New publications
Scientists have described how cells are activated to cause fibrosis and scarring of organs
Last reviewed: 02.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
A new study by Unity Health Toronto, which examines how fibroblast cells in the body are activated to cause fibrosis and organ scarring, was published in the journal Nature Reviews Molecular Cell Biology. Fibrosis and organ scarring are a leading cause of death, with evidence suggesting they are responsible for up to 45% of deaths in developed countries.
Fibrosis is a process in which fibroblast cells in our body produce excess amounts of a protein complex called the extracellular matrix (ECM). The ECM contains proteins such as collagen, elastin, and fibronectin, and can be thought of as a kind of body-wide “glue” that connects the various organs of our body, maintaining their boundaries.
Normally, fibroblasts produce ECM to support tissue structure and to help repair damaged or injured tissue. For example, under normal circumstances, when you get a cut, fibroblasts move to the site of the cut or wound, multiply, and produce ECM to help heal the wound. In fibrosis, however, fibroblasts receive certain signals that activate them to overproduce ECM.
This excess ECM, especially excess collagen, can lead to scar tissue formation, which can impair organ function. Fibrosis can occur in any tissue or organ in the body, including the lungs, liver, kidneys, and heart, and is associated with many common diseases, often in their late stages.
A new study summarizes some of the signals and molecular mechanisms that play a role in activating fibroblasts to overproduce ECM. The researchers also discuss the heterogeneity of fibroblasts and how their greater heterogeneity may impact the healing process.
"This review attempts to unravel some of our knowledge and understanding - or misunderstanding - of fibroblasts and their activation," said Dr Boris Hinz, study author and scientist at the Keenan Centre for Biomedical Science at St Michael's Hospital.
"We usually talk about fibroblasts being activated from a dormant state in normal healing and fibrosis. But the cells that were activated to make new ECM were not truly dormant, and not all of them were fibroblasts," Hinz said. "We wanted to understand exactly which cells were being activated. What types of activations were happening — like, 'What are the key signals that are activating these fibroblasts and how?'"

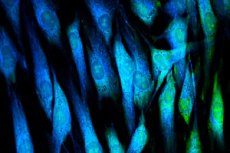
Nuclear mechanotransduction and myofibroblast memory. Source: Nature Reviews Molecular Cell Biology (2024). DOI: 10.1038/s41580-024-00716-0
Fibroblasts Remain 'On' Graduate student Fereshteh Sadat Younesi helped conduct the review. Younesi is a member of the Hintz lab and a student at the St. Michael's Research Training Center.
"One of the key signals comes from mechanical stress in the compacted environment of fibrotic areas. When tissues undergo fibrosis, they become much stiffer than normal because of these fibroblasts that start overproducing and reorganizing the ECM," Younesi said.
"These fibroblasts sense the stiffness around them, which keeps them 'on' even after the initial injury has healed. These mechanically induced fibroblasts aggravate the fibrotic area with their constant activity."
Hinz said that once researchers better understand the signals and mechanisms involved in fibroblast activation, they may be able to develop therapies and interventions to interrupt this process and stop the overproduction of ECM, thus stopping fibrosis.
"We need a way to cure fibrosis. Scientists have known about fibrosis for about a century, and there is still no cure," Hinz said. "With only two drugs currently approved, we can stop fibrosis in some organs — at best. The ultimate goal would be to 'instruct' the scar-making cells to remove excess ECM with pharmaceutical guidance. That's where science is heading, and that's the ultimate dream."
