New publications
Study emphasizes the need for cell type-specific therapies for HIV
Last reviewed: 02.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Researchers at the University of Illinois have demonstrated the importance of targeting specific cell types in treating HIV. Their study, published in the journal Proceedings of the National Academy of Sciences, is one of the first to look at the differential or cell type-specific effects of HIV latency modulation on myeloid cells, a type of immune cell produced in the bone marrow.
One of the main obstacles to eliminating HIV infection is managing latency, or the period during which an infected cell lies dormant and cannot produce virus. Latent HIV cells collect in the body in places known as reservoirs. Latent reservoirs are problematic because they can start producing virus at any time.
Complete eradication of the disease would require the removal of all latent cells from the body or permanent resistance to activation stimuli. However, reactivation can be triggered by a variety of factors, including signals that direct myeloid cell differentiation.
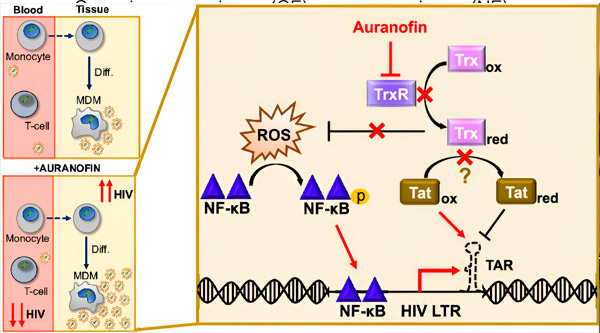
Regulation of HIV latency in monocyte-derived macrophages (MDMs) may pose a risk to viral dissemination. Differentiation of monocytes into macrophages can trigger HIV reactivation, potentially promoting viral dissemination in tissues (top left). A clinical candidate, Auranofin, reduces viral DNA in blood and promotes HIV latency in T cells and monocytes, but causes HIV reactivation in MDMs (bottom left). In MDMs, we hypothesize that inhibition of TrxR by Auranofin leads to accumulation of reactive oxygen species (ROS), which induces NF-κB activation and activation of the HIV LTR promoter (right). Inhibition of TrxR potentially reduces substrate reduction, allowing the Tat protein to remain preferentially oxidized, where it can bind to TAR and initiate HIV transcription. Source: Proceedings of the National Academy of Sciences (2024). DOI: 10.1073/pnas.2313823121
For years, HIV cure research has centered around two approaches known as "shock and kill" and "block and lock." The former works in combination with antiretroviral therapy to activate latently infected cells and kill them through apoptosis, or programmed cell death, while the latter forces infected cells into a deep latent state from which they cannot reactivate on their own.
Research around these techniques has traditionally focused on a type of white blood cell called T cells, which are the primary target of HIV infection. However, latent reservoirs are made up of more than just T cells; in fact, they contain dozens of different cell types, each with its own unique patterns of HIV gene expression.
"There's a huge diversity of cells, even within a single lineage," said Collin Kieffer, an assistant professor of microbiology and an author of the paper. "The variability of the response in these reservoirs increases with each new cell type."
Alexandra Blanco, a graduate student in Kieffer’s lab, wanted to study cell types that had been missed in traditional HIV research. Focusing on myeloid cells, she created a clone library containing 70 populations of latently infected monocytes. Blanco then analyzed the clonal populations and their responses to activation. The responses varied widely, highlighting the great diversity within a single cell type.
This observation raised a new question: do different cell types really have different responses to HIV latency treatments? Indeed, their findings showed that some HIV latency therapies can promote latency in T cells and monocytes, while they can reverse latency in macrophages.
"Not all cells in the body are the same," Kieffer said. "So it makes sense that not all infected cells will respond to the virus in the same way."
Their paper highlights the need for future HIV treatments to consider all cell types and how each cell might respond to potential therapies.
Their findings build on research by Roy Dar, a former Illinois bioengineering professor whose lab studied heterogeneity in HIV gene expression.
"He started it, and we took it over and built it to where it is today," Kieffer said. "So the collaboration really kicked off these results. It's turned into a new direction for our lab, and we're really excited about it."
An additional and unexpected finding from Blanco’s analysis revealed changes in cell size and shape in response to infection, suggesting that HIV can alter cell morphology. Blanco’s next goal is to identify the biological mechanisms underlying these phenotypic changes.
Kieffer and his lab members are also looking forward to reproducing their results, which were mostly done in a cell line, in primary cells. Reproducing the results in a more human-like model would improve the clinical relevance of the study, Kieffer explained.
"We'd like to do larger screens in T cells, monocytes and macrophages to identify potential drugs that might work on all of these cell types," Blanco said. "We might find even more molecules that don't behave in a cell type-specific manner."
