New publications
Scientists have grown a unique organoid that mimics the entire brain
Last reviewed: 03.08.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
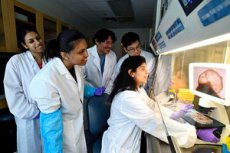
Researchers at Johns Hopkins University have grown a unique human brain organoid containing neural tissue and rudimentary blood vessels. The development could be a breakthrough in the study of neuropsychiatric disorders such as autism.
“We’ve created a next-generation organoid,” said lead author Annie Kathuria, an assistant professor in JHU’s Department of Biomedical Engineering who studies brain development and neuropsychiatric diseases. “Typically, studies create organoids that represent just one part of the brain — the cortex, hindbrain, or midbrain. We were able to grow a rudimentary whole-brain organoid that we call a multi-regional brain organoid (MRBO).”
The work, published in the journal Advanced Science, is one of the first times scientists have created an organoid that includes tissue from all major brain regions interacting with each other. This is especially important for studying diseases that affect the entire brain, such as schizophrenia or autism. Until now, such studies have mainly been conducted on animal models.
To grow MRBO, Kathuria’s team first cultured neural cells from different parts of the brain, as well as rudimentary blood vessels, in separate dishes. They then connected these parts using special “glue” proteins, allowing the tissues to grow together and communicate. As the organoid grew, electrical signals began to emerge, indicating neural network activity.
The organoid created included a wide range of neuronal cells similar to those in the brain of a human embryo on the 40th day of development. The laboratory-created mini-brain structure managed to reproduce approximately 80% of the cell types characteristic of the early stage of human brain development.
Although the MRBO is significantly smaller than the real brain (about 6-7 million neurons versus tens of billions in an adult), it provides a unique platform for studying the development of the brain as a whole.
The organoid also showed an early form of the blood-brain barrier, a layer of cells that controls the passage of substances into the brain.
“If we want to understand neurodevelopmental disorders or psychiatric illnesses, we need to work with human cells. But I can’t just ask someone to ‘lend’ me their brain to study autism,” Kathuria explains. “Whole-brain organoids allow us to observe disease progression in real time, test treatments, and even develop customized therapies.”
Scientists note that using such organoids to test new drugs could improve the efficiency of clinical trials. Today, 85% to 90% of drugs fail phase I human trials, and for neuropsychiatric drugs the failure rate is even higher — up to 96%. This is because animal models are mostly used in the early stages of development, while MRBO better reproduces human brain development and can serve as a more accurate model.
“Schizophrenia, autism and Alzheimer’s disease affect the entire brain, not just specific regions,” Kathuria says. “If we can understand what’s going wrong at the earliest stages of development, we can find new targets for therapy and drug development. We can test drugs directly in these organoids and assess their effectiveness before they reach human clinical trials.”
