New publications
Vitamin D in Multiple Sclerosis: Less Brain Atrophy, No Impact on Relapses
Last reviewed: 18.08.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
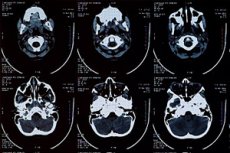
Can a simple supplement slow down the shrinkage of the brain in multiple sclerosis (MS)? Nutrients published a 4-year observational study from Katowice: patients with MS who regularly took vitamin D showed a slower loss of brain volume (according to a number of MRI indicators of atrophy) compared to those who did not take the supplement. As in previous studies, vitamin D did not significantly affect the clinical activity of the disease - relapses, lesions on MRI, progression according to EDSS.
The study was conducted from October 2018 to April 2024 and included 132 adults with MS on stable disease-modifying therapy (DMT). Of these, 97 patients were taking vitamin D (mean ≈2600 IU/day), 35 were not. MRI signs of atrophy were assessed at baseline and after 36 months; relapses, EDSS, new/enlarged T2 lesions, and gadolinium-enhancing lesions were assessed annually.
Background
Multiple sclerosis (MS) is a chronic autoimmune disease of the central nervous system, in which the immune system attacks myelin and axons. At the macro level, this manifests itself as inflammatory foci on MRI and gradual brain atrophy (a decrease in the volume of gray and white matter). It is the rate of atrophy that is today considered one of the best predictors of long-term disability: it reflects not only acute inflammatory "flares", but also cumulative neurodegenerative damage that continues during periods of clinical calm. Disease-modifying drugs (DMTs) are good at suppressing inflammatory activity (relapses, new foci), but they affect atrophy differently - so finding available ways to slow down structural loss remains a priority.
Vitamin D has long been a feature of MS epidemiology: low 25(OH)D levels are more common in people living in high latitudes, and are associated with increased risk of MS onset and greater disease activity. Biologically, this is plausible: the active form of vitamin D “recalibrates” the immune response via the VDR receptor (restrains Th1/Th17, maintains T-regulatory cells and a “calmer” cytokine profile), and is involved in neuroglial homeostasis and remyelination. At the clinical level, the results of interventions are contradictory: randomized trials of supplements often fail to show a significant reduction in relapse rates or the number of new lesions, while observational studies often find a link between maintaining sufficient 25(OH)D and more favorable dynamics of surrogate indicators, including slower atrophy.
Hence the interest in longitudinal studies that look not only at relapses and “focal activity,” but also at structural MRI metrics: ventricular width, intercaudate distance, indices that indirectly reflect shrinkage of the subcortical and periventricular regions. Such simple 2D parameters are available in everyday practice and allow one to detect changes in brain volume over a period of several years—enough to notice a potential “structural effect” of vitamin D, even if classic clinical outcomes do not change.
Finally, an important applied context is safety and realism. Maintaining 25(OH)D levels in the reference range is considered safe at reasonable doses and laboratory monitoring, and is easily combined with current DMT therapy and behavioral measures (insolation, nutrition). If additional “structural” benefit is indeed confirmed in longitudinal data, this gives patients and doctors another, relatively simple lever for protecting brain tissue - not as a replacement for basic therapy, but as an adjuvant neuroprotection strategy. At the same time, RCTs with objective 3D assessments of brain volume and cognitive outcomes remain the gold standard for verification - they should finally answer to whom, in what doses and at what level of 25(OH)D vitamin D provides a clinically significant benefit.
How it was done
- Subjects included: adults with relapsing MS, EDSS ≤6.5, no recent steroids/relapse and no DMT change; recruited at the Neurology Department of the Medical University of Silesia.
- What was measured:
- MR atrophy with simple 2D metrics: frontal horn width of the lateral ventricles (FH), intercaudate distance (CC), third ventricle width (TV), interthalamic distance (IT, mIT), as well as Evans indices (FH/mIT), bicaudate (CC/IT) and FH/CC.
- Annually: recurrences, EDSS, new/enlarged T2 lesions, gadolinium-positive lesions, 25(OH)D level. - Who drank D and how much: 97 out of 132 people. Average dose - 2603 ± 1329 IU/day; groups were comparable in terms of basic characteristics.
What came out at the exit
- Cerebral atrophy: after 36 months, atrophy increased in both groups, but in those not taking the supplement, the growth of the intercaudate distance, the width of the third ventricle and the bicaudate index was significantly greater (p<0.05) - that is, the shrinkage of subcortical structures was faster.
- Disease activity: no statistically significant effect of vitamin D intake on the number of relapses, EDSS dynamics, or focal activity on MRI was found over 4 years of observation. This is consistent with the results of several meta-analyses of RCTs in recent years.
- Levels of 25(OH)D: at the start without supplementation - on average ~21.7 ng/ml, with supplementation - ~41.2 ng/ml. In "non-drinkers" vitamin D gradually increased to optimal values over 4 years (contribution of the sun/recommendations), in "drinkers" it remained stably optimal.
Behind the numbers is another interesting tidbit. People who reported adequate sun exposure were more likely to have sufficient vitamin D levels and, on average, lower EDSS; but when the authors added “sun” as a factor in the longitudinal statistical models, this association was no longer significant, likely due to the influence of other variables.
What does it mean
- Yes: Maintaining 25(OH)D levels within reference ranges in adults with MS is associated with slower brain volume loss as measured by surrogate MRI metrics over 3 years. This is an important “structural” goal.
- No: Vitamin D at routine doses showed no effect on relapse/new lesions/progression of disability over 4 years - and this is consistent with the overall picture of RCTs. Don't expect a "second DMT" from the supplement.
- Practice: In many patients on DMT, 1500-4000 IU/day (depending on baseline, body weight, and geography) is a common tactic under blood 25(OH)D monitoring. Specific goals and doses should be discussed with the treating neurologist. (In the study, the average dose was ~2600 IU/day.)
Restrictions
- Observational design: not randomized; hidden differences between groups and “co-habits” (diet, activity) cannot be excluded.
- Simple MR metrics: 2D indicators (FH, CC, TV and indices) are used, rather than automated 3D segmentation - this makes monitoring cheaper, but is rougher in terms of local changes.
- Attrition over time: some participants dropped out by 36–48 months; the authors took this into account statistically, but residual bias is possible.
Where to look next
- RCTs focusing on atrophy: If structural benefit is confirmed, trials with 3D assessment of gray/white matter volume, cortical thickness and cognitive outcomes are logical.
- Dose personalization: test whether a target 25(OH)D range (say 30-50 ng/mL) provides an optimal benefit/safety balance across different MS phenotypes and DMTs.
- The role of sun and behavior: Objective metrics (light/activity sensors) will help you understand who is winning more - and why.
Conclusion
In the real clinic, vitamin D appears to be a “structure” support rather than an “anti-relapse” agent: it is associated with slower brain atrophy but does not change classic markers of MS activity. Maintain your 25(OH)D levels by testing, without stopping or changing your baseline therapy – and discuss the dose with your neurologist.
Source: Galus W., Winder M., Owczarek AJ, Walawska-Hrycek A., Rzepka M., Kaczmarczyk A., Siuda J., Krzystanek E. Does Vitamin D Supplementation Slow Brain Volume Loss in Multiple Sclerosis? A 4-Year Observational Study. Nutrients. 2025;17(14):2271. https://doi.org/10.3390/nu17142271
