Bacterial resistance is not always a bad thing
Last reviewed: 07.06.2024

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
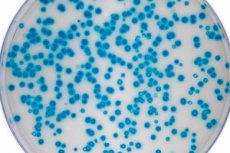
Useful microorganisms with resistance to antibacterial drugs gain a quantitative advantage over pathogenic flora.
Antibiotics are prescribed to suppress the vital activity of bacteria, but the microflora often soon becomes resistant to their action. On the one hand, this is normal: in any living organism, DNA gradually accumulates mutational changes, including in bacteria. Such changes can be negative, neutral or positive, adapting the microorganism to other conditions of existence. If the microflora happens to interact with antibacterial drugs, not all will be able to survive. Only adapted microbes will be able to continue to exist and reproduce, resulting in an antibiotic resistant population.
According to another pathway, microorganisms are able to acquire resistance by selecting the necessary gene modifications from other, already resistant, bacteria. This is horizontal gene transport. Cells interact with each other in complex ways, or remove DNA particles from their surroundings (e.g., from dead cells). In this way, microbes can transfer gene information from different microorganisms.
Of course, it is extremely unfavorable if dangerous bacteria become resistant to an antibiotic. Therefore, scientists do not stop working on the creation of more and more new drugs that can affect the infection with resistance. However, we should not forget that antibiotics affect not only pathogenic, but also useful flora, which can also develop resistance.
Recently, scientists decided to trace how the intestinal microbiome changes in patients with tuberculosis - a disease that requires active intake of antibiotics of different groups. It is worth noting that the quality of human microflora plays an important role not only in digestive processes, but also in the formation of immunity.
In patients with tuberculosis during therapy, symbiotic microorganisms gradually acquired resistance to antimicrobials and their numbers leveled off.
If such microorganisms were transported into rodent organisms and then antibiotics were given to the animals, it is obvious that the bacteria showed almost no reaction: the resistance remained even after transportation. Moreover, the resistant flora gradually began to suppress other flora, including dangerous flora capable of causing pathological processes. In other words, the beneficial bacteria suppressed the development of pathogenic microorganisms.
Indeed, this fact could be used in medicine and in other situations where there is a need to avoid the influence of pathogenic flora. Specialists continue to research and expand the scope of activities in this direction.
Full details are available at sCIENCE.
