New publications
"One Molecule Instead of Two": Tongkat Ali Produces Double-Action Gout Drug Prototype
Last reviewed: 18.08.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
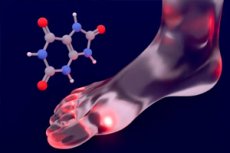
Scientists have come up with a rare thing for gout therapy: a single molecule that both reduces uric acid levels and dampens joint inflammation. The researchers didn’t start from scratch — the starting point was a natural component from the Eurycoma longifolia plant (also known as “tongkat ali”). After phenotypic screening and multi-round structure optimization, the team synthesized 64 derivatives and derived candidate number 32, which showed efficacy in preclinical models at the level of the best drugs, but with a more favorable safety profile. The article was published in Nature Communications on August 12, 2025.
Background of the study
Globally, gout was estimated to affect ~56 million people in 2020; prevalence and incidence have been increasing in recent decades. The disease is more common in men and the elderly and is closely associated with metabolic comorbidities.
- Key biology: NLRP3 → IL-1β. The attack is triggered by monosodium urate crystals in the joint: they activate the NLRP3 inflammasome, which leads to the release of IL-1β and powerful neutrophilic inflammation. Therefore, NLRP3 is one of the main anti-inflammatory targets in gout.
- Two lines of therapy today. (1) Long-term reduction of uric acid: xanthine oxidase inhibitors (allopurinol, febuxostat) and uricosurics (URAT1 inhibitors, etc.). (2) Relief of attacks: NSAIDs, colchicine, GCS; ACR-2020 recommends “treat-to-target” <6 mg/dL. But often several drugs are required at once.
- Why uricosurics are important. Most of the urate after glomerular filtration is reabsorbed in the proximal tubule - mainly via the URAT1 and GLUT9 transporters; OAT4, ABCG2, etc. are also involved. Blockade of these pathways increases urate excretion.
- Limitations of existing agents. The uricosuric lesinurad had dose-dependent renal AEs; the drug was eventually withdrawn from the US (2019) and EU (2020) markets. For febuxostat, after warning signs in older studies, the newer FAST-trial showed no increase in overall mortality vs allopurinol - the debate about the safety profile continues.
- The logic of “two targets in one molecule.” The ideal is an agent that simultaneously lowers urate (via URAT1/GLUT9/OAT4) and dampens inflammation (via NLRP3). This could reduce polypharmacy and drug interactions. Until now, such “polypharmacological” candidates have been rare.
- Why Eurycoma longifolia (Tongkat Ali)? This plant is known for its diverse pharmacological activity; for gout, it has been described as having a urate-lowering effect in animals and inhibiting urate transport (URAT1) by individual components - a good source of "natural skeletons" for design.
- What the current work adds. The authors in Nature Communications (August 12, 2025) took β-carboline-1-propionic acid from E. longifolia and created 64 derivatives through phenotypic screening/structural optimization. The lead candidate, compound 32, showed uric acid reduction in mice (similar to febuxostat, better than lesinurad/benzbromarone) and suppression of NLRP3-dependent inflammation in an acute arthritis model — that is, exactly the desired “dual mechanism.”
What did they do?
The authors took β-carboline-1-propionic acid from E. longifolia and designed a series of derivatives with a “dual” pharmacophore: simultaneously hitting uric acid transporters in the kidneys (to speed up its excretion) and the NLRP3 inflammasome (a key trigger of inflammation in gout). As a result, compound 32 became the leader: it suppresses urate reabsorption through URAT1, GLUT9 and OAT4 (i.e., it works as a powerful uricosuric) and simultaneously inhibits NLRP3 activation, reducing the release of IL-1β, the main “mediator” of a painful attack.
Results in models
- In mouse models of hyperuricemia, the candidate reduced uric acid comparable to febuxostat and significantly better than lesinurad and benzbromarone; however, in tests on individual targets, the IC₅₀ for URAT1 for “32” was half that of lesinurad (3.81 vs. 6.88 μM).
- In a rat model of acute gouty arthritis, the drug reduced NLRP3-mediated inflammation.
- Safety: negative hERG cardiotoxicity tests, oral bioavailability in rats of ~53%, tolerance of doses above 1000 mg/kg in mice, and no organ damage with long-term high-dose administration. This is better than control drugs known to have problematic profiles.
Why is this important?
Today's gout therapy is usually divided into two directions:
- Long-term reduction of uric acid (xanthine oxidase inhibitors such as allopurinol or febuxostat, and uricosurics such as URAT1 inhibitors).
- Relief of attacks (NSAIDs, colchicine, steroids).
But the classic drugs have their downsides: febuxostat and allopurinol have side effects and are poor in acute attacks; lesinurad had warnings about nephrotoxicity, which is why it was eventually withdrawn from some markets. So a single molecule that simultaneously removes urate and blocks the NLRP3 inflammatory cascade is a potential way to reduce polypharmacy, drug interactions, and toxicity.
A little context: what are these targets?
- URAT1/GLUT9/OAT4 are the main transport proteins responsible for the reabsorption of uric acid in the kidneys; their blockade increases urate excretion.
- The NLRP3 inflammasome is an intracellular “signaling node” that, when exposed to monosodium urate crystals, triggers an inflammatory cascade and the release of IL-1β; this is what makes a gout attack so violent.
Limitations and what's next
It is important to emphasize that all results are still preclinical (mice and rats). Tolerability and efficacy in humans have yet to be tested in phases I–III clinical trials, including assessment of the effect on the kidneys and cardiovascular risks in patients with comorbidity, which is common in gout. Nevertheless, the work sets a new strategy – rationally designed polypharmacology based on natural skeletons – and adds a promising candidate for further development to the “portfolio”.
Source: Nature Communications, August 12, 2025: Discovery of multi-target anti-gout agents from Eurycoma longifolia Jack through phenotypic screening and structural optimization.
