New publications
Stem cells shed light on genetic mechanism of childhood cancer
Last reviewed: 02.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Scientists have made a new discovery in the genetic pathways that drive childhood cancer, opening up new prospects for personalized treatments.
Researchers from the University of Sheffield have created a stem cell model to study the origins of neuroblastoma - a cancer that mainly affects infants and young children.
Neuroblastoma is the most common childhood cancer outside the brain, affecting the lives of approximately 600 children in the European Union and the UK each year.
Until now, studying genetic changes and their role in the initiation of neuroblastoma has been hampered by a lack of suitable laboratory methods. A new model developed by researchers at the University of Sheffield in collaboration with the St. Anna Childhood Cancer Research Institute in Vienna recapitulates the emergence of early neuroblastoma cancer cells, providing insight into the genetic pathways of the disease.
A study published in the journal Nature Communications sheds light on the complex genetic pathways that initiate neuroblastoma. An international research team has discovered that certain mutations in chromosomes 17 and 1, coupled with overactivation of the MYCN gene, play a key role in the development of aggressive neuroblastoma tumors.
Childhood cancers are often diagnosed and discovered at late stages, leaving researchers unaware of the conditions that lead to tumor initiation, which occurs very early in fetal development. Models that replicate the conditions that lead to tumor formation are vital to understanding tumor initiation.
The formation of neuroblastoma usually begins in the womb when a group of normal embryonic cells called " neural crest (NC) stem cells " become mutated and cancerous.
In an interdisciplinary effort led by stem cell expert Dr Ingrid Saldanha from the University of Sheffield's School of Biosciences and computational biologist Dr Luis Montano from the St Anna Childhood Cancer Research Institute in Vienna, the new study has found a way to use human stem cells to grow NC stem cells in petri dishes.
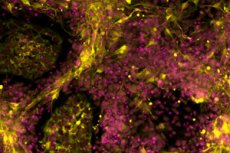
These cells carried genetic changes often seen in aggressive neuroblastoma tumors. Using genomic analysis and advanced imaging techniques, the researchers found that the altered cells began to behave like cancer cells and looked very similar to neuroblastoma cells found in sick children.
These findings provide new hope for the development of personalized treatments that specifically target cancer while minimizing the adverse effects patients experience from existing therapies.
Dr Anestis Tsakiridis, from the University of Sheffield's School of Biosciences and lead author of the study, said: "Our stem cell model mimics the early stages of aggressive neuroblastoma formation, providing invaluable insights into the genetic drivers of this devastating childhood cancer. By replicating the conditions that lead to tumour initiation, we will be able to better understand the mechanisms behind this process and so develop improved treatment strategies in the long term.
"This is very important because survival rates for children with aggressive neuroblastoma are low, and most survivors suffer side effects associated with harsh treatments, which include possible problems with hearing, fertility and lungs."
Dr Florian Halbritter, from St Anne's Childhood Cancer Research Institute and second lead author of the study, said: "This was an impressive team effort that crossed geographical and disciplinary boundaries to make new discoveries in childhood cancer research."
