New publications
"Oxygen for cells": a simple implant helped to lower sugar levels without strong drugs
Last reviewed: 18.08.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
A new “oxygen” implant for the treatment of type 1 diabetes was described in Nature Communications: a compact electrochemical oxygen generator (iEOG) continuously supplies O₂ to a macrocapsule with insulin-secreting cells. This system allows for tight packing of isolated islets (up to 60,000 IEQ/ml) and maintains their viability and secretion even in low oxygen conditions. In rats with diabetes, the device implanted under the skin maintained normal sugar for up to three months — without immunosuppression. Control rats, without oxygen, remained hyperglycemic.
Background
- The main technical problem is oxygen. As soon as we “hide” the cells behind the membrane and put the device under the skin (conveniently and easily extracted), they lack oxygen: diffusion through the membrane and the poorly vascular place does not meet the needs of the “voracious” islets. Hence the early death, weak work and the need to greatly thin out the seeding - otherwise the capsule turns out to be huge.
- Why is it so physically difficult? Oxygen passes through tissues only for very short distances, and encapsulated cells do not have their own vessels - for the first months they live only due to passive diffusion. Any thickening of materials or "compaction" of cells quickly transfers the center of the capsule to hypoxia.
- What have you tried before?
- They made oxygen-refillable macrodevices (for example, βAir): there is a reservoir inside that is replenished with oxygen daily; there were preclinical and early clinical trials. It works, but it is labor-intensive for the patient.
- Chemical O₂ donors and "carrier" materials (perfluoro compounds) were tried: they help, but give a short and difficult to control effect. "Air" frames for accelerating O₂ delivery into the thickness of the gel also appeared.
- The capsules themselves and the implantation sites (thin membranes, prevascularization) were improved, but without an external source of O₂ they still run up against the cell density limits.
- What gap in the puzzle does the new work fill? The authors of Nature Communications show a continuous supply of oxygen from a mini-generator right inside the macroencapsulation system: the device takes water from the tissues and electrochemically releases O₂, which evenly “breathes” along the capsule with cells. The idea is to give the capsule its “own aquarium compressor” so that it can pack more cells and still keep them alive and working – even in a subcutaneous, not very “oxygenated” place.
Why is this necessary at all?
Islet or beta cell transplantation is one of the most promising avenues to a “functional cure” for type 1 diabetes. But there are two major barriers:
- Immunity - usually requires lifelong immunosuppressants;
- Oxygen starvation - capsules that shield the immune system simultaneously cut off cells from vessels, and beta cells, voracious for O₂, quickly "suffocate". The new work hits the second barrier: it gives the capsule its own, controlled source of oxygen.
How the implant works
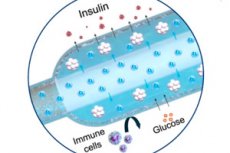
- Two parts. In a titanium case there is a mini-oxygen generator (iEOG), which extracts water from the interstitial fluid and releases O₂ by electrolysis; next to it there is a thin linear capsule with cells (similar to a long "sausage"), through which a gas-permeable tube passes: oxygen is evenly absorbed along the entire capsule. Between the cells and tissues there is a semi-permeable membrane (electrospin + alginate): glucose and insulin pass through, immune cells do not.
- Dimensions: The second version of iEOG is 13 mm in diameter and 3.1 mm thick, weighing about 2 g. When paired with a capsule, such a system can be inserted and removed through a small incision, which is important for safety.
- Productivity. The generator produces ~1.9–2.3 cm³ O₂/h and maintains the specified flow for months and even years (in long-term tests in a saline solution — up to 2.5 years), and after implantation in rats, this level was maintained. Such a flow is calculated to cover the needs of hundreds of thousands of islet equivalents — the order of magnitude that a person needs.
What the experiments showed
- In vitro: At 1% O₂ (severe hypoxia), oxygenation maintained viability and secretion in INS-1 aggregates and in human islets packed in a very dense layer (60,000 IEQ/mL).
- In vivo (rats). After subcutaneous implantation in an allogeneic diabetes model, the iEOG system normalized glycemia for up to 3 months without immunosuppression; devices without oxygen had no effect. Histology around the generator showed no significant adverse reactions.
Why is this important for the clinic?
- A step towards “realistic dimensions”. To provide an adult with a dose of 300–770 thousand IEQ, the capsule must be tightly packed – this has always been limited by oxygen. Controlled O₂ supply “removes the ceiling” on density and gives a chance to make the device compact enough for real implantation.
- Plus convenience. Previously, we tried chemical oxygen donors (peroxides) - they do not work for long and are uncontrollable, as well as O₂ reservoirs with daily "refilling" through the skin - cumbersome and inconvenient. Here, oxygen is supplied constantly and in measured doses, without injections.
Technical details that impress
- The source of water is tissue. iEOG takes in the vapor of interstitial fluid through a porous “window”, and then a classic membrane-electrode assembly (MEA) and a voltage of 1.4–1.8 V are used to separate water into H₂ and O₂; gases are removed through different channels.
- Durability. Three devices in saline solution operated for 11 months, 2 years, and 2.5 years on direct current without degradation by oxygen flow; after implantation in immunodeficient and immunocompetent rats, performance was maintained.
Limitations and "what next"
This is still pre-clinical: rats, high density in the capsule, oxygen supply - everything is great, but key tests are ahead:
- scaling to human doses and timeframes;
- reliability and power supply of electrochemists in the human body for years (the power supply architecture is not detailed in the article);
- minimization of fibrosis around the capsules and diffusion stability;
- testing on beta stem cells and in models closer to humans. The authors openly compare their solution with previous approaches and position it as a platform for clinically translatable capsules.
Conclusion
In order for transplanted beta cells to live and function without immunosuppressants, they need to breathe. The Cornell and partners team showed that a mini-oxygen generator built into a linear capsule can “feed” cells with O₂ long enough and evenly enough for them to withstand high density and reduce sugar even in a subcutaneous location. The clinic is still a long way off, but the engineering logic is simple and beautiful — give cells air where it’s lacking.
