyte-derived macrophages and microglia), to work for the tumor rather than against it, glioblastoma creates a tumor microenvironment for itself that allows the cancer to grow aggressively while evading anti-cancer immune responses.
Finding out the mechanism
Having confirmed the role of monocyte-derived macrophages, Weglia's lab next sought to understand exactly how these cancer-associated immune cells work against the immune system.
They sequenced macrophages to determine whether the cells had any abnormal gene expression patterns that might indicate genes that play a role in immunosuppression, and also examined the metabolic patterns of macrophages to understand whether abnormal gene expression was related to metabolism.
Gene and metabolism analysis led them to glucose metabolism. A series of tests showed that monocyte-derived macrophages with increased glucose metabolism and expression of GLUT1, the main glucose transporter, blocked T cell function by releasing interleukin-10 (IL-10).
The team demonstrated that glioblastoma disrupts glucose metabolism in these macrophages, causing them to become immunosuppressive.
Histone lactylation and its role
Researchers have discovered that the key to the immunosuppressive activity of monocyte-derived macrophages associated with glucose metabolism lies in a process called “histone lactylation.” Histones are structural proteins in the genome that play a key role in the expression of genes such as IL-10 in certain contexts.
By rapidly metabolizing glucose, monocyte-derived macrophages produce lactate, a byproduct of glucose metabolism. Histones can become "lactylated" (that is, lactate is integrated into the histones) such that the histone organization promotes the expression of IL-10, which is produced by monocyte-derived macrophages to support cancer cell growth.
Problem solution
But how can you stop the immunosuppressive activity of monocyte-derived macrophages associated with glucose metabolism? Dr. Veglia and his team identified a possible solution: PERK, an enzyme they identified as a regulator of glucose metabolism and GLUT1 expression in macrophages.
In preclinical models of glioblastoma, targeting PERK disrupted histone lactylation and immunosuppressive activity of macrophages, and when combined with immunotherapy, blocked glioblastoma progression and induced long-term immunity that protected the brain from tumor regrowth, suggesting that targeting the PERK-histone lactylation axis can be a viable strategy to combat this deadly brain cancer.
