New publications
A surprising link between COVID-19 and cancer regression has been found
Last reviewed: 02.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
A new study led by researchers at Northwestern Medicine's Canning Thoracic Institute and published in the Journal of Clinical Investigation has found a link between COVID-19 infection and cancer regression. The discovery could pave the way for new cancer treatments.
In a surprising turn of events, scientists have discovered that RNA from the SARS-CoV-2 virus, which causes COVID-19, triggers the development of a unique type of immune cell with anti-cancer properties. These cells, called “inducible non-classical monocytes” (I-NCM), attack cancer cells and could be used to treat cancers that are resistant to current therapies.
These findings may explain the mechanism underlying the reported cases of regression of some cancers following COVID-19 infection.
"This discovery opens a new avenue for cancer treatment," said Ankit Bharat, MD, chief of thoracic surgery, the Harold L. and Margaret N. Method Professor of Surgery, and director of the Canning Thoracic Institute, and senior author of the study.
“We found that the same cells activated by severe COVID-19 could be induced by the cancer drug, and in our study we saw a response in melanoma, lung, breast and colon cancer.
Although this is still in the early stages and the effectiveness has only been studied in preclinical animal models, it gives hope that this approach could be used to help patients with advanced cancers that have not responded to other treatments.”
The study, conducted using both human tissue and animal models, has shown that these unique immune cells can be pharmacologically stimulated using small molecules, potentially creating a new therapeutic option for cancer patients. This discovery could have significant implications, particularly for patients with aggressive or advanced cancers who have exhausted traditional treatment options such as immunotherapy.
How the body's response to COVID-19 could help fight cancer
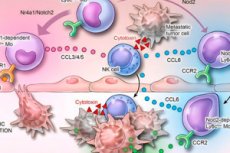
Researchers have found that a special subset of immune cells can be stimulated in the body during COVID-19. This process begins when the virus’s RNA activates certain signals in the immune system. These signals cause regular monocytes (a common type of white blood cell) to transform into I-NCMs. These newly formed cells are able to infiltrate both blood vessels and surrounding tissue where tumors are growing, something most other immune cells cannot do.
"What makes these cells so special is their dual ability," Bharat said. "Normally, immune cells called non-classical monocytes patrol blood vessels looking for threats. But they can't enter the tumor site because they lack specific receptors.
In contrast, I-NCMs created during severe COVID-19 retain a unique receptor called CCR2, which allows them to travel outside of blood vessels and into the tumor environment. Once there, they release certain chemicals, attracting the body's natural killer cells. These killer cells then surround the tumor and begin to directly attack cancer cells, helping to shrink the tumor."
What's next?
Despite the encouraging results, Bharat cautions that more work is needed before this approach can be used in clinical practice.
"We are in the early stages, but there is potential to transform cancer treatment. Our next steps will include clinical trials to see if we can safely and effectively use these discoveries to help cancer patients," Bharat said.
The team hopes that further research will lead to the development of therapies that specifically target these cells to treat difficult-to-treat forms of cancer. This could lead to new treatment options for patients who have exhausted all other options.
The research could play an important role in the Thoracic Institute Canning Double Lung Replacement and Multidisciplinary Care (DREAM) program, a unique clinical initiative at Northwestern Medicine that offers double lung transplants to select patients with advanced lung cancer who have not responded to traditional treatments. To date, more than 40 patients have received double lung transplants through the DREAM program.
"While the program has been very successful, we suspect that some patients may relapse. Because we use monocytes in our study, we may be able to treat DREAM patients without the risk of rejection of the new lungs," Bharat said.
