New publications
"Skin from a syringe": biphasic "granular" bioink printed dermis and implanted it
Last reviewed: 18.08.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
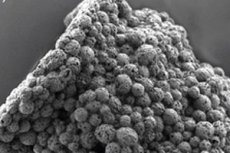
Scientists from Sweden have presented µInk bioink for 3D bioprinting of the dermis: it is a two-phase granular hydrogel based on porous gelatin microspheres with human dermal fibroblasts “planted” on them plus a matrix of hyaluronic acid. The mixture behaves like a liquid under pressure in a syringe/printer nozzle and gels again in a wound - that is why journalists have dubbed it “skin in a syringe”. In experiments on mice, printed structures with a very high cell density survived, quickly built up an extracellular matrix, grew vessels and integrated with tissues in 28 days. The work was published in Advanced Healthcare Materials.
Background
- Why current skin substitutes are far from "true dermis". The clinical standard for large wounds and burns is split-thickness autografts (STSG) and/or dermal templates (e.g. Integra). They save lives and close the defect, but often leave scars and contractures, especially with thin flaps; the quality of the scar depends greatly on the proportion of "deep dermis" in the graft. Even "mesh" flaps, convenient for covering large areas, produce more noticeable scarring due to healing through the mesh cells. Dermal templates help form a "neoderm", but remain acellular, require stages, and do not solve the problem of insufficient autologous cells/vessels in the first weeks.
- Why 3D skin bioprinting is a logical next step, but is being held back by bioink. Printing allows cells and materials to be placed in a targeted manner, but classic homogeneous hydrogels fall into a “fork”:
- too liquid - they spread and do not hold their shape; too rigid - they press on the cells, interfere with the penetration of blood vessels and do not allow printing high cell density. In addition, it is still difficult to recreate adnexal structures (hair follicles, etc.). We need bio-inks that flow under nozzle pressure and then instantly “gather” into a stable porous mass and do not kill cells by shear.
- What are granular (microgel, "jammed") bioinks and why are they suitable for the dermis? These are "densely packed" microgel particles that behave like a solid at rest and like a liquid under shear (shear-thinning) - ideal for syringe/extrusion printing and injections. After application, the string holds its shape, leaving intergranular pores for vascular growth; the mixture can be additionally "cross-linked" with soft chemistry. This class of materials has become the basis for soft tissue printing in recent years.
- The idea of µInk in a nutshell. The authors combined two layers of the problem — cells and matrix: they planted human dermal fibroblasts on porous gelatin microspheres (biocompatible “beads” similar in chemistry to collagen), and then “glued” the granules together with a hyaluronic matrix using copper-free click chemistry. The result was a “liquid under pressure — solid at rest” bioink that allows for ultra-high cellular density, printing/injection, and rapid recruitment of extracellular matrix already in situ. The constructs took root and vascularized in mice within 28 days.
- How this approach addresses the clinic’s “pain points.”
- Speed and logistics: instead of a long cultivation of a tissue equivalent, there is a quick preparation of “live granules” and the introduction of “skin from a syringe” directly into the wound or printing in the shape of the defect.
- Biology: High cellularity + porous architecture → better ECM deposition and neoangiogenesis - key to less scarring and elastic dermis.
- Compatibility with autology: fibroblasts are easily obtained from a small biopsy; gelatin/HA are components familiar to the skin.
- Where the gaps remain. This is all still preclinical in mice; moving to patients requires full-thickness skin models, long-term follow-up, co-printing with keratinocytes/endothelium, GMP standardization, and proof that the technology actually reduces scarring and improves function compared to the standard.
- Why this news is important right now. Against the backdrop of persistent limitations of STSG/templates and the maturity of the granular bioink class, µInk demonstrates a practical assembly: “microgel carriers + soft binding matrix + high doses of autologous cells”. This makes the scenario of rapid, cell-dense dermal reconstruction without lengthy “incubator” stages more realistic.
Why is this necessary?
Classic skin replacements often leave a scar: they have few cells, they grow together poorly and produce a weak “correct” dermal matrix. And growing thick and complex dermis entirely in a dish is long and difficult. The authors propose a different way: quickly assemble “bricks” from the patient’s own fibroblasts, planting them on porous microspheres, and inject/print this directly into the defect area, where the body itself will complete the full-fledged dermis.
How µInk bioink works
- Phase 1: “living granules.” Porous gelatin microspheres (essentially tiny beads, chemically similar to skin collagen) on which primary human dermal fibroblasts are propagated in a bioreactor.
- Phase 2: "Binding Gel". A hyaluronic acid solution that glues the granules together via copper-free click chemistry.
- Rheology. The result is a shear-thinning granular hydrogel: it flows under pressure and holds its shape at rest, which means it is suitable for both syringe application and 3D printing.
What the experiments showed
- Printing and Viability: Stable mini-patches with ultra-high cell density were printed from µInk; fibroblast viability and phenotype were preserved.
- In vivo (mice): Subcutaneously implanted constructs for 28 days
- became overgrown with vessels,
- demonstrated hydrogel remodeling,
- and accumulated dermal ECM (fibroblasts continued to divide and function), indicating tissue integration. - Application practice. The material can be applied through a needle directly into the wound - "skin in a syringe" - or a layer/shape can be printed for a specific defect.
Why is this important?
- Speed and density. Time is critical for burns and chronic wounds. µInk allows you to bypass long cycles of tissue growth "in volume" and immediately introduce many active cells where they are needed.
- Biology closer to normal. The high cellularity and porous architecture of the microspheres encourage matrix production and neovascularization, two keys to scar-free healing and elasticity.
- Clinic logistics. The concept fits well with the autologous approach: take a small skin biopsy → quickly multiply fibroblasts on microspheres → print a transplant for the patient's wound.
How is this different from the usual “hydrogels with cells”
Conventional "homogeneous" hydrogels are either too liquid (spread) or too rigid (press on cells, interfere with vascular growth). Granular architecture provides pores and pathways for vessels, and "two-phase" - both mechanical stability and injectability. Plus, gelatin carriers are biodegradable and "familiar" to tissues.
Limitations and what's next
This is pre-clinical so far (mice, subcutaneous pockets; time frame - 4 weeks). Ahead:
- full thickness skin defects and longer follow-ups;
- keratinocyte/endothelial cell and combination full-thickness skin tests;
- transition to patient autologous cells and burn/chronic wound model;
- scaling for **GMP production** (bioreactors, sterility, click control).
Source: Shamasha R. et al. Biphasic Granular Bioinks for Biofabrication of High Cell Density Constructs for Dermal Regeneration, Advanced Healthcare Materials, online June 12, 2025 https://doi.org/10.1002/adhm.202501430
