New publications
Study reveals mechanism of resistance to immunotherapy in glioblastoma patients
Last reviewed: 02.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
A rare, deadly cancer cell is resistant to immunotherapy. Now researchers may have found the reason, which could pave the way for a new type of treatment.
Immunotherapy has become a medical success, allowing doctors to treat and even cure some cancers that were once considered deadly. But this is not true for all cancers. The aggressive brain cancer glioblastoma resists treatment. Until now, researchers did not know why, says one of the scientists involved in the new study from the University of Copenhagen.
"By mutating, i.e. changing their DNA, cancer cells can become resistant to treatment. However, glioblastoma cells behave differently during immunotherapy," says clinical professor and team leader at the Biotechnology Research and Innovation Center (BRIC) Joachim Lütken Weischenfeldt. His new study, published in the journal Neuro-Oncology, describes the response of tumor cells to immunotherapy.
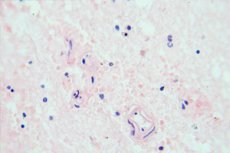
Every year, around 300 Danes are diagnosed with the rare cancer glioblastoma. "By examining and comparing tumor material before and after treatment with immunotherapy, we were able to identify a group of patients in whom the appearance of the tumor cells had changed. The cells had simply put on a different 'coat'," explains Joachim Lütken Weischenfeldt.
Instead of mutating, a process that requires changing a cell's DNA and takes a long time, the tumor cells simply changed their appearance and behavior.
"These cells, which can change their appearance to resemble a particular type of cell found in bone marrow, are extremely plastic," explains Weishenfeldt.
"But it wasn't just the cancer cells that changed. We also saw significant changes in macrophages and T cells, which normally help kill cancer cells."
Untreated cancer cells can usually protect themselves from T cell attack. Immunotherapy prevents this.
"In patients with glioblastoma, immunotherapy did not make the cancer cells unable to defend themselves against T cell attack. Our results show that they can attack T cells with signals and thus 'wear them down,'" Weishenfeldt said.
In other words, glioblastoma cells can evade immunotherapy by changing their appearance, rendering the treatment ineffective, and defend themselves against T-cell attack by exhausting them. This combination makes glioblastoma resistant to immunotherapy and the body’s natural defenses, making it a very aggressive type of cancer.
A Rare But Deadly Cancer " Glioblastoma is the most aggressive type of brain tumor in adults, with short-term survival. We desperately need new, effective treatments," says Weishenfeldt.
He hopes the new research will open the way to new treatments that can combat glioblastoma's unique resistance mechanisms.
"When these tumor cells change their appearance, they express different proteins. And because these proteins will be unique to these cells, it should be possible to target them," he concludes.
This would involve using glioblastoma's clever defense mechanisms against itself. However, it will be some time before such treatments are available to patients.
"Developing a treatment that targets only a specific type of cancer cell is difficult, so it will take time to find the right balance and be able to fight the tumor without serious side effects," explains Weishenfeldt.
The next step for Weischenfeldt and his colleagues will be to try to identify other plastic cancers where treatment failure cannot be entirely explained by genetic mutations.
"Conceptually, this study suggests a different approach to cancer treatment. The idea is to target the plasticity of cancer cells, that is, their ability to change their appearance and interact with surrounding cells, including T cells and macrophages.
"This could be a first step towards more personalised treatments for patients with aggressive cancers such as glioblastoma, for which we desperately need new treatments."
