New publications
Scientists discover key genetic factors underlying testicular cancer
Last reviewed: 02.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Scientists have identified new genetic defects and evolutionary patterns that contribute to the development of testicular cancer. Their findings provide insight into how the disease develops and potential treatment strategies.
Testicular cancer accounts for only about 1% of all cancers in men, but is the most common cancer among men aged 15 to 44. Around 200 men are diagnosed with testicular cancer in Ireland each year, and there has been an increase in the incidence in recent years - a trend also seen in northern and central Europe.
Fortunately, testicular cancer is highly treatable, especially when detected early, with survival rates exceeding 90%. However, patients at the highest risk have a significantly worse prognosis: the survival rate is only about 50% despite extensive clinical trials, and existing chemotherapy treatments come with significant toxicity and side effects.
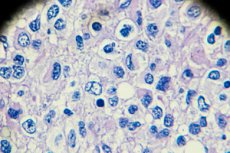
Using data from the 100,000 Genomes Project, led by Genomics England and NHS England, the scientists applied whole genome sequencing (WGS) to 60 patient samples to answer important biological and clinical questions about testicular germ cell tumours (TGCTs). The findings have been published in the leading international journal Nature Communications.
Key discoveries include:
- Novel potential drivers of testicular cancer, including subtype-specific drivers that may aid in stratifying patients based on their tumor characteristics.
- Reconstruction of evolutionary trajectories of genome changes and probable pathways of TGCT progression.
- Discovery of a broader spectrum of mutational signatures associated with TGCT. These characteristic patterns of DNA damage may reflect various carcinogenic exposures (e.g., smoking, UV radiation) and allow retrospective assessment of risk associated with exposure to these factors.
- Previously unidentified recurrent mutational hotspots in testicular cancer.
- Identification of a unique genomic immune mechanism for TGCT, predominantly in seminomas, the most common tumor type.
"We have made a significant step forward in our understanding of how this disease progresses and have gained important insights into potential treatment strategies, which is clearly key to improving outcomes for patients," said first author Moira Ni Lethlobair, an associate professor in the School of Genetics and Microbiology at Trinity College Dublin.
"Importantly, this study was made possible by the valuable contribution of tissue samples provided by the 100,000 Genomes Project and the collaborative efforts of NHS healthcare professionals. It is one of the first relatively large-scale studies of the testicular cancer landscape to use the powerful technique of whole genome sequencing, which has been key to uncovering new data not available using other methods," added Ní Lethlobair.
The study aims to turn genomic data into meaningful patient outcomes by linking fundamental discoveries with applied medical applications. It is also an example of how large volumes of data and patient samples can give us a more detailed understanding of disease.
The study was a collaborative effort led by senior authors Professors Matthew Murray, Andrew Prothero, Claire Verrill and David Wedge, and involved a team of researchers, clinicians and trainees from academia and the NHS, with contributions from Trinity College, the University of Oxford, the University of Cambridge and the University of Manchester.
To further deepen their understanding of the disease, the researchers hope to enroll more participants to account for the diversity of outcomes, ethnicities and types of testicular cancer.
